Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Research Article - Open Access, Volume 5
Risk of postpartum hemorrhage in an ethnic minority region: Prediction results based on iterative machine learning
Jun-Yu Pan1; Ling Wang1*; Kai-Feng Liu1; Sheng-Yun Xie2
1Intensive Care Unit, People’s Hospital of Qiandongnan Miao and Dong Autonomous Prefecture, Kaili 556000, Guizhou, China.
2Obstetrics, People’s Hospital of Qiandongnan Miao and Dong Autonomous Prefecture, Kaili 556000, Guizhou, China.
*Corresponding Author : Ling Wang
Intensive Care Unit, People’s Hospital of
Qiandongnan Miao and Dong Autonomous
Prefecture, Kaili 556000, Guizhou, China.
Email: 463082910@qq.com
Received : Nov 10, 2024
Accepted : Dec 03, 2024
Published : Dec 10, 2024
Archived : www.jcimcr.org
Copyright : © Ling W (2024).
Abstract
Purpose: To develop a predictive model for Postpartum Hemorrhage (PPH) in a minority region of China (Qiandongnan Miao and Dong Autonomous Prefecture).
Methods: A retrospective study was conducted using data from 23,490 hospitalized patients. Employing machine learning techniques, a multilayer perceptron neural network model was built to identify significant risk factors affecting PPH.
Results: Among 23,490 hospitalized patients, 1,050 cases experienced PPH, yielding an incidence rate of 4.47%. Significant risk factors contributing to PPH included placental implantation, anterior placenta, retained placenta, placental abruption collectively contributing over 70% of the variance. The model achieved accuracies of 95.3% on the training set and 95.4% on the test set.
Conclusion: The neural network model demonstrated excellent predictive efficacy for PPH. Clinicians should prioritize these critical risk factors to identify patients who are at a high risk of PPH prenatally.
Keywords: Postpartum hemorrhage; Risk factor; Prediction model; Ethnicity; Minority region.
Citation: Jun-Yu P, Ling W, Kai-Feng L, Sheng-Yun X. Risk of postpartum hemorrhage in an ethnic minority region: Prediction results based on iterative machine learning. J Clin Images Med Case Rep. 2024; 5(12): 3379.
Introduction
Postpartum Hemorrhage (PPH) is a critical obstetric complication. Its incidence increases year-on-year based on factors such as age, miscarriage, and placental implantation [1-3]. PPH poses a serious threat to maternal life, with numerous studies highlighting it as the primary cause of maternal mortality [1-4]. Consequently, global efforts by governments and healthcare institutions have been directed toward preventing PPH and reducing maternal mortality [5]. PPH has a multifactorial etiology, and its occurrence can be influenced by factors such as race, geographic location, socioeconomic status, cultural differences, healthcare infrastructure, and prenatal care. These factors contribute to significant variations in the incidence and treatment outcomes among different regions and ethnic groups [6,7]. Clinically, it is essential to identify patients who are at a high risk of PPH and to develop emergency measures [8]. The Qiandongnan Miao and Dong Autonomous Prefecture is located in southwestern China, with a total population of 4.88 million. The primary ethnic groups are the Miao and Dong, with these ethnic minorities accounting for as much as 81.7% of the population. The region boasts a rich cultural heritage with abundant historical and diverse ethnic cultural legacies. Treatment choices for pregnant women are collectively influenced by ethnicity, culture, and economics. The present study aims to utilize iterative machine learning methods to identify key risk factors for PPH in a specific ethnic minority region of China (Qiandongnan Miao and Dong Autonomous Prefecture). The objective is to develop a predictive model for the prenatal assessment and identification of women who are at a high risk of PPH in this region.
Materials and methods
The study adhered to the ethical principles outlined in the revised 2013 Declaration of Helsinki 1975 and followed the STROBE guidelines for reporting observational studies [9]. We adopted a retrospective research method and expected to collect 960 cases.
Study population
This study included patients admitted to the People’s Hospital of Qiandongnan Miao and Dong Autonomous Prefecture’s obstetrics and intensive care units between January 1, 2018, and December 31, 2023 (continuous case selection). Pregnancy duration was longer than 28 weeks. Overall, 23,490 patients were identified, including 1,050 patients with PPH (4.47%) and 22,440 patients without PPH. The average age of the patients was 31.11±5.59 years, with an age range of 16-48 years. Among them, 13,525 patients underwent cesarean section (57.58%), and 9,965 patients had vaginal delivery. There were 529 patients admitted to the intensive care unit (2.25%), with a total of five deaths (0.02%).
PPH diagnostic criteria
The diagnostic criteria for PPH were as follows: clinical signs of PPH, with a hemorrhage volume exceeding 500 mL for vaginal deliveries and 1000 mL for cesarean section deliveries.
Treatment modalities
The hospitals used proactive treatment measures to address complications, closely monitor patients, and implement necessary organ function support therapy to maintain the stability of patients’ vital signs. Postpartum management involved intravenous oxytocin infusion (dosage: 0.02-0.04 units per minute). For all patients, 10 units of oxytocin were administered intramuscularly after placental expulsion. In patients with continued bleeding, 1 g tranexamic acid was infused intravenously along with transfusion therapy. If conservative treatment failed, uterine artery embolization was performed. In patients in whom bleeding persisted after embolization, or severe intraoperative or post-operative hemorrhage resulted in profound shock necessitating life-saving hysterectomy, hysterectomy was performed. Patients experiencing hemodynamic instability or organ dysfunction were admitted to the intensive care unit for monitoring.
Observational indicators
According to the diagnostic criteria for PPH, patients were categorized into the PPH and non-PPH groups. The relevant data were extracted from the patients’ health records after discharge, including age, assisted reproductive technology, number of pregnancies, parturition number, macrosomia, twins, history of cesarean section, history of adverse obstetric or perinatal events, non-vertex presentation, and stillbirth. Moreover, uterine fibroids, anterior placenta, umbilical cord around the neck, preexisting hypertension before pregnancy, pregnancy-induced hypertension, pre-eclampsia, and HELLP (Hemolysis, Elevated Liver enzymes, and Low Platelets) syndrome were assessed. Furthermore, gestational diabetes mellitus, diabetes mellitus before pregnancy, hepatitis B, Peripartum cardiomy- opathy, history of pelvic inflammatory disease, history of vaginitis, Peripartum sepsis, history of uterine cavity infection, thrombocytopenia were evaluated. Other items of interest included polyhydramnios, oligohydramnios, post-term pregnancy, intrahepatic cholestasis of pregnancy, induced abortion, premature birth, premature membrane rupture, placental abruption, uterine atony, retained placenta, placental implantation, and placental adhesion.
Statistical methods
Data processing was performed using SPSS 26.0 statistical software. Categorical data were analyzed using the χ2 test, and presented as n (%). Continuous data are presented as the mean ± standard deviation, and intergroup comparisons were performed using the independent-samples t-test. The model was established using a multilayer perceptron neural network. P<0.05 was considered statistically significant.
Results
Analysis of Factors Related to PPH. The proportions of patients with advanced age, high number of pregnancies and deliveries, twin pregnancies, an adverse pregnancy history, non-vertex presentation, placenta previa, nuchal cord, pre-eclampsia, gestational diabetes mellitus, pelvic inflammatory disease history, intrauterine infection history, thrombocytopenia, polyhydramnios, preterm birth, miscarriage, premature membrane rupture, placental abruption, uterine atony, retained placenta, placenta accreta, general anesthesia, and placental ad- hesion were higher in the PPH group than in the non-PPH group (all P<0.05). The detailed data are presented in (Table 1).
Data are n (%) or mean ± standard deviation. PPH: postpartum hemorrhage; HELLP: Hemolysis, Elevated Liver enzymes, and Low Platelets. Establishment of the Neural Network Model: Multilayer perceptron was used to establish the neural network model. The presence or absence of PPH was designated as the dependent variable (assignment: present = 1, absent = 0). Factors associated with PPH were selected as independent variables from (Table 1). Normalization was applied to all categorical variables in the input layer (assignment: present = 1, absent = 0). The dataset was randomly partitioned into the training and test sets. The training set comprised 70% of the total patient population, and the test set accounted for the remaining 30%. The number of nodes in the hidden layer was automatically computed, and the hyperbolic tangent function was chosen as the activation function. Batch processing was used for model training, with the optimization algorithm utilizing the adjusted conjugate gradient method. To simplify the analysis, the importance of each factor was ranked in descending order.
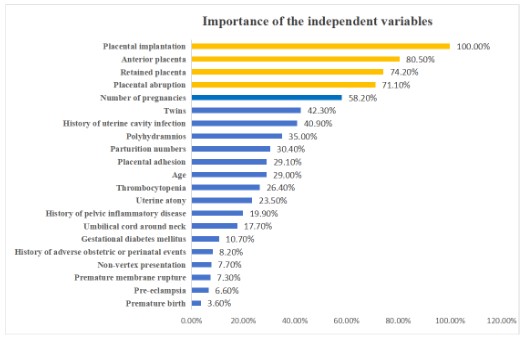
A neural network model with one hidden layer and four neurons was obtained. The model had a predictive accuracy of 95.3% in the training set and 95.4% in the test set (Table 2). The results of the importance analysis for the independent variables indicated that placental implantation, anterior placenta, retained placenta, placental abruption were significant influencing factors (importance > 70%). The contribution rates for all independent variables are detailed in (Table 3 and Figure 1).
Table 1: Analysis of factors associated with postpartum hemorrhage in the PPH and non-PPH groups.
| Parameters | PPH group (n=1050) | Non-PPH group (n=22440) | χ²/t | P-value |
|---|---|---|---|---|
| Age | 31.63±6.05 | 31.09±5.57 | 2.833 | 0.005 |
| Assisted reproductive technology | 77(7.33) | 1297(5.78) | 4.100 | 0.051 |
| Number of pregnancies | 4.99±4.84 | 2.98±2.34 | -6.625 | 0.000 |
| Parturition numbers | 1.74±1.02 | 1.45±0.93 | 10.132 | 0.000 |
| Macrosomia | 43 (4.10%) | 776 (3.46%) | 1.065 | 0.301 |
| Twins | 98 (9.33%) | 803 (3.58%) | 84.732 | 0.000 |
| History of cesarean section | 322(30.67) | 7035(31.35) | 0.219 | 0.658 |
| History of adverse obstetric or perinatal events | 215(20.48) | 4025(17.94) | 4.252 | 0.040 |
| Non-vertex presentation | 349(33.24) | 6261(27.9) | 19.134 | 0.000 |
| Stillbirth | 16(1.52) | 189(0.84) | 3.904 | 0.006 |
| Uterine fibroids | 144(13.71) | 1382(6.16) | 72.016 | 0.000 |
| Anterior placenta | 253(24.1) | 1071(4.77) | 421.236 | 0.000 |
| Umbilical cord around neck | 216(20.57) | 5972(26.61) | 19.841 | 0.000 |
| Preexisting hypertension before pregnancy | 45(4.29) | 814(3.63) | 1.174 | 0.313 |
| Pregnancy-induced hypertension | 28(2.67) | 522(2.33) | 0.488 | 0.531 |
| Pre-eclampsia | 67(6.38) | 1022(4.55) | 6.842 | 0.011 |
| HELLP syndrome | 2(0.19) | 17(0.08) | 1.200 | 0.627 |
| Gestational diabetes mellitus | 64(6.10) | 1742(7.76) | 4.196 | 0.041 |
| Diabetes mellitus before pregnancy | 73(6.95) | 1862(8.3) | 2.519 | 0.121 |
| Hepatitis B | 4(0.38) | 51(0.23) | 0.859 | 0.519 |
| Peripartum cardiomyopathy | 2(0.19) | 51(0.23) | 0.064 | 0.801 |
| History of pelvic inflammatory disease | 83(7.9) | 1088(4.85) | 17.059 | 0.000 |
| History of vaginitis | 65(6.19) | 1640(7.31) | 1.949 | 0.163 |
| Peripartum sepsis | 10(0.10) | 6(0.03) | 1.023 | 0.274 |
| History of uterine cavity infection | 68(6.48) | 479(2.13) | 57.706 | 0.000 |
| Thrombocytopenia | 26(2.48) | 225(1.00) | 15.293 | 0.000 |
| Polyhydramnios | 17(1.62) | 234(1.04) | 2.201 | 0.138 |
| Oligohydramnios | 69(6.57) | 1462(6.52) | 0.005 | 0.956 |
| Post-term pregnancy | 183(17.43) | 3571(15.91) | 1.766 | 0.184 |
| Intrahepatic cholestasis of pregnancy | 33(3.14) | 588(2.62) | 0.825 | 0.364 |
| Induced abortion | 33(3.14) | 824(3.67) | 0.617 | 0.432 |
| Premature birth | 199(18.95) | 2650(11.81) | 42.231 | 0.000 |
| Premature membrane rupture | 128(12.19) | 3322(14.8) | 5.116 | 0.018 |
| Placental abruption | 17(1.62) | 115(0.51) | 29.017 | 0.000 |
| Uterine atony | 182(17.33) | 2049(9.13) | 65.317 | 0.000 |
| Retained placenta | 50(4.8) | 6(0.03) | 203.603 | 0.000 |
| Placental implantation | 109(10.38) | 188(0.84) | 313.767 | 0.000 |
| Placental adhesion | 788(75.05) | 12802(57.05) | 141.351 | 0.000 |
Table 2: Analysis of factors associated with postpartum hemorrhage in the PPH and non-PPH groups.
| Samples | Measured results | Number of cases | Predicted results | ||
|---|---|---|---|---|---|
| Non-PPH | PPH | Correct percentage | |||
| Training set | Non-PPH | 15675 | 15571 | 104 | 99.3% |
| PPH | 730 | 663 | 67 | 9.2% | |
| Total | 16405 | 16234 | 171 | 95.3% | |
| Test set | Non-PPH | 6713 | 6680 | 33 | 99.5% |
| PPH | 320 | 294 | 26 | 8.1% | |
| Total | 7033 | 6974 | 39 | 95.4% | |
Dependent variable: Postpartum Hemorrhage (PPH).
Table 3: The importance of independent variables.
| Independent Variables | Importance | Standardized Importance |
|---|---|---|
| Age | .040 | 29.0% |
| Number of pregnancies | .081 | 58.2% |
| Parturition numbers | .042 | 30.4% |
| Twins | .059 | 42.3% |
| History of adverse obstetric or perinatal events | .011 | 8.2% |
| Non-vertex presentation | .011 | 7.7% |
| Anterior placenta | .111 | 80.5% |
| Umbilical cord around neck | .024 | 17.7% |
| Pre-eclampsia | .009 | 6.6% |
| Gestational diabetes mellitus | .015 | 10.7% |
| History of pelvic inflammatory disease | .028 | 19.9% |
| History of uterine cavity infection | .057 | 40.9% |
| Thrombocytopenia | .037 | 26.4% |
| Polyhydramnios | .048 | 35.0% |
| Premature birth | .005 | 3.6% |
| Premature membrane rupture | .010 | 7.3% |
| Placental abruption | .098 | 71.1% |
| Uterine atony | .033 | 23.5% |
| Retained placenta | .103 | 74.2% |
| Placental implantation | .138 | 100.0% |
| Placental adhesion | .040 | 29.1% |
Discussion/conclusion
The Qiandongnan Miao and Dong Autonomous Prefecture, located in Guizhou Province, China, is a culturally diverse region that is primarily inhabited by the ancient and distinct Miao and Dong ethnic groups. With societal development, the demographic profile of pregnant women in this region has been constantly changing. For instance, there has been an increase in the number of pregnancies in people of advanced maternal age. In this study, the average maternal age at childbirth was 31.11 years. Social factors have also led to an increase in the rates of miscarriage and cesarean section, potentially causing placenta accreta in subsequent pregnancies. Cultural practices during pregnancy play significant roles among these ethnic groups. Many expectant mothers are influenced by traditional Chinese medicine culture, using herbs like Yi Mu Cao, which have unknown side effects, to maintain prenatal health. Due to genetic factors related to race, pregnant women in this region tend to have smaller body sizes and narrower pelvises, resulting in the requirement for cesarean section deliveries. Research has indicated that ethnicity is a risk factor for PPH, with signifi- cant differences in the rates of PPH among ethnic groups, such as those from sub-Saharan Africa and the Pacific islands [10-13]. Preventing PPH is crucial for ensuring reproductive health, and machine learning has been proposed as a reliable method to enhance the accuracy of PPH prediction [14-16]. The present study used a multilayer perceptron neural network model to identify risk factors for PPH in Qiandongnan Miao and Dong Autonomous Prefecture, China, providing personalized prevention strategies. The results highlighted placental implantation, anterior placenta, retained placenta, placental abruption as significant influencing factors (contribution rate >70%). The model demonstrated an accuracy exceeding 95%, indicating robust predictive performance, which is consistent with the findings of previous studies [17,18]. To compare our results with those from other regions, we reviewed the previously published literature. Some studies identified many risk factors for PPH, among which the most significant were placenta previa, placental abruption, uterine rupture, and multiple pregnancies [19]. These risk factors have similarities with the risk factors identified in our study, but there are also differences. In a previous study, regression analysis revealed that maternal age <18 years, previous cesarean section, history of PPH, assisted reproductive technology, pre-delivery anemia, stillbirth, prolonged labor, and giant fetus were significant risk factors for severe PPH [20], differing from the local risk factors identified in the present study. Moreover, a retrospective cohort study [21] of pregnant women at tertiary hospitals in central and southern Louisiana showed that the incidence of PPH was 12.3%. Black people, higher body mass index, and cesarean section were associated with PPH risk. The incidence rate of the study was 4.47% (1,050/23,490), indicating significant differences between races. A case-control study [22] of PPH in the northern province of Rwanda showed that the overall incidence of primary PPH was 25.2%. Prenatal bleeding, multiple pregnancies, uterine contractions, residual placental tissue, and genital organ tears were all risk factors for PPH, which were significantly different from those in the Qiandongnan region. At a hospital in Greece, the incidence rate of PPH was 2.5%. Maternal age greater than 35 years, preterm delivery, uterine atony, and placental retention were identified as independent predictors of PPH, some of which were similar and others of which were different from those in the Qiandongnan region. Another retrospective cohort study [23] involving 360,370 women with PPH showed that Black women had a higher risk of serious incidence rate and mortality associated with PPH. These research results indicate that there are differences in the occurrence and prognosis of PPH among races. Particularly, there are differences between ethnic minority areas in Qiandongnan and other regions, and it is necessary to be vigilant during the prenatal and perinatal periods to identify women with risk factors and to conduct early intervention to prevent PPH. Despite the valuable insights gained from our results, this study has some limitations that should be considered. This was a single-center retrospective study, and future research should involve multicenter validation and model refinement to establish stronger associations between predictions and patient outcomes. The rate of PPH differs between women in the Qiandongnan region and women from other regions. Risk factors, such as placental implantation, anterior placenta, retained placenta, placental abruption, should be thoroughly identified during prenatal care. The neural network model developed in this study demonstrated good efficacy in predicting PPH. In clinical practice, it is crucial to identify these high-risk factors, promptly implement emergency measures, and prevent adverse outcomes.
Declarations
Competing interests: All authors declare that there is no conflict of interest.
Funding: Supported by the Science and Technology Support Program of Qiandongnan Prefecture ([2021]11), and Guizhou Province High-Level Innovative Talent Training Program ([2022]201701).
References
- Bienstock JL, Eke AC, Hueppchen NA. Postpartum Hemorrhage. N Engl J Med. 2021; 384(17): 1635-1645.
- Patek K, Friedman P. Postpartum Hemorrhage-Epidemiology, Risk Factors, and Causes. Clin Obstet Gynecol. 2023; 66(2): 344- 356.
- Wang S, Rexrode KM, Florio AA, et al. Maternal Mortality in the United States: Trends and Opportunities for Prevention. Annu Rev Med. 2023; 74: 199-216.
- Sitaula S, Basnet T, Agrawal A, et al. Prevalence and risk factors for maternal mortality at a tertiary care centre in Eastern Nepal-retrospective cross-sectional study. BMC Pregnancy Childbirth. 2021; 21(1): 471.
- Carr BL, Jahangirifar M, Nicholson AE, et al. Predicting postpartum haemorrhage: A systematic review of prognostic models. Aust N Z J Obstet Gynaecol. 2022; 62(6): 813-825.
- Shen JJ, Mojtahedi Z, Vanderlaan J, Rathi S. Disparities in Adverse Maternal Outcomes Among Five Race and Ethnicity Groups. J Womens Health (Larchmt). 2022; 31(10): 1432-1439.
- Gyamfi-Bannerman C, Srinivas SK, Wright JD, et al. Postpartum hemorrhage outcomes and race. Am J Obstet Gynecol. 2018; 219(2): 185.1-185.10.
- Escobar MF, Nassar AH, Theron G, et al. FIGO recommendations on the management of postpartum hemorrhage 2022. Int J Gynaecol Obstet. 2022; 157-1(1): 3-50.
- von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007; 147: 573-577.
- Linde LE, Ebbing C, Moster D, et al. Recurrence of postpartum hemorrhage in relatives: A population-based cohort study. Acta Obstet Gynecol Scand. 2021; 100(12): 2278-2284.
- Butwick AJ. Postpartum hemorrhage and low fibrinogen levels: the past, present and future. Int J Obstet Anesth. 2013; 22(2): 87-91.
- Westcott JM, Hughes F, Liu W, et-al. Prediction of Maternal Hemorrhage Using Machine Learning: Retrospective Cohort Study. J Med Internet Res. 2022; 24(7): 34108.
- Okunlola O, Raza S, Osasan S, et al. Race/Ethnicity as a Risk Factor in the Development of Postpartum Hemorrhage: A Thorough Systematic Review of Disparity in the Relationship Between Pregnancy and the Rate of Postpartum Hemorrhage. Cureus. 2022; 14(6): 26460.
- Mehrnoush V, Ranjbar A, Farashah MV, et al. Prediction of post- partum hemorrhage using traditional statistical analysis and a machine learning approach. AJOG Glob Rep. 2023; 3(2): 100185.
- Ende HB. Risk assessment tools to predict postpartum hemorrhage. Best Pract Res Clin Anaesthesiol. 2022; 36(3-4): 341-348.
- Boujarzadeh B, Ranjbar A, Banihashemi F, et al. Machine learning approach to predict postpartum haemorrhage: a systematic review protocol. BMJ Open. 2023; 13(1): 067661.
- Venkatesh KK, Strauss RA, Grotegut CA, et al. Machine Learning and Statistical Models to Predict Postpartum Hemorrhage. Obstet Gynecol. 2020; 135(4): 935-944.
- Akazawa M, Hashimoto K, Katsuhiko N, Kaname Y. Machine learning approach for the prediction of postpartum hemorrhage in vaginal birth. Sci Rep. 2021; 11(1): 22620.
- Ende HB, Lozada MJ, Chestnut DH, et al. Risk Factors for Atonic Postpartum Hemorrhage: A Systematic Review and Meta-analysis. Obstet Gynecol. 2021; 137(2): 305-323.
- Liu CN, Yu FB, Xu YZ, et al. Prevalence and risk factors of severe postpartum hemorrhage: a retrospective cohort study. BMC Pregnancy Childbirth. 2021; 21(1): 332.
- Taylor K, Noel E, Chapple AG, et al. Risk factors for postpartum hemorrhage in a tertiary hospital in South-Central Louisiana. J Matern Fetal Neonatal Med. 2022; 35(25): 7353-7359.
- Bazirete O, Nzayirambaho M, Umubyeyi A, et al. Risk factors for postpartum haemorrhage in the Northern Province of Rwanda: A case control study. PLoS One. 2022; 17(2): 0263731.
- Gyamfi-Bannerman C, Srinivas SK, Wright JD, et al. Postpartum hemorrhage outcomes and race. Am J Obstet Gynecol. 2018; 219(2): 185.1-185.10.