Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Series - Open Access, Volume 6
Stent graft puncture as a method of optimizing coronary angioplasty complicated by vessel perforation
Rafał Celiński, PhD; Marcin Łubiarz, MD; Kamil Banasik, MD*
Department of Cardiology, Specialist Hospital in Chełm, Poland.
*Corresponding Author : Kamil Banasik, MD
Department of Cardiology, Specialist Hospital in
Chelm, Ceramiczna 1, 22-100 Chełm, Poland.
Tel: +48 82 56 23 277
Email: kamil1.16@o2.pl
Received : Jan 22, 2025
Accepted : Feb 17, 2025
Published : Feb 24, 2025
Archived : www.jcimcr.org
Copyright : © Banasik K (2025).
Abstract
Percutaneous Coronary Interventions (PCI) are widely performed procedures in modern cardiology but carry risks, including vessel perforation. This report describes two cases of Left Main Coronary Artery (LMCA) perforation managed with stentgraft implantation, followed by reopening of occluded side branches using specialized Chronic Total Occlusion (CTO) guidewires (Confianza PRO).
In the first case, a 75-year-old woman underwent LMCA bifurcation PCI. Vessel perforation during the procedure led to pericardial tamponade and cardiac arrest, successfully managed by stentgraft placement. However, the LCx branch was occluded by the stentgraft. Using CTO techniques, LCx patency was restored, achieving TIMI 3 flow. In the second case, a 90-year-old woman presented with NSTEMI and LMCA perforation during PCI. After stentgraft placement and stabilization, the LAD branch was recanalized with CTO techniques, achieving similar angiographic success.
Despite technical success, both patients succumbed to complications shortly after the procedures. These cases underscore the potential of advanced PCI tools in managing complications but highlight the critical importance of balancing procedural optimization with timely intensive care. Sharing such experiences may enhance procedural strategies and improve outcomes in complex PCI scenarios.
Keywords: Percutaneous coronary intervention; Vessel perforation; Stentgraft implantation; Bifurcation PCI.
Abbreviations: PCI: Percutaneous Coronary Intervention; LMCA: Left Main Coronary Artery; CTO: Chronic Total Occlusion; LAD: Left Anterior Descending artery; LCx: Left Circumflex artery; TIMI: Thrombolysis In Myocardial Infarction; NSTEMI: Non-ST-Elevation Myocardial Infarction .
Citation: Celinski R, Lubiarz M, Banasik K. Stent graft puncture as a method of optimizing coronary angioplasty complicated by vessel perforation. J Clin Images Med Case Rep. 2025; 6(2): 3480.
Introduction
Percutaneous Coronary Interventions (PCI) are among the most commonly performed medical procedures in Poland. Like any medical procedure, they carry a risk of complications. One of the most frequent risks is vessel perforation during the intervention. Fortunately, effective treatment options, such as the implantation of a stentgraft, are available. A natural consequence of this treatment is the occlusion of side branches of the treated artery [1-3].
This report presents two cases of PCI complicated by perforation of the left main coronary artery, managed by stentgraft implantation, followed by reopening of the occluded side branch using a specialized guidewire designed for Chronic Total Occlusion (CTO) procedures (Confianza PRO).
Case 1
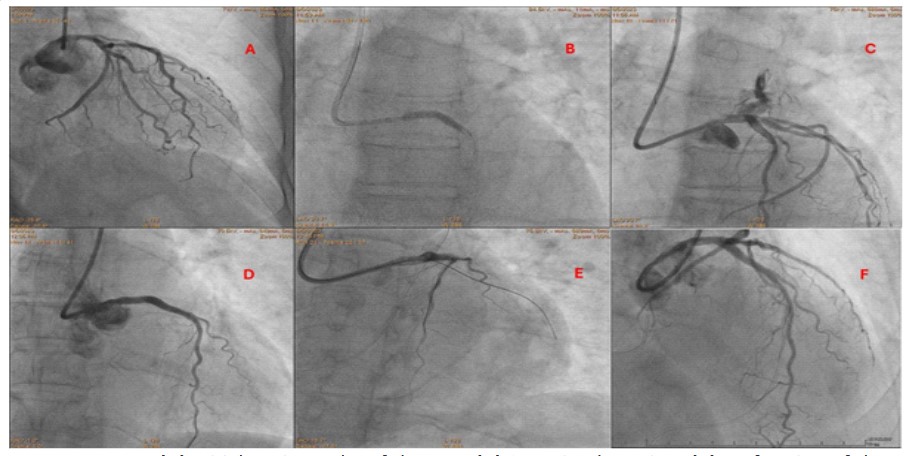
A 75-year-old female patient was admitted to the cardiology department due to class III angina symptoms according to the Canadian Cardiovascular Society (CCS) classification. Coronary angiography revealed multivessel coronary artery disease involving the Left Main Coronary Artery (LMCA). Due to the patient’s refusal of the proposed Coronary Artery Bypass Grafting (CABG), a percutaneous revascularization approach was chosen. In the first step, the angioplasty of the circumflex branch (LCx) of the left coronary artery was performed with the implantation of a Drug-Eluting Stent (DES). Despite the initial intervention, the patient continued to experience symptoms and dynamic ST-segment changes on the ECG. A follow-up coronary angiography showed satisfactory results from the previous procedure. The intervention at the LMCA bifurcation was undertaken. After predilation with balloon catheters, a stent (Promus PREMIER 3.5×20 mm) was implanted in the LM-LCx direction. A second stent (Ultimaster 4.0×38 mm) was deployed from LM to the Left Anterior Descending artery (LAD). During contrast injection, vessel perforation was observed.
The patient’s condition deteriorated, presenting with shock symptoms. Echocardiography confirmed pericardial effusion with right ventricular compression. Emergency pericardiocentesis evacuated approximately 150 ml of blood. The perforation was managed by implanting a stentgraft (Papyrus 3.5×20 mm). However, the patient experienced cardiac arrest due to electromechanical dissociation. After successful resuscitation, angiographic imaging confirmed no further bleeding but revealed occlusion of the LCx, whose ostium was covered by the stent graft.
Using multiple attempts with hydrophilic guidewires, the stentgraft membrane was successfully penetrated with the CTO guidewire (Confianza PRO). The administration of contrast through the microcatheter (ASAHI Corsair Pro) confirmed the correct position of the guidewire. The LCx ostium was dilated with progressively larger balloon catheters, and the procedure was optimized using the “kissing balloons” and Proximal Optimization Technique (POT) with an NC balloon (5.0×12 mm), achieving TIMI 3 flow in both vessels.
Case 2
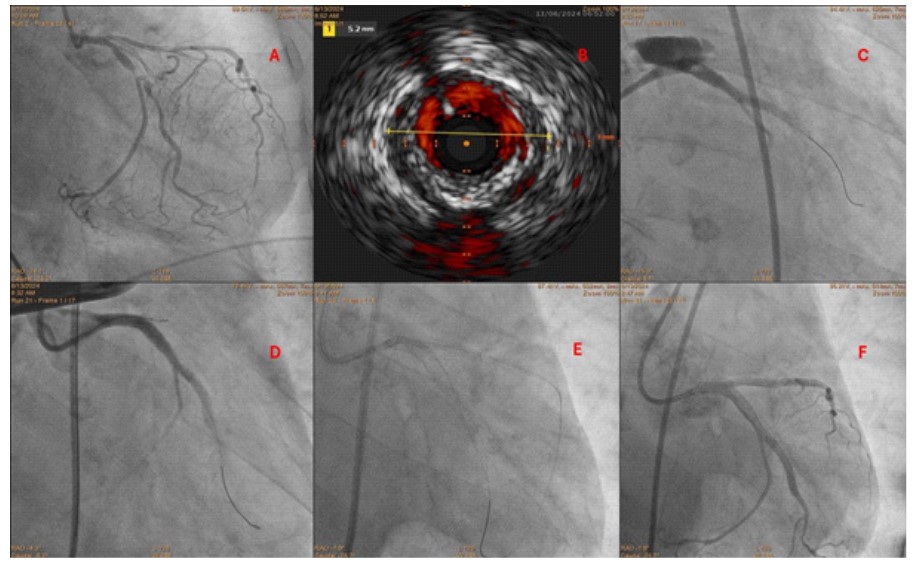
A 90-year-old female patient was admitted with Non-ST-Elevation Myocardial Infarction (NSTEMI) and chest pain. Laboratory tests showed elevated troponin levels. Coronary angiography revealed multivessel coronary artery disease. Due to the patient’s advanced age, CABG was not considered. Firstly, the PCI of the LCx branch was performed with DES implantation. In the second step, the angioplasty of the LMCA bifurcation was planned. Following Intravascular Ultrasound (IVUS) assessment and predilatation, a stent (Resolute Onyx 4.5×26 mm) was implanted from LM to LCx. Contrast injection revealed LMCA perforation and pericardial tamponade.
The patient experienced cardiac arrest due to electromechanical dissociation and was resuscitated. Pericardiocentesis effectively drained the pericardial fluid. The perforation was managed with a stent graft (Papyrus 4.0×20 mm). After restoring hemodynamic stability, efforts to recanalize the LAD branch were made, as its ostium was covered by the stentgraft membrane. Based on experience from the first case, the CTO guidewire (Confianza PRO) was utilized to penetrate the stent graft membrane, and a microcatheter (ASAHI Corsair Pro) was introduced. Contrast injection confirmed correct guidewire positioning. The LAD ostium was dilated using progressively larger balloon catheters, optimized with “kissing balloons” and POT (NC 4,5×15 mm), achieving TIMI 3 flow in both vessels.
Outcome
Despite optimal angiographic results, both patients died a few days post-procedure due to hemorrhagic and ischemic complications.
Conclusion
These cases highlight rare examples of optimized management of complicated PCI procedures using available tools. However, the use of such techniques should only be considered when they can be performed efficiently. Prolonged procedures delaying specialized treatment in the intensive care unit may be counterproductive. Sharing these experiences may improve awareness of the capabilities and limitations of available equipment, contributing to the optimization of PCI procedures [4-6].
References
- Solomonica A, Kerner A, Feld Y, et al. Novel Technique for the Treatment of Coronary Artery Perforation. Can J Cardiol. 2020; 36: 1326.e1-1326.e3
- Nagalli S, Hajouli S. Coronary Artery Perforation. 2023 Jul 3. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2024 Jan. PMID: 32119363
- Abdalwahab A, Farag M, Brilakis ES, et al. Management of Coronary Artery Perforation. Cardiovasc Revasc Med. 2021; 26: 55-60.
- Monteleone PP, Yeh RW. Management of Complications. Interv Cardiol Clin. 2016; 5: 201-209.
- Means G, End C, Kaul P. Management of Percutaneous Coronary Intervention Complications. Curr Treat Options Cardiovasc Med. 2017; 19: 25.
- Doll JA, Hira RS, Kearney KE, et al. Management of Percutaneous Coronary Intervention Complications: Algorithms From the 2018 and 2019 Seattle Percutaneous Coronary Intervention Complications Conference. Circ Cardiovasc Interv. 2020; 13: e008962.