
Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
A rare case of high-grade chondroblastic osteosarcoma post-radiotherapy for a right frontal oligodendroglioma
Sinead Horan*; Oscar Breathnach; Liam Grogan; David Fitzpatrick; Patrick Morris; Jarushka Naidoo; Guhan Rangaswamy; Marion Quinn; Francesca Brett; Alan Beausang; Adrian Murphy
Beaumont Hospital, Ireland.
*Corresponding Author : Sinead Horan
Beaumont Hospital, Ireland.
Email: sineadhoran@rcsi.ie
Received : Feb 13, 2021
Accepted : Mar 22, 2021
Published : Mar 24, 2021
Archived : www.jcimcr.org
Copyright : © Horan S (2021).
Abstract
This is the fourteenth case of an intracranial and dural-based osteosarcoma in the literature to date. The case involves a forty-year old woman with a previous history of a brain tumour, which was treated with surgery, chemotherapy and radiotherapy six years previously. The hypothesis is that this rare malignancy is secondary to the radiation exposure given the growth of the lesion in the previous radiation field.
Keywords: Chondroblastic osteosarcoma, Radiation-induced, Primary meningeal osteosarcoma.
Citation: Horan S, Breathnach O, Grogan L, Fitzpatrick D, Morris P, et al. A rare case of high-grade chondroblastic osteosarcoma post-radiotherapy for a right frontal oligodendroglioma. J Clin Images Med Case Rep. 2021; 2(2): 1033.
Introduction
Radiation-induced secondary malignancies are a well-recognised side effect of radiation therapy. Contributing factors include younger age, increased dose and volume of the irradiated area, treatment zone and radiation technique [1]. Given the improvements in treatment and the growing population of cancer survivors, secondary cancers have risen from 9% of all cancers in 1975-1979 to 19% in 2005-2009 [2]. Osteosarcomas are a “heterogeneous group of malignancies with bone formation or mesenchymal tissue with histopathological evidence of osteogenic differentiation”. There is a predominance of chondroid matrix in the tumour cells [3]. Here we present a rare case of high-grade chondroblastic osteosarcoma post-radiotherapy for a right frontal oligodendroglioma.
Case description
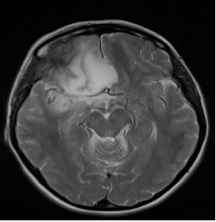
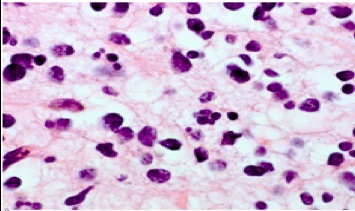
A 40-year-old woman was diagnosed with a 5 cm grade II right frontal oligodendroglioma in 2014 (See Figure 1). She underwent subtotal debulking surgery. The histology was IDH1 mutant, ATRX equivocal and P53 expressed. 1p19q was not co deleted. This was a grade two oligodendroglioma (see Figure 2a and 2b). She had a history of growth hormone deficiency, for which she was on growth hormone, and epilepsy. The tumour was fifty percent debulked as assessed by imaging, and she proceeded to receive 54Gy in 30 fractions of radiotherapy. The radiotherapy met high-risk criteria due to the risk of neurological deficit, tumour growth across the midline, and the subtotal resection size. She was planned for six cycles of adjuvant PCV (procarbazine, lomustine (CCNU) and vincristine) chemotherapy, which was discontinued after four cycles due to grade II diarrhoea and deranged liver function tests.
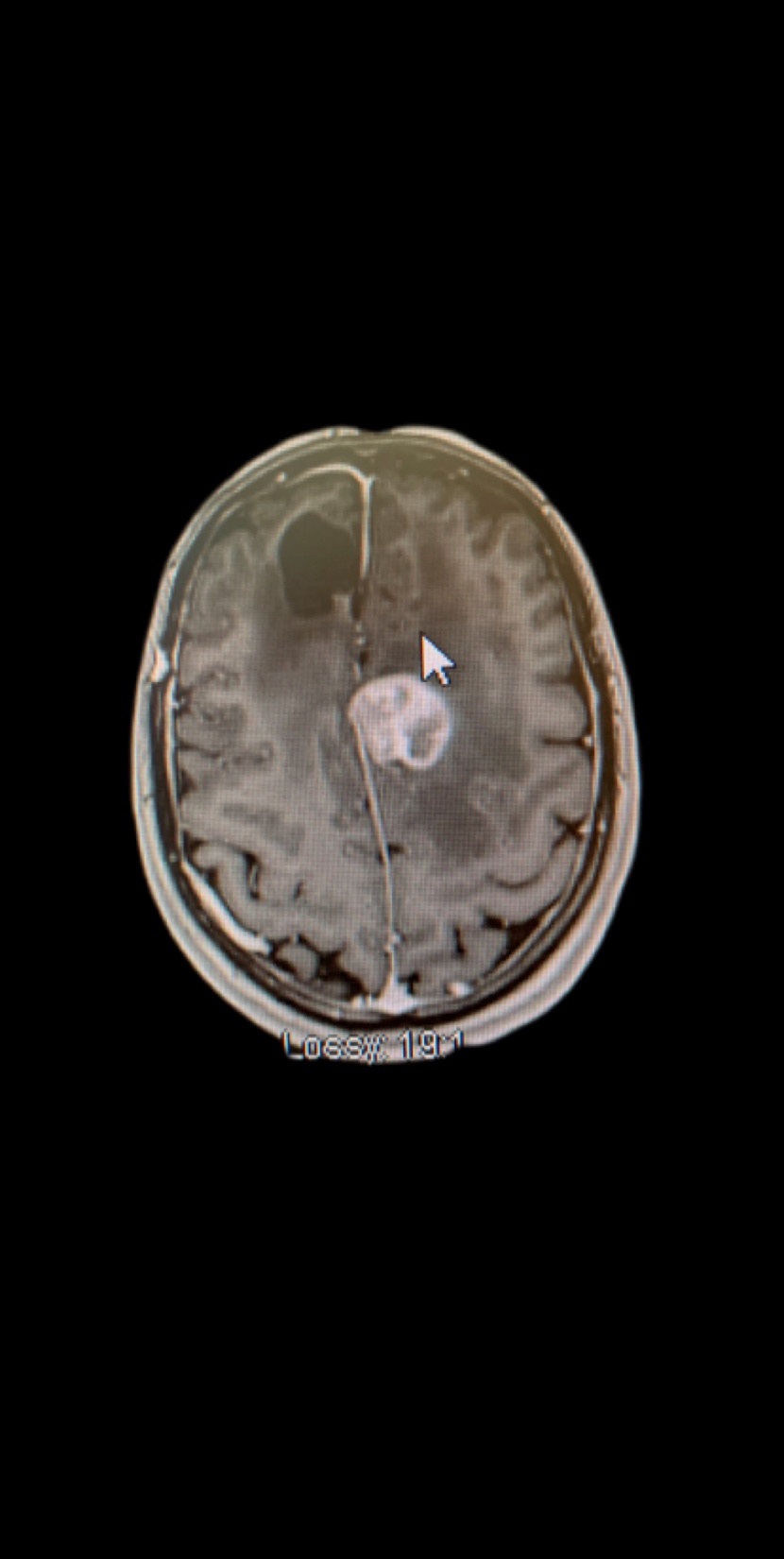
She remained well until September 2020 when a surveillance MRI brain reported a tumour recurrence in the falx and dura close to the previous surgery site. Measuring 47 x 45 x 32 mm, it was arising from the falx and notably, not the skull bone. It had the appearance of a meningioma with atypical features (see Figure 3). There were no distant metastases found on imaging. She underwent a craniotomy with a significant subtotal excision of the left parafalcine mass. There was residual tumour superiorly extending on both sides of the falx, invading the superior sagittal sinus, measuring 37 x 29 x 23 mm. This superior sagittal sinus invasion precluded full excision of the lesion.
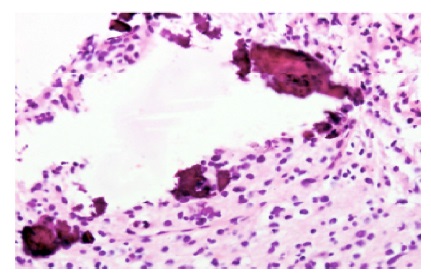
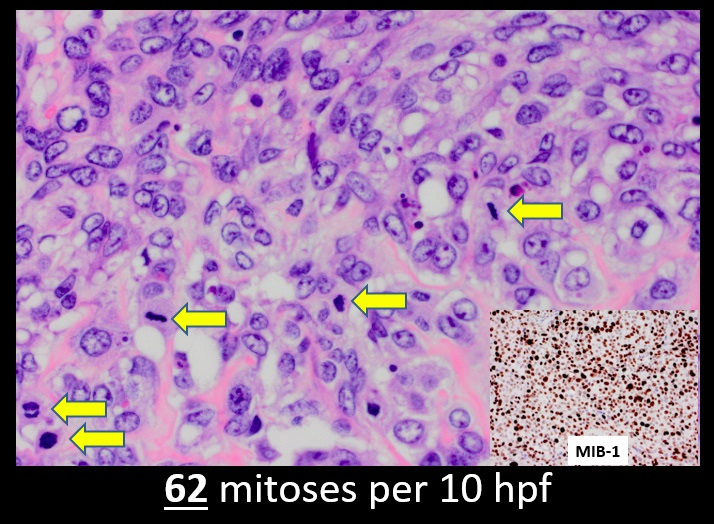
Unexpectedly, the histology from the resection showed a highgrade chondroblastic osteosarcoma with brain invasion. There was no evidence of a glial component to suggest recurrence or high-grade sarcomatous transformation of the previously resected right frontal low-grade glioma. Whilst focal EMA and SSTR2 expression were seen, anaplastic meningioma with heterologous differentiation was not favoured due to the relatively short latent period between prior radiotherapy and tumour development, and the extensive well-formed sarcomatous elements (See Figure 4). She is currently undergoing ten cycles of methotrexate, doxorubicin and cisplatin (MAP chemotherapy). She is planned for brain radiotherapy upon completion of chemotherapy.
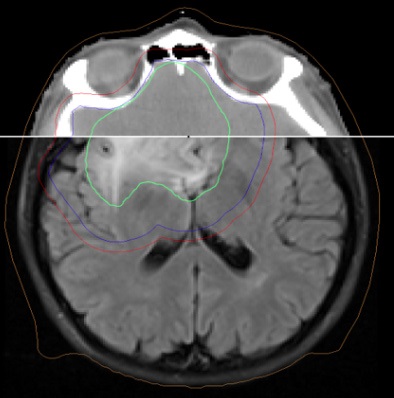
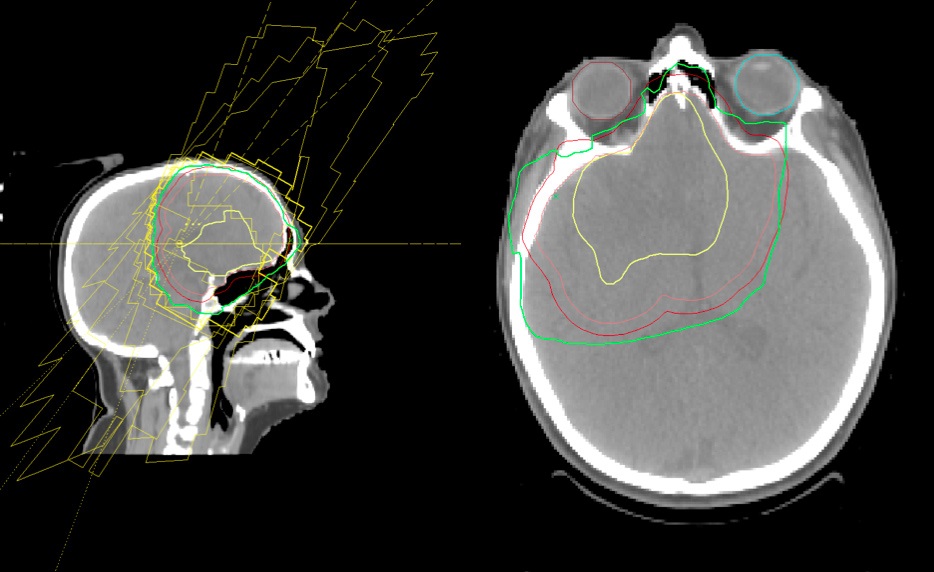
We assessed current and prior brain imaging to determine whether the new tumour developed within the prior radiotherapy’s radiation field. Figure 5 is an axial slice of the original planning CT in 2014 fused with her MRI scan showing the T2 flair abnormality in green encompassed by Clinical Target Volume (CTV) in blue with 5 mm margin to Planning Target Volume (PTV) in red. Figure 6 shows the radiotherapy plan with the beam arrangements and PTV encompassed by the 95% isodense line in green. It is clearly seen that the new lesion, the high-grade chondroblastic osteosarcoma, has developed within the radiation field of the previous lesion.
Discussion
In this case, we present an exceedingly rare case of intracranial and dural-based osteosarcoma. Intracranial osteosarcomas usually occur as metastases; however, these too are unusual with a reported incidence of 1.8–5.6% of primary osteosarcomas. They are associated with pulmonary metastasis, with the consensus that lung tumour emboli metastasise to the brain [4].
They are also known as primary meningeal osteosarcomas. Due to the lack of characteristic changes on imaging, it is difficult to distinguish these tumours from meningiomas [5].
Romeo et al. [6] have noted thirteen documented intracranial and dural-based osteosarcoma cases in the literature, and now to our knowledge, this is the fourteenth case to date. Of the thirteen documented cases of meningeal dura-based osteosarcomas, eight cases occurred de novo. Five developed after previous radiation for meningioma or glioblastoma with intervals ranging from 7 months to 22 years. Of these thirteen cases, histopathological classification had only been noted in three cases; two chondrogenic osteosarcomas and one fibroblast osteosarcoma. Prognostic factors and standardised treatment regimens do not exists [6]. Unfortunately, the prognosis of radiation-induced osteosarcomas is less favourable the prognosis of primary osteosarcoma [7].
Radiation-induced osteosarcomas are usually associated with doses exceeding 30 Gy [8]. Radiation-induced osteosarcomas typically occur at the periphery of the radiation field, and the hypothesis is that the radiation, whilst not strong enough to cause cell death, can induce malignant transformation [9].
Radiation-induced sarcomas develop in 1 in 1000 patients who survive five years post-radiotherapy. The criteria for defining a new tumour as a post-radiation sarcoma include; development of the tumour within the previous radiation field and at least three years between radiation and tumour development [10]. Our case fulfils these criteria, as demonstrated by the planning images in Figure 5 and Figure 6 and an interval period of six years.
Conclusion
This is the fourteenth case of intracranial and dural-based osteosarcoma to date. It is a rare cancer occurring secondary to radiotherapy. Pathology is paramount in diagnosing these tumours, particularly if there is a history of radiation and imaging is suggestive of a meningioma. A multidisciplinary approach to care was adopted in this case involving surgery, chemotherapy and radiotherapy [6].
References
- Dracham CB, Shankar A, Madan R. Radiation induced secondary malignancies: A review article. Radiat Oncol J. 2018; 36(2): 85-94.
- Morton LM, Onel K, Curtis RE, Hungate EA, Armstrong GT. The rising incidence of second cancers: Patterns of occurrence and identification of risk factors for children and adults. Am Soc Clin Oncol Educ Book. 2014; e57-67.
- Almeida E, Mascarenhas BA, Cerqueira A, Medrado AR. Chondroblastic osteosarcoma. J Oral Maxillofac Pathol. 2014; 18(3): 464-468.
- Doval DC, Chacko M, Sinha R, Choudhury KD, Sharma A, Rao A, Mehta A. A rare case of brain metastasis in a patient with osteosarcoma. South Asian journal of cancer. 2017; 6(1): 36-37.
- Ghosal N, Dadlani R, Furtado S, Bagdi N, Hegde A. Dural based primary osteosarcoma in right fronto-temporal region: Case report with review of literature. Neurology India. 2010; 58(1): 128-130.
- Romeo E, Gisserot O, de Jaureguiberry JP, Desse N, Souraud JB, Salem N, Bertucci F. Meningeal chondroblastic osteosarcoma: case report and review of the literature. J Neurooncol. 2010; 100(2), 305-309.
- Ito T, Ozaki Y, Sato K, Oikawa M, Tanino M, Nakamura H, Tanaka, S. Radiation-induced osteosarcomas after treatment for frontal gliomas: a report of two cases. Brain Tumor Pathol. 2010; 27(2): 103-109.
- Arlen M, Higinbotham NL, Huvos AG, Marcove RC, Miller T, Shah IC. Radiation-induced sarcoma of bone. Cancer. 1971; 28(5): 1087- 1099.
- Lee YY, Van Tassel P, Nauert C, Raymond AK, Edeiken J. Craniofacial osteosarcomas: plain film, CT, and MR findings in 46 cases. AJR Am J Roentgenol. 1988; 150(6): 1397-1402.
- Bar-Sela G, Tzuk-Shina T, Zaaroor M, Vlodarsky Y, Tsalik M, Kuten A. Primary osteogenic sarcoma arising from the dura mater: case report. Am J Clin Oncol. 2001; 24(4): 418-420.
