Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
Incidental diagnosis of haemophilia: A case report of three cases following voluntary medical male circumcision in South Africa
Donna Jacobs1*; Carla Visser2; Freck Dikgale1 ; Ngoanamathiba Molepo3; Raymond Mabuse1; James Ndirangu4
1 University Research Co., LLC (URC) & Center for Human Services, Pretoria, South Africa
2 RTI International, Pretoria, South Africa.
3 Department of Health, Polokwane, Limpopo, South Africa.
4 Office of the Dean, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa.
*Corresponding Author : Donna Jacobs
University Research Co., LLC (URC), Pretoria, South
Africa.
Email: dtj29@yahoo.com & djacobs@urc-chs.com
Received : Mar 19, 2021
Accepted : Apr 24, 2021
Published : Apr 28, 2021
Archived : www.jcimcr.org
Copyright : © Jacobs D (2021).
Abstract
Introduction: Since 2007, over 15.2 million Voluntary Medical Male Circumcisions (VMMCs) have been performed in 14 sub-Saharan African countries for partial prevention of transmission of HIV. In South Africa, close to 4 million VMMCs have been conducted since the onset of the national VMMC program in 2010. Within this context, the occurrence of notifiable adverse events related to peri-operative bleeding occurs commonly. The ability to screen, diagnose, and manage these cases appropriately will mitigate associated adverse events.
Aim: In this paper, we describe three cases of prolonged bleeding after VMMC procedure and propose program measures.
Methods: Descriptive haemophilia case accrual at three sites implementing a PEPFAR- funded VMMC program. The cases were recruited consecutively over a 17-month period (May 2017 to September 2018). Standard laboratory tests were used to confirm diagnosis. Written assent and informed consent were obtained from each subject and their respective guardians.
Results: A total number of 31 severe or moderate adverse events were reported of whom three 16-year-old clients from three different provinces in South Africa were diagnosed with Haemophilia post VMMC services during July 2018. Two clients were diagnosed with Haemophilia A and one client was diagnosed with Haemophilia B.
Conclusions: Greater emphasis on training and placement of qualified health care workers for peri-operative screening as well as a high index of suspicion for pre-operative diagnosis and appropriate referral for bleeding disorders is highly recommended. Clinical VMMC protocols guiding post-operative wound management, adverse event management, active client follow-up and care need to be reinforced, with rigorous reporting.
Keywords: Prolonged bleeding; Adverse events; Haemophilia; Screening; Bleeding disorders; Incidental diagnosis.
Citation: Jacobs D, Visser C, Dikgale F, Molepo N, Mabuse R, et al. Incidental diagnosis of haemophilia: A case report of three cases following voluntary medical male circumcision in South Africa. J Clin Images Med Case Rep. 2021; 2(2): 1078.
Introduction
Since 2007, over 15.2 million voluntary medical male circumcisions (VMMCs) have been performed in 14 sub-Saharan African countries for partial prevention of HIV [1-3]. In South Africa alone, over 3.9 million VMMCs have been conducted since the inclusion of medical male circumcision in the country’s national HIV prevention program in 2010. Free VMMC services to all eligible males between the ages of 15-49 years form part of the National Department of Health’s strategy to reduce the transmission of HIV as per WHO/UNAIDS recommendations [4]. In line with WHO quality assurance guidance, monitoring, tracking, reporting and mitigating adverse events following VMMC are implemented by all PEPFAR programs [5-7]. Recent reports document that one of the most commonly occurring VMMC notifiable adverse events is bleeding resulting in hospitalization for more than three days [8-10]. Within this context, several causes may be identified, including bleeding disorders. However, the incidence of post-VMMC bleeding due to bleeding disorders, specifically haemophilia is not known. The purpose of this paper is to supplement the existing literature and describe three cases of an infrequent but important occurrence of prolonged postVMMC bleeding due to haemophilia.
The three complications were identified during the course of the first 17 months (May 2017- September 2018) of a newly awarded PEPFAR-funded VMMC program (USAID VMMC Project) in South Africa, which performed 233,865 VMMCs during this period. PEPFAR has been supporting VMMC activities in South Africa since 2010, contracting implementing partners through both USAID and CDC funding mechanisms. These efforts complement those of the South African Department of Health (DOH), which also provides VMMC services as well as local funding to VMMC service delivery institutions. Since the onset of the VMMC program in South Africa in 2010, close to 4 million VMMCs have been performed by various implementing partners, under the auspices of the National and Provincial DOH, South Africa [11].
During May 2017-September 2018, the PEPFAR-funded USAID VMMC Project worked in 14 districts in six provinces of South Africa. A total of 200 fixed, mobile and outreach sites were supported to provide VMMC services. To document the three VMMC Serious Adverse Events related to bleeding disorders presented here, descriptive methodology was used. The cases were accrued from three different VMMC sites, run by a single clinical service delivery partner organization. The cases were recruited consecutively, and detailed case notes were recorded. Written informed consent was obtained from all clients. On the basis of prolonged bleeding (exceeding 24 to 48 hours), laboratory screening and diagnostic tests were done for a coagulation profile, blood count and clotting factor VIII and IX assays. A standard classification of severity of haemophilia was followed (see Table 1). The case notes and laboratory results were summarized in tables.
Table 1: Classification of haemophilia severity
Severity |
Factor (VIII or IX) |
Clinical Presentation / Treatment |
Mild |
5% to 40% |
Occasional bleeding, usually only after severe trauma or |
Moderate |
1% to 5% |
Less frequent bleeding which usually follows trauma, surgery, |
Severe |
<1% |
Factor VIII or IX replacement is needed several times per month for traumatic, or apparently, spontaneous bleeding may be on regular prophylactic factor therapy |
Results
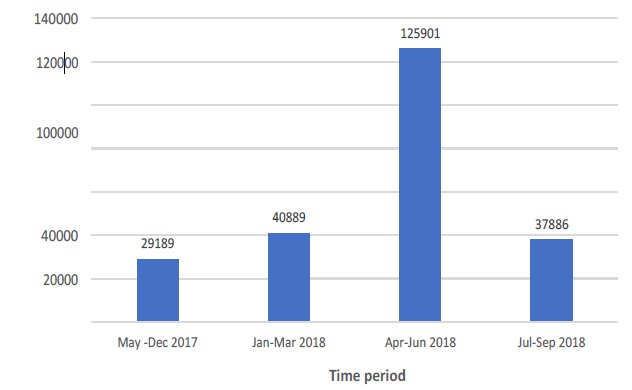
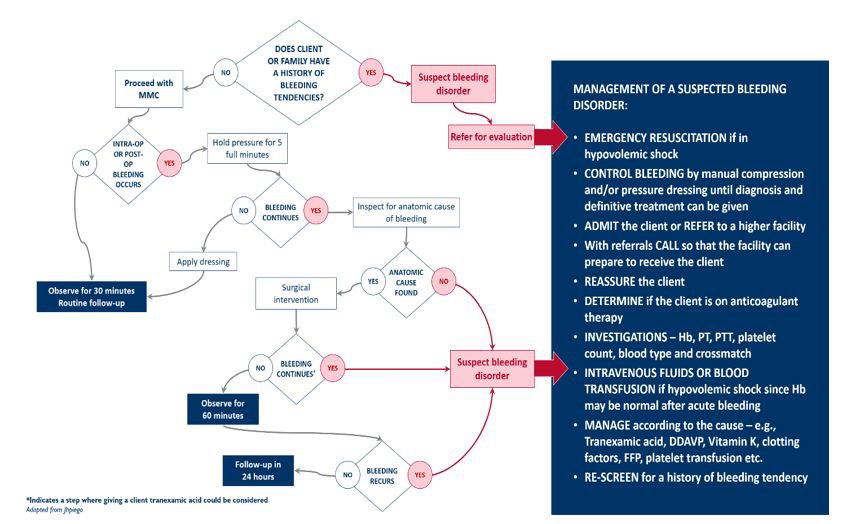
An overall summary of the 233,865 VMMCs done, disaggregated by time period is presented (Figure 1). The total number of severe/moderate adverse events reported (31) is presented (Table 2), disaggregated by type of event. The management of intra-operative and immediate post-operative bleeding is presented (Figure 2). The three haemophilia cases are described (Table 3).
Table 2: Total number of Severe/Moderate Adverse Events reported (May 2017-September 2018)
Total Number |
Bleeding |
Infection |
Wound disruption |
Other |
31 |
3 |
22 |
2 |
4 |
|
|
|
|
|
† other includes pain and / difficulty with micturition
Table 3: Summary of case characteristics
Age (years) & |
Location |
Time to present (days) |
Time to diagnosis (days) & Diagnosi s |
Factor VIII |
Factor IX levels (IU/dl) |
Hb (g/dl) |
Blood products |
Family history |
16 years Student |
Rural |
3 21 |
18 Hem A |
*10.7 |
111.5 |
12.9 |
2000IU (F8) |
Negative |
16 years Student |
Urban |
2 3 |
2 Hem A |
*26 |
ND |
12.2 |
2000IU (F8) |
Negative |
16 years Student |
Rural |
2 18 |
17 Hem B |
141 |
*<1.0 |
9.5 |
FFP 4 units; 2000IU (F9) |
Negative |
‡ WB, whole blood; FFP, fresh frozen plasma; F8, Factor 8; F9, Factor 9
Case presentation 1
A 16-year-old male presented with a complaint of unrelenting bleeding and pain five days following an uneventful VMMC surgical procedure. He had previously returned to the VMMC site immediately after bandage removal 48 hours (on day two) and 96 hours post-operatively (on day four) thereafter for exploration, suturing, application of pressure bandages and prophylactic oral antibiotics.
Past medical history: Upon further enquiry, it was established that the client was an orphan who lived with his aged grandmother. His grandmother mentioned a vague history of two previous hospitalizations for bleeding problems when the client was younger. She had advised the client to inform the medical providers about this before his VMMC, but he refused. He had also declined to do an HIV screening test before his VMMC procedure.
On examination (D5): His general condition was fair, and he was noted to be febrile with a temperature of 38˚C. He had mild pallor, BP 100/62 and pulse 88. The circumcision wound was still bleeding moderately, with haematoma formation, and early signs of infection. There was also mild wound disruption at the frenulum.
Investigations: Over the next 21 days, the client was hospitalized at three different hospital levels - district (one day), regional (10 days) and tertiary (10 days) for further investigations and escalating levels of care and treatment. While in hospital, several blood tests and investigations were conducted, revealing normal Hb (12,9g/dl), elevated WCC (7,49), elevated CRP (11); slightly low platelets (367); PTT 33.7; INR: 1.38; significantly low Factor VIII (10.7 IU/dL); other factors within normal limits.
Diagnosis of haemophilia A: Eighteen days after his VMMC procedure, the client was diagnosed with haemophilia A, based on a deficiency of Factor VIII. A total of 11 doses of Factor VIII were administered over 11 days. Prior to this, management of the client included insertion of a Foley’s catheter, daily reviews and wound dressing with betadine and pressure bandages, intravenous antibiotics (Cefazolin and Flagyl); Oral and intravenous analgesics (Panado; Tramadol) and antifibrinolytic medication (Cyclokapron). The client showed remarkable improvement and all bleeding stopped. The circumcision wound healed well.
Referral to haematologist for expert opinion: Upon discharge from hospital, the client was transferred to the haematology clinic located in the tertiary hospital, under the care of a haematologist for ongoing specialist management and care.
Case presentation 2
A 16-year-old male presented with a complaint of severe and continuous bleeding three days following an uneventful VMMC surgical procedure. He had previously returned to the facility immediately after bandage removal (on day 2) for exploration, suturing, cautery of bleeding vessels and application of pressure bandages due to a similar complaint.
Past medical history: Upon further enquiry, the client’s father disclosed that the boy was a known haemophiliac, who was receiving treatment at a tertiary-level hospital haematology clinic. He and his son admitted that they had failed to disclose his son’s bleeding disorder to the VMMC provider and took full responsibility for the related consequences. The reason for the lack of disclosure was that they feared that due to his haemophiliac status, the boy might be turned away from the clinic and not receive medical circumcision. The father was also fearful that if his son did not receive a medical circumcision, his son would be compelled to go for traditional circumcision in a non-clinical setting, which, taking into consideration his haemophilic status, might have fatal consequences.
On examination: This showed a healthy adult in a good general condition, afebrile, with a BP of 126/70 mmHg; pulse 61 beats / minute; HB 15.6g/dl and weight 50kg. There was active bleeding noted from the circumcision wound.
In hospital follow-up: Following disclosure of the boy’s haemophiliac status, he was referred for admission at a tertiary level hospital, where laboratory investigations revealed Hb = 12,2g/dl; Iron studies: 8.1umol/L; Folate: 33.8nmol/L; PTT 13.6 sec; INR: 1.12; low Factor VIII level (26 IU/dl). He was also given seven doses of Factor VIII over three days. With the administration of intravenous Factor VIII twice a day, there was noticeable progress and all bleeding stopped. Upon discharge both the client and his father were provided with intensive counselling regarding the importance of disclosing the boy’s condition to all medical providers, and the importance of planning elective surgical interventions with the medical providers in order to ensure prophylaxis and address any bleeding complications immediately. As the client is a known haemophiliac, who is under the care of the haematology unit at a tertiary hospital, he was referred back to the haematology unit for ongoing specialist care and management.
Case presentation 3
A 16-year-old male presented with active bleeding five hours following VMMC surgical procedure. Exploration, cauterization and suturing was done. Two days later review of the wound showed a blood-soaked dressing and moderate bleeding. The client was then admitted to hospital to allow investigation for a possible bleeding disorder. The client was stable with no signs of infection
Investigations: He had low Hb (9.5g/dl); prolonged PTT and INR: 1.08; normal Factor VIII level: 141; low Factor IX level: <1.0.
Treatment: While in hospital the patient was reviewed on a daily basis and daily wound dressing was continued. Whilst awaiting the results of the clotting factors, the client was transfused with four units of fresh human plasma (Bioplasma FDP).
With the administration of FDP, there was noticeable progress and all bleeding stopped. Analysis of his clotting factors revealed a deficiency of Factor IX.
Diagnosis of haemophilia B: Seventeen days after the VMMC the client was diagnosed with haemophilia B, based on a deficiency of Factor IX. As he had been transfused with FDP, his clotting profile was to be reviewed again prior to discharge, with weekly monitoring of his clotting profile for three weeks and thereafter monthly.
Outcome and follow-up: Following complete recovery of the circumcision wound, the client was discharged and client was referred to a haematologist in a referral tertiary hospital for ongoing specialist care and management.
Discussion
Globally, the worldwide incidence of bleeding disorders is not well documented. Affecting individuals of all races and ethnic origins, a vast number of patients with haemophilia, or other bleeding disorders, remain undiagnosed – or are diagnosed at a very late stage [12]. Of the inherited bleeding disorders, haemophilia is recorded as one of the most prevalent, with an estimated incidence of 6.6 ± 48 per 100,000 in lower income countries and higher in high- income countries at 12.8 ± 6.0 (mean ± SD) per 100,000 births [12]. Of these, 85% have haemophilia A and 15% have haemophilia B [13-15]. Definitively, haemophilia A occurs in approximately 1 in 5,000 males [13] while haemophilia B occurs in 1 in 30,000 males [13]. In South Africa, approximately 1 in 1,000 people suffers from a bleeding condition and 1 in 5,000 boys are born with haemophilia [13,16]. This report shows an incidence of haemophilia of 1.28 per 100,000 with 66% suffering from haemophilia A and 33% suffering from haemophilia B.
Described in literature as far back as the 12th century, haemophilia is an X-linked genetic deficiency of a coagulation factor. There are three forms of haemophilia, including haemophilia A, which is due to Factor VIII deficiency; haemophilia B which is due to Factor IX deficiency; and haemophilia C which is due to Factor XI deficiency. The coagulating factor deficiency in haemophilia results in failure of blood to clot and therefore a tendency to bleed, after minor or major trauma and surgery. Haemophilia A is the most common of the three affecting approximately one in 10,000 new-born males. In the majority of cases, it is inherited as an X-linked recessive trait, although there are cases which arise from spontaneous mutations. Due to the nature of transmission, men are predominantly affected and display clinical symptoms. In a few cases, women may also be affected and display clinical symptoms. In general, women are obligate carriers, and transmit the disease to their children. Sons always inherit the disease from their mothers. Mothers may pass on carrier status to their daughters, who in turn may pass the disease to their male offspring.
In this paper, three 16-year-old clients from three different provinces in South Africa presented for VMMC services during July 2018. Following detailed questioning and probing after the clients presented with post-operative bleeding, it transpired that all three had a history of prior bleeding tendency which they did not disclose to the VMMC providers pre- operatively, for various reasons. The predominant reason for non-disclosure cited by all three clients was the fear that they would be denied medical circumcision services at the clinical sites. One client (Case 2), stated that he and his father had previously been advised by their medical providers that any surgical procedure would have to be undertaken in a clinical setting to avoid mortality or morbidity. The client stated that within this context, he was fearful that he would be found unfit for medical circumcision and be forced to endure a traditional medical circumcision in a non-clinical setting, which would have been life- threatening for him. The other two clients (Case 1 & 3) feared that they would not be able to access VMMC services if the providers thought that they were not completely well. Notably, these two clients had been raised primarily by their elderly grandmothers, and thus were unaware of much of their medical history or diagnoses. The reluctance of clients to disclose their haemophiliac status/bleeding tendencies echoes findings from Galukande et al, [8] who also describe clients who were aware of their bleeding tendencies but did not disclose this to the VMMC providers pre-operatively.
This paper raises important issues regarding
i. Clients’ fear of revealing previous bleeding tendencies / haemophiliac status – while all three clients indicated prior history of prolonged bleeding following surgical procedures, this disclosure was only made once they were hospitalized and investigated for bleeding disorders post-VMMC. To mitigate this, we recommend education and advocacy for clients suffering from bleeding disorders be included in all VMMC pre-operative counselling.
ii. The social construct in South African society, where children are often raised by elderly grandmothers who may not be able to provide adequate details regarding existing medical conditions or previous medical history. This poses serious challenges for medical providers, and may lead to life-threatening complications, as is seen in this paper. While addressing this societal norm may be beyond the scope of the medical fraternity to address, it is advisable for all VMMC providers to maintain a high index of suspicion for bleeding disorders, particularly in adolescent boys who often present to VMMC services with their friends and older relatives, who may not be aware of their medical conditions.
iii. Cultural practices including traditional male initiation / circumcision, which serves as a rite of passage for adolescent boys to manhood in several cultural groups within South Africa. All males diagnosed with bleeding disorders should be warned of the manifold dangers of being circumcised in a setting where blood and blood factor products and transfusions are not easily available, and where there is little to no monitoring of bleeding post-operatively. This may be ultimately fatal. It is also recommended that traditional surgeons be trained on the importance of conducting thorough pre-operative history-taking and physical assessments to rule out bleeding disorders in potential clients.
iv. The importance of educating staff working at haematology clinics about the dangers of elective surgical procedures, particularly VMMC, which is performed at various sites nationwide. It would be essential for all clinic staff to understand the importance of counselling male clients and their families about planning for VMMC within well-resourced medical sites by providers who are experienced in dealing with haemophiliac clients. It would also be critical for all staff to check for understanding of limitations by clients following this counselling, as there may be differences in interpretation of the message being given.
v. HIV testing is recommended as an essential part of the VMMC program. In these three cases, all the clients declined HIV testing, which may have identified clients at risk due to continued oozing post pricking / post-HIV testing.
vi. This case also highlights the critical issues of orphans and vulnerable children and adolescents who may be raised by a caregiver who is unaware of their medical conditions and risk factors.
vii. Family counselling is critical, following a definitive diagnosis of Haemophilia in males. The implications for male relatives should be explained in detail. Counseling and advice on diagnosis and management should be offered for patients with haemophilia and their families.[17] It is vital for patients to understand the importance of reporting all bleeding occurrences to their healthcare providers.
Limitations
Only clients from the 14 districts in 6 provinces where the PEPFAR-funded USAID VMMC Project implemented services were considered for this report.
Conclusions
The cases presented in this paper illustrate the occurrence of a rare but potentially severe life-threatening morbidity, which may only be diagnosed post medical male circumcision procedure, if clients fail to disclose their disease earlier. It is therefore critical for all providers to receive clinical VMMC training which includes information regarding the occurrence of significant comorbidities, such as bleeding disorders. It is also important for all clinicians to take a thorough medical, surgical and family history of personal or familial bleeding disorders / diathesis from each client, pre-operatively and during clinical screening. Clinical VMMC protocols guiding post-operative wound management, adverse event management, active client follow-up and care need to be reinforced, with rigorous reporting. It is also important for all providers to have a high index of suspicion in cases of uneventful circumcisions where clients come back repeatedly complaining about post-operative bleeding, where no obvious source of active bleeding is found.
In view of the occurrence of these cases and the observed health system challenges encountered, the following recommendations are made: i) There is need for improved communication within the public health care facilities in order to eliminate delays in patient management; ii) follow up rates should be enhanced for the VMMC program thorough rigorous patient management and prompt follow up review; iii) post-operative care protocols should be strengthened to address the postoperative care of patients who present with bleeding disorders after the surgical procedure through re-enforced health promotion focusing on wound care, early health-seeking behavior, personal hygiene, avoidance of coital interaction and strenuous exercises to ensure complete and speedy recovery.
Implications for training
All clinicians undergoing VMMC training must be educated about the importance of taking a thorough medical history regarding previous surgery / prolonged bleeding post-surgery. A family history regarding haemophilia / prolonged bleeding in other family members, especially men is critical, as this will serve as a warning sign.
Acknowledgements
USAID VMMC III project implementing partners, Department of Health, USAID, PEPFAR. The Funding was provided by USAID/ PEPFAR under contract number AID-674-H-17-00002.
Author contribution
DJ: conceptualized paper, drafted and completed article FD: verification of data and review of article
CV: review and editing of article
MM: investigation of cases and review of article RM: investigation of cases and review of article
JN: conducted the descriptive analysis and substantial review of article All authors reviewed and approved the final manuscript.
References
- Davis SM, Hines JZ, Habel M, Grund JM, Ridzon R, et al. Progress in voluntary medical male circumcision for HIV prevention supported by the US President’s Emergency Plan for AIDS Relief through 2017: longitudinal and recent cross-sectional programme data. BMJ Open. 2018; 8: 1-9.
- Siegfried N, Muller M, Deeks JJ, Volmink J. Male circumcision for prevention of heterosexual acquisition of HIV in men. Cochrane Database Syst Rev. 2009; CD003362.
- PEPFAR. PEPFAR latest global results.
- South Africa Government. National Strategic Plan for HIV, TB and STIs 2017-2022. https://www.nsp.sanac.org.za. 2020.
- WHO. Male circumcision quality assessment toolkit. 2020.
- Population Services International. Adverse Event Action Guide for Voluntary Medical Male Circumcision by Surgery or Device, 2nd Edition. 2018.
- Seretse D, Cherutich P, Nkhata A, Come J, Anyolo E, et al. Voluntary medical male circumcision - Southern and Eastern Africa, 2010-2012. MMWR Morb Mortal Wkly Rep. 2013; 62: 953-957.
- Galukande M, Kahendehe C, Buuza E, Sekavuga DB. A rare but important adverse event associated with adult voluntary medical male circumcision: prolonged bleeding. Int J Emerg Med. 2015; 8: 8.
- Hinkle LE, Toledo C, Grund JM, Byams VR, Bock N, Ridzon R, Cooney C, et al. Bleeding and blood disorders in clients of voluntary medical male circumcision for HIV prevention – Eastern and Southern Africa, 2015-2016. MMWR Morb Mortal Wkly Rep. 2018; 67; 337-339.
- Sgaier SK, Reed JB, Thomas A, Njeuhmeli E. Achieving the HIV Prevention Impact of Voluntary Medical Male Circumcision: Lessons and Challenges for Managing Programs. PLoS Med. 2014.
- UNAIDS and WHO. Voluntary medical male circumcision. 2019.
- Fedhealth. Haemophilia - The facts. 2020.
- Kliegman R. Nelson Textbook of Pediatrics. 19th ed. Philadelphia: Saunders. 2011.
- National Hemophilia Foundation. Types of bleeding disorders. 2020.
- World Federation of Hemophilia. Annual global survey 2015.
- Stonebraker JS, Bolton-Maggs PHB, Michael Soucie J, Walker I, Brooker M. A study of variations in the reported haemophilia A prevalence around the world. Haemophilia. 2010; 16: 20-32.
- Coppola A, Capua MD, Di Minno MND, Di Palo M, Maronne E, Lerano P, Artuto C, et al. Treatment of hemophilia: A review of current advances and ongoing issues. J Blood Med. 2010; 1: 183- 195.