Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
Typical, rare and atypical CT findings in COVID-19 pneumonia: A pictorial review
Charlotte M Biebaû*; Adriana Dubbeldam; Johan Coolen; Johny A Verschakelen; Walter De Wever
Department of Radiology, University Hospitals Leuven, Leuven, Belgium.
*Corresponding Author: Charlotte M Biebaû
Department of Radiology, University Hospitals
Leuven, Leuven, Belgium.
Email: charlotte.biebau@uzleuven.be
Received : Jun 18, 2021
Accepted : Jul 27, 2021
Published : Jul 30, 2021
Archived : www.jcimcr.org
Copyright : © Biebaû CM (2021).
Abstract
Objectives: The objective of this pictorial review is to make radiologists and clinicians familiar with the typical, atypical and rare CT findings of COVID-19 pneumonia to help in diagnosis as well as in monitoring disease.
Main text: Bilateral ground-glass opacities, whether isolated or coexisting with consolidations, and typically in basal, posterior and peripheral lungs are the key findings in COVID-19 pneumonia. With further analysis other typical, atypical and rare CT findings are described and we need to keep in mind that the radiological presentation is dynamic with a rapid evolutive phase, peaking at 10-11 days, and a subsequent absorption phase after 14 days with a decrease in opacities and increase in repairing signs.
Conclusion: The presence of typical findings of COVID-19 pneumonia on a chest CT scan during the pandemic outbreak of SARSCoV-2 helps in diagnostic analysis. Chest CT scan has a reported sensitivity of 97-98% in times with a high pre-test probability. Some CT findings (crazy paving pattern and pleural effusion) as well as an increasing percentage of lung opacities are associated with a worse patient outcome, emphasizing the role of chest CT in determining the risk of disease progression. Furthermore chest CT scan is also useful in monitoring disease control. With these acknowledgement we want to give a useful overview of the chest CT manifestations in COVID-19 pneumonia to help decision making in daily practice.
Keywords: COVID-19; SARS-CoV-2; tomography; X Ray computed; diagnosis.
Abbreviations: CT: Computed Tomography; SARS-Cov-2: Severe Acute Respiratory Syndrome Coronavirus 2; COVID-19: Coronavirus Disease 2019; GGO: Ground-Glass Opacities; RT-PCR: Real Time Reverse Transcription Polymerase Chain Reaction.
Key points: - To make radiologists familiar with the typical CT
findings of COVID-19 pneumonia who are helpful in diagnosis during the pandemic outbreak of
SARS-CoV-2 virus.
- Atypical and rare CT findings of COVID-19 pneumonia may be present, making the diagnosis
more difficult to distinguish from other lung diseases (e.g. pulmonary oedema, intra-alveolar
haemorrhage caused by small vessel vasculitis,
drug-induced pneumonitis and other pneumonias).
- There are many characteristic signs of COVID-19
pneumonia but they can be present in other diseases as well.
Citation: Biebaû CM, Dubbeldam A, Coolen J, Verschakelen JA, Wever WD. Typical, rare and atypical CT findings in COVID-19 pneumonia: A pictorial review. J Clin Images Med Case Rep. 2021; 2(4): 1248.
Introduction
The recent pandemic outbreak of the highly contagious severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) caused a worldwide diagnostic challenge to give a reliable, practical and rapid method to diagnose COVID-19 pneumonia in time of a significant amount of pressure on the health care institutions [1-3]. RT-PCR has an estimated sensitivity of 60-70% [4-7], and can be falsely negative when the viral load is low in contrast to chest CT which can demonstrate suggestive findings at that time [1,2,4-10]. In this regard chest CT scanning can be helpful in diagnosis, and the coronavirus disease 2019 (COVID-19) Reporting and Data System is therefore a well-used categorical assessment scheme in predicting COVID-19 in patients with moderate to severe symptoms [11]. However we need to emphasize that recognition of the typical CT features of COVID-19 pneumonia has to be interpreted in a setting of reporting at a time where pre-test probability of COVID-19 is high (high community disease burden) [2,7]. Earlier studies report a sensitivity of 97-98% [1,5-7,9,10,12] in these circumstances, but the sensitivity is probably much lower when the pre-test probability is lower. This assumption together with the relatively low negative predictive value and specificity are probably the reasons why chest CT scan has never been proposed by any society for routine screening [2,3,7,12-14]. Chest CT scanning is only used for the purpose of estimating the risk of disease progression and for medical triage of patients with suspected COVID-19 who present with moderate to severe clinical features in accordance to the Fleischner Society Statement on Chest Imaging and COVID-19 [2-4,7,15]. Earlier evidence underlines the importance of the determination of the lung injury in the baseline chest CT and the 1st follow-up CT as prognostic tool [16]. Finally, chest CT scan can be used for disease monitoring or when complications (e.g. myocardial injury, pulmonary embolism, bacterial superinfection,…) are suspected [1,2,7,13,15]. The principal differential diagnosis includes other viral pneumonias (especially influenza), pulmonary edema, intra-alveolar hemorrhage and acute lung injury patterns, in particularly organizing pneumonia (idiopathic or secondary to infections, radiotherapy or druginduced pneumonitis) [3,7,12].
The aim of this pictorial review is to give a good overview of all the typical, rare and atypical CT findings in COVID-19 pneumonia based on a comprehensive literature review and the CT experience in our institution to help interpreting Chest CTs and making a quick and accurate diagnosis. All of the shown examples are COVID-19 confirmed cases by means of RT-PCR assay on respiratory specimens.
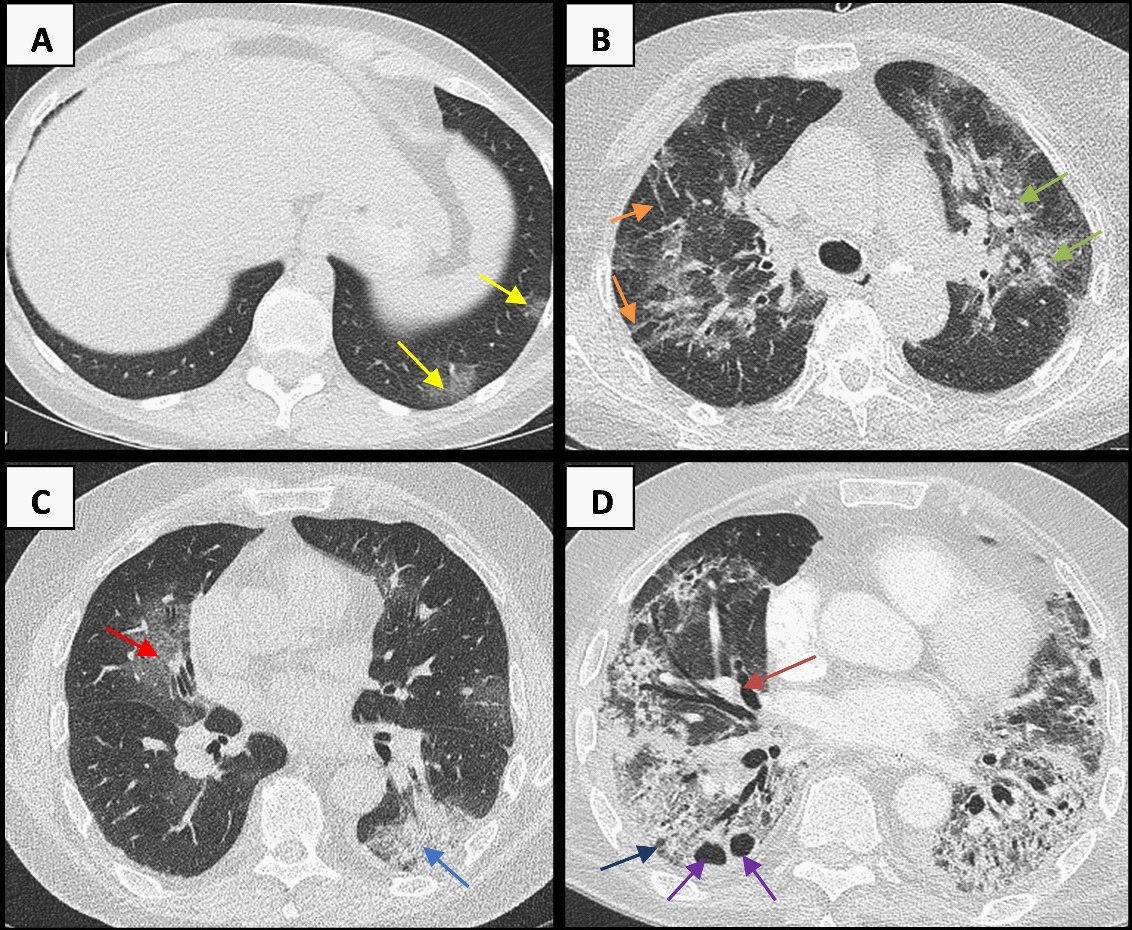
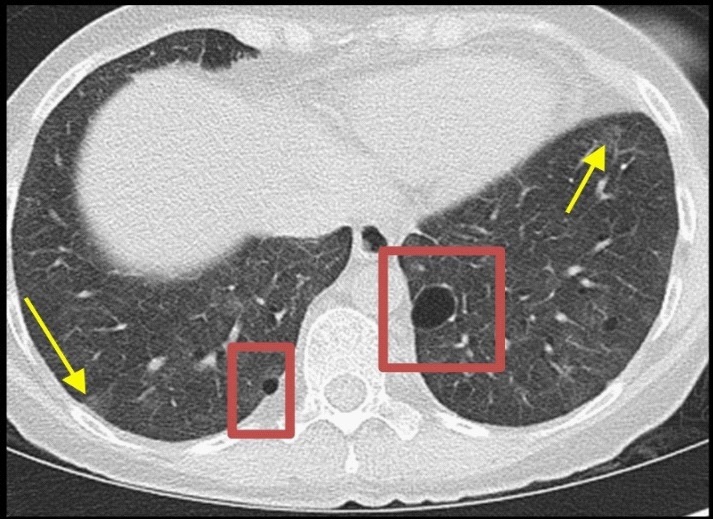
Typical CT findings
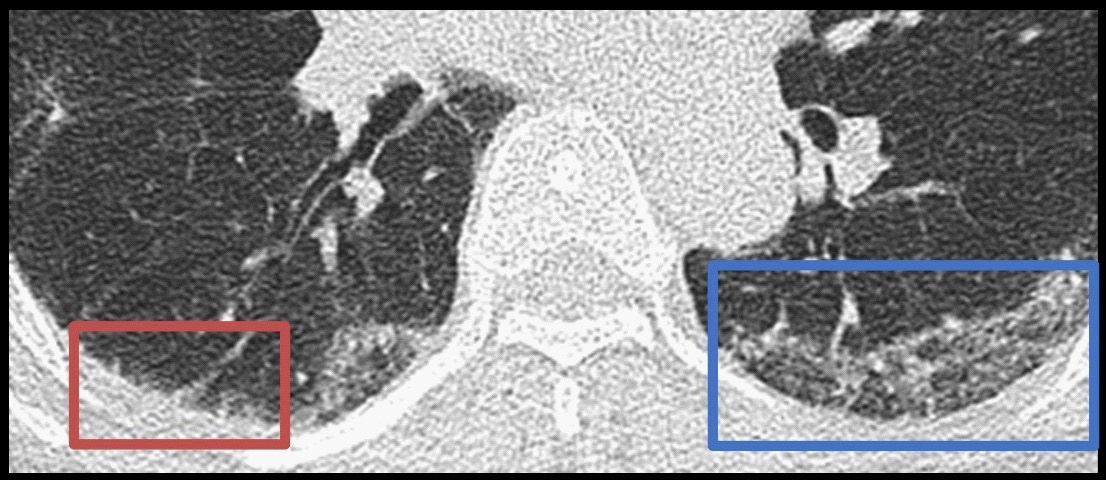
Bilateral ground-glass opacities are frequently (in up to 98%) encountered in patients with COVID-19 infection [1,17]. GGOs are defined as areas of increased opacification of the lung parenchyma without obscuring the underlying pulmonary vessels [1,10,18]. In COVID-19 pneumonia they typically appear as hazy nodular structures, predominant in the peripheral and lower parts of the lungs, which diverge to larger areas and extend along the peribronchovascular bundle later on (Figure 1) [3,12,13,17-21]. The pathologic cause of GGOs in COVID-19 pneumonia is probably a combination of partial filling of the airspaces and thickening of the interlobular interstitium caused by pulmonary edema and hyaline membrane formation [1,19]. The endobronchial spreading virus infects type II alveolar epithelial cells via ACE2 receptors [1,15] causing cellular apoptosis in alveolar cells and subsequent release of viral particles to infect neighboring cells [4]. The subsequent release of proinflammatory cytokines causes inflammatory reactions in the alveoli and interstitium leading to exudation into the alveolar space with diffuse alveolar damage and fibrin-rich hyaline membranes causing the opacities in COVID-19 pneumonia [4].
In the areas of ground-glass opacification frequently (in up to 64%) a prominent vascular structure can be visualized, defined as vascular dilatation (Figure 2) [1,4,10]. This may correspond to the in earlier studies reported vascular wall damage and thickening by pro-inflammatory factors as well as the intraluminal thrombogenic material in the injured small lung vessels, resulting in a larger caliber of the vessels and subsequently angiogenesis [1,19,22].
Consolidations, defined as areas with complete opacification of the airspaces and with obscuration of underlying vessels [1,10,18], are formed with disease progression (in up to 64%) [1]. In COVID-19 pneumonia they typically appear in the peripheral lungs and have a more irregular nodular or linear aspect which diverge to more circumscribed, segmental or lobar consolidations later on [1,17,18,20,21]. They might be related to cellular fibromyxoid exsudates filling the alveoli [1,23,24]. A higher total lung involvement (% opacities) and a higher grade of dense opacities is predictive for a more severe outcome [4,9,15,25].
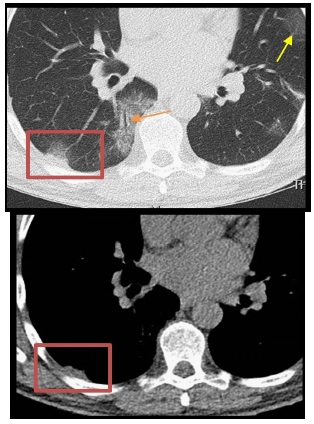
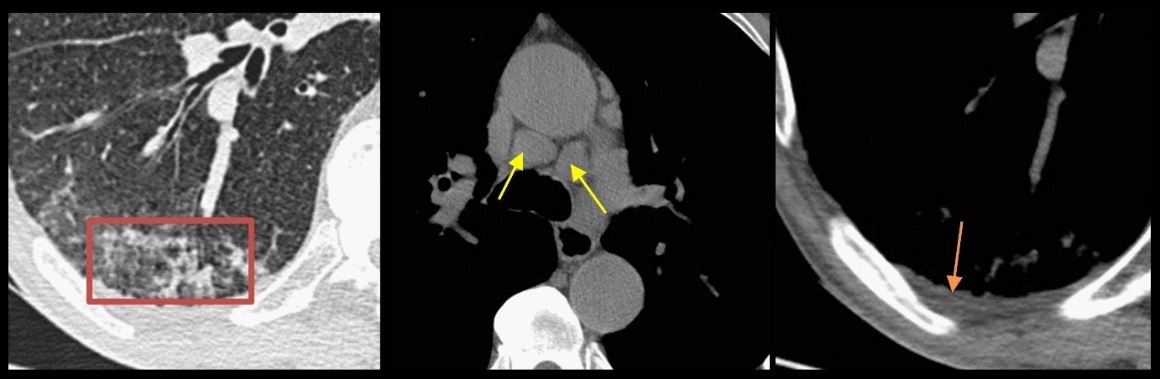
The linear opacities (Figure 3) appear as small bands running almost perpendicular to the pleural surface and can be distinguished from the subpleural bands lying parallel to the pleural surface. The linear consolidations and the reversed halo sign are typical for an organizing pneumonia pattern [13].
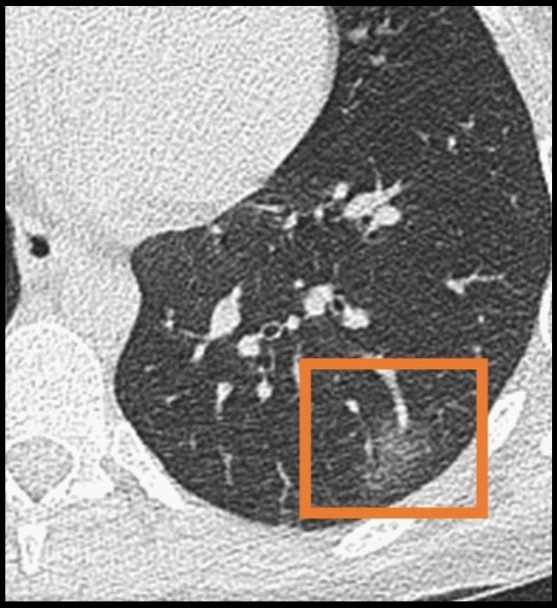
Blurred bounded nodular opacities (Figure 4) are formed within the areas of ground-glass opacity [18]. Sometimes a small air containing spot (< 5 mm) can be seen which have been described in the literature as the air bubble sign or vacuolor sign [1,4,10]. This last may be due to the incomplete filling of the alveoli [10].
Subpleural bands or the parallel pleura sign, defined as thin curvilinear strands (1-3 mm thickness) lying subpleural and parallel to the pleural surface (less than 1 cm from the pleural surface) and typically in the lower parts of the lungs, are frequently noted in chest CTs of COVID-19 proven patients (Figure 5) [1,19]. This finding is reported in 20-25% of cases [1] and is very characteristic but not specific for COVID-19 pneumonia. It can also be seen in some interstitial lung diseases and it mimics hypoventilation strands. They might be related to pulmonary oedema or fibrosis of COVID-19 pneumonia [1]. The lymph drainage of the interlobular interstitium, especially the perialveolar interstitium, is directed toward the subpleural space and the interlobular septum which can be an explanation for the orientation of these subpleural bands and likewise the lower described subpleural reticulation seen in COVID-19 pneumonia [19].
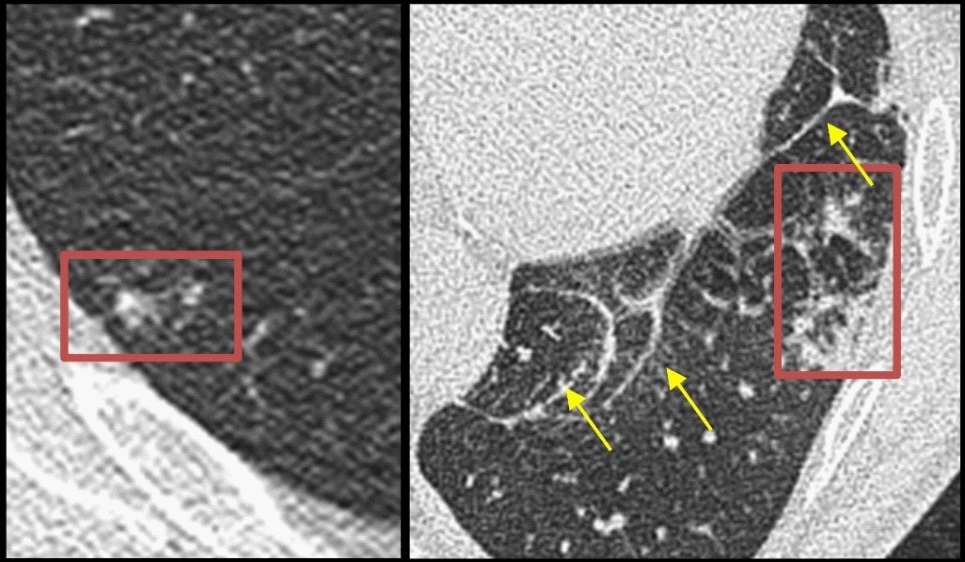
Subpleural reticulation is a type of reticular interstitial pattern where the thickened interlobular septa and intralobular septa, are located in the peripheral lungs (Figure 6). They might be related to interstitial lymphocyte infiltration [1]. It’s reported in up to 22% of cases [1,4,18] and the prevalence is assumed to be higher in long-standing disease [1]. The presence of the parallel pleura sign and subpleural reticulation are very characteristic for COVID-19 pneumonia but they are not specific and can be present in other interstitial lung diseases as well (e.g. NSIP, UIP). It has been assumed that aberrant healing mechanisms are triggered, causing a scarring of the epithelium and consequently patchy fibrosis [4].
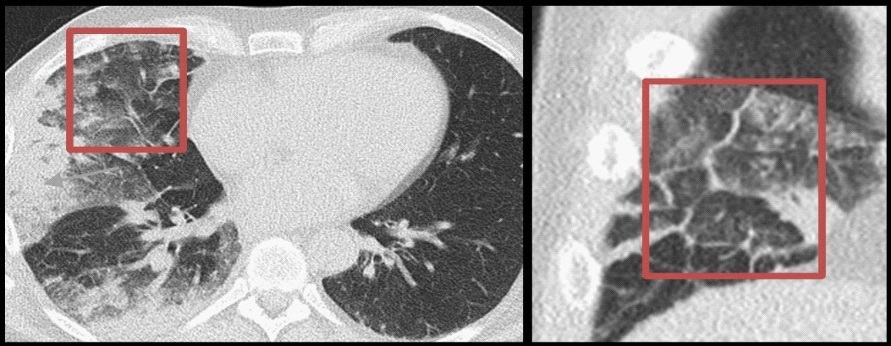
In average 19.5% (5~36%) of COVID-19 proven cases, a crazy paving pattern is founded on Chest CT [1,4,18,25]. Crazy-paving pattern is defined as areas of ground-glass opacity with superimposed interlobular and intralobular septal thickening, resembling paving stones (Figure 7) [1,10]. This pattern is noted in the more advanced stadia of COVID-19 pneumonia and is suggestive for disease progression [1,9,13,15] and a worse patient outcome as mentioned in earlier studies. They might be related to pulmonary oedema and the interstitial inflammatory reaction of COVID-19 pneumonia [1].
In COVID-19 pneumonia frequently a subtle focal pleural thickening adjacent to the peripheral opacities, with or without a pleural retraction sign, can be visualized (Figure 8). This focal pleural thickening is noted in earlier studies in up to 41.7 % of patients with COVID-19 pneumonia [1,4,26].
An air bronchogram refers to the appearance of air-filled bronchi on a basis of GGOs and/or consolidations and is reported in 41.2% of COVID-19 pneumonia (Figure 9) [1,4]. It’s a non-specific sign of COVID-19 pneumonia and and can be present in other lung pathology as well (e.g. pulmonary infections, interstitial lung diseases, pulmonary oedema, pulmonary infarct, pulmonary haemorrhage and neoplasms). Recent autopsy reports in COVID-19 patients are mentioning a gelatinous mucus substance in the bronchi, so maybe the air bronchogram reflects the presence of a gelatinous mucus instead of air in the bronchi, causing the insufficient sputum mobility and subsequent ‘dry cough’ in COVID-19 pneumonia [1]. It’s more frequently present in the more advanced stadia of COVID-19 pneumonia and is often associated with a slightly bronchiolar dilatation in the opacities [1].
Overview of the CT findings in COVID-19 pneumonia |
||
|
||
Typical CT findings |
Ground-glass opacities |
|
|
Consolidations
|
|
|
Vascular dilatation |
|
|
Subpleural bands |
|
|
Subpleural reticulation |
|
|
Crazy paving pattern |
|
|
Focal pleural thickening |
|
|
Air bronchogram |
|
|
||
Rare CT findings |
Halo sign |
|
|
Bronchial wall thickening |
|
|
Bronchiectasis |
|
|
Reversed halo sign |
|
|
Cysts |
|
|
Pneumatoceles |
|
|
||
Atypical CT findings |
Centrilobular nodules |
|
|
Mucoid impactions |
|
|
Pleural effusion |
|
|
Enlarged lymph nodes |
|
|
Tree-in-bud opacities |
|
|
Cavitation |
|
Evolution of chest CT findings of COVID-19 pneumonia in time
The characteristic radiological presentation of COVID-19 pneumonia is that of bilateral and frequently multilobular ground-glass opacities (GGOs), whether isolated or coexisting with consolidations, and typically in basal, posterior and peripheral lungs [1,3,4,8-10,13,17-19,21,23,24,26]. As in earliest studies reported, the predominant peripheral and basal distribution may be due to the fact that the endobronchial spreading virus invades bronchioles and alveoli, causing bronchiolitis and subsequently inflammatory reactions in the alveoli and interstitium which needs the participation of blood vessels and lymphatics who are more abundant in the peripheral and lower areas of the lungs [10,19]. The large airways are less affected due to its better viral clearance (abundant cilia and strong immune function) [19].
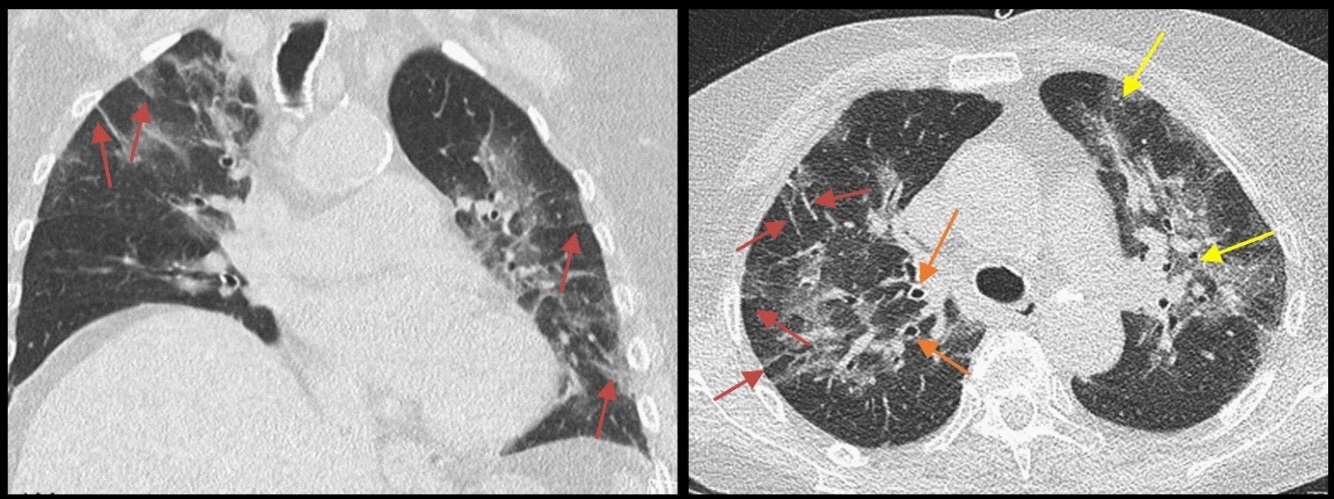
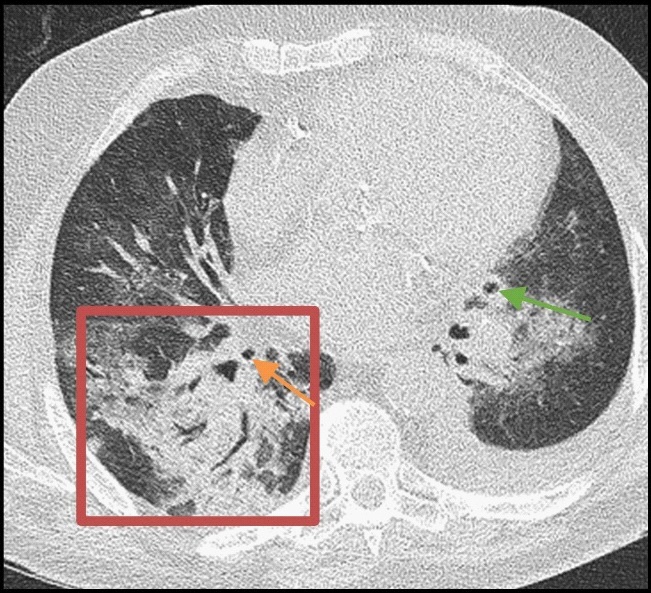
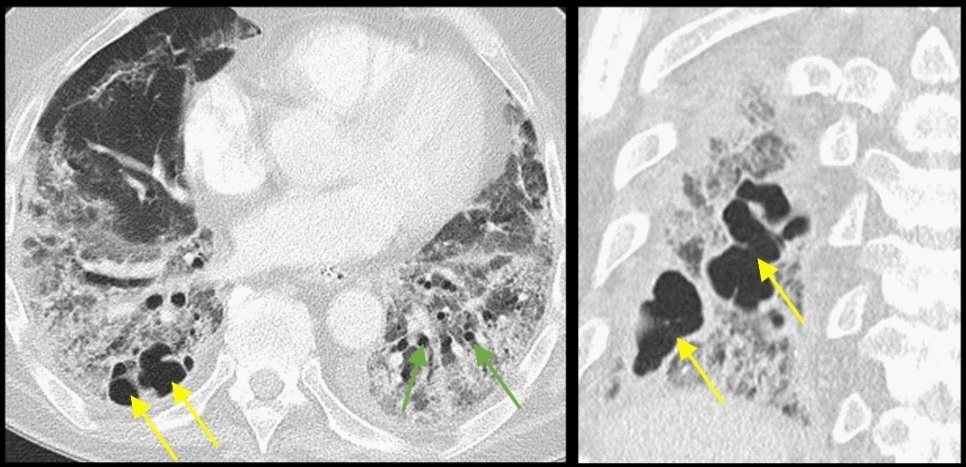
The appearance of COVID-19 pneumonia is depending on the time between symptom onset and the CT scan [4,9,10,17,18,26]. The first two days after symptom onset, there are no CT findings in more than 50% of cases [3,4,9,12,13]. After a few days hazy nodular GGO appear in a peripheral lobular distribution and typically with a lower and posterior predominance (Figure 10a) [4,10,12,13,17,21,26,28]. With disease progression, the ground-glass opacities diverge while spreading along the bronchovascular bundles and consolidations are formed [3,10,19,21,28], peaking at 10-11 days, frequently starting with a peripheral nodular or linear aspect of the consolidations (Figure 10b) [4,9,10,17,18,26,28]. A crazy paving pattern appears in the GGOs as well as a halo sign around the nodular opacities or a reversed halo sign around the GGOs [1,9,10,19,21,28]. In the more advanced stages multifocal, patchy or more circumscribed segmental consolidations are formed (Figure 10c) [10,19,21,26]. Most often there is a gradual decreasing trend after 14 days, the absorption phase, with a decline in the grade of opacities and an increase in repairing signs or the formation of organization (subpleural bands, interlobular and intralobular septal thickening, bronchus distortion) [3,4,9,10,19,21,26]. Asynchronous patterns are described, meaning that some lesions are resolving while other lesions are enlarging or newly formed at the same time causing persistent patchy opacities [10,19]. In a few patients aberrant healing mechanisms are triggered which cause scarring of the epithelium and consequently fibrosis [4,19]. Severe/critical patients who are intubated for a long time can evolve pneumatoceles, patchy fibrosis and tractive bronchiectasis (Figure 10d) [3]. In patients with clinical worsening without extension of lung opacities, pulmonary embolism or acute myocarditis should be excluded [2,9].
Younger people tend to have more, typically nodular GGOs while older patients and sicker patients tend to have more extensive multilobar lung involvement and a higher occurrence of consolidations, architectural distortion, bronchiectasis, subpleural lines, lymphadenopathy, pleural effusion and pleural thickening [3,4,21].
Rare findings
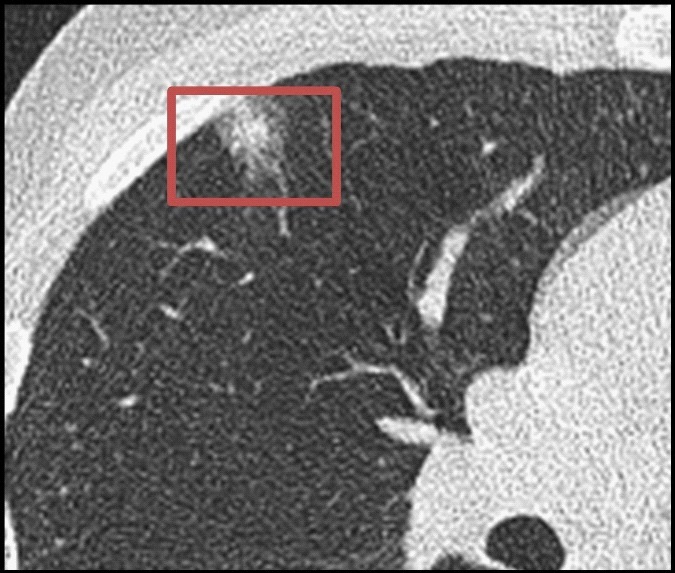
The “Halo sign” refers to a nodular or mass like consolidation surrounded by ground-glass opacity representing adjacent hemorrhage in angio-invasive aspergillosis, hypervascular metastases, viral infections, vasculitis and organizing pneumonia (Figure 11) [1,19]. It’s reported in up to 11% of COVID-19 pneumonia cases [4]. To date the pathological cause of this sign remains unknown [1]. Hypothetical the sign can reflect hemorrhagic alterations around the opacity or the spread of the inflammatory process towards the surrounding interstitium [19].
Bronchial wall thickening is noted in around 10-20% of cases and is probably due to the inflammation of the bronchial wall and the bronchial obstruction caused by the endobronchial spreading infectious process [1,3].
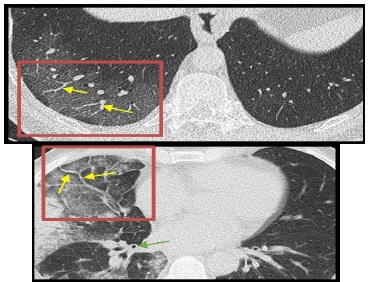
Bronchiectasis is a rare finding in COVID-19 pneumonia and is reported in up to 18%, typically in the severe/critical patients (Figure 12) [1,4,19]. Bronchiectasis is defined as the irreversible dilatation of the bronchi, usually associated with inflammation of the bronchial wall and proliferation of fibrous tissue progressing to fibrosis and tractive bronchiectasis [1]. A wide variety of lung diseases may result in bronchiectasis, the most common of which is infection. Other causes include Cystic Fibrosis (CF), Allergic Bronchopulmonary Aspergillosis (ABPA), chronic aspiration and air way obstruction.
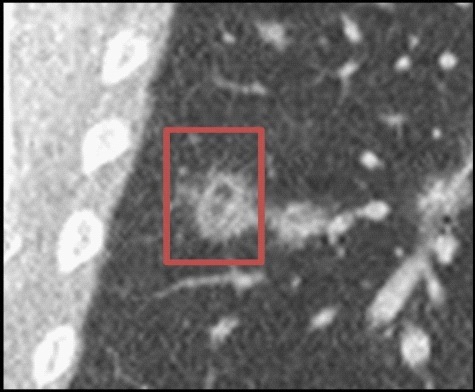
The ‘reversed halo sign’ or ‘atoll sign’, defined as a ring-like consolidation around a rounded ground glass opacity (Figure 13), can be seen in cryptogenic organizing pneumonia as well as in certain infections (e.g. tuberculosis), postradiotherapy, vasculitis, COP or in pulmonary neoplasms [1,19,27]. It’s a rare but characteristic sign of COVID-19 pneumonia and is reported in up to 2.4-5.1% of cases [3,4]. A possible suggestion is that these sign may reflect the inflammatory repair at the edges of the lesions [19].
Cysts are smooth, thin walled structures that are likely related to dilated airspaces from obstruction of the distal bronchioles. They are very rare in COVID-19 pneumonia with just a few case reports in the literature [24,26]. In our institution there was only one confirmed COVID-19 case with cystic alterations on chest CT with presentation (Figure 14).
Atypical findings
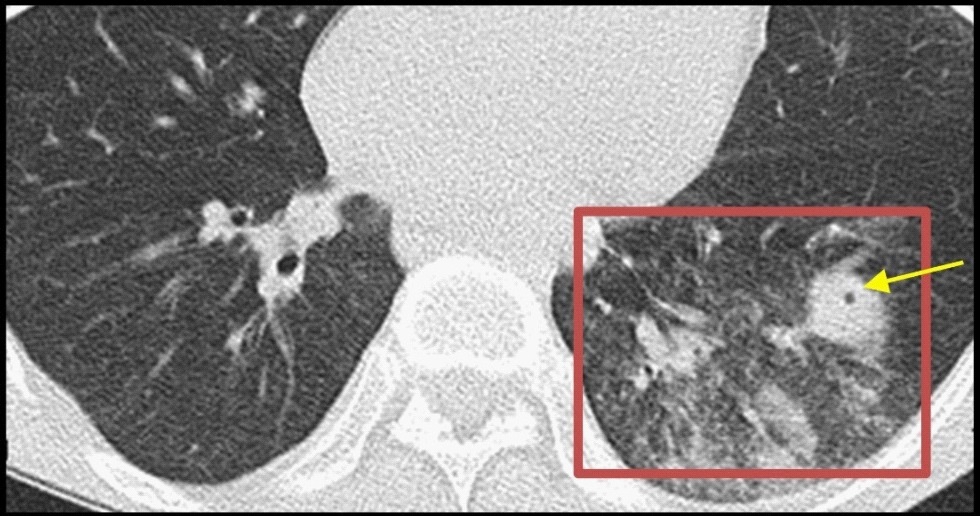
Centrilobular nodules are millimetric, mixed or purely solid/ ground-glass nodules, occurring in the centre of the secondary pulmonary lobule and in a centrilobular distribution pattern with sparing of the subpleural space (Figure 15). In a smoker they typically indicate respiratory bronchiolitis. In a non-smoker they can indicate a hypersensitivity pneumonitis, but any cause of bronchiolitis or vasculitis can cause centrilobular nodules. They are more atypical in COVID-19 pneumonia, reported in average 7.8% (3 ~13% ) of cases, but can be present when there is a bacterial superinfection or with concomitant miliary metastases [1,4].
Pleural effusion and enlarged lymph nodes (Figure 15) are more atypical for COVID-19 pneumonia but can be present, representing bacterial superinfection or cardiac strain (possibly secondary to acute myocarditis or pulmonary embolism caused by COVID-19 infection) [13]. The combination of enlarged lymph nodes, pleural effusion and extensive millimetric nodules may suggest bacterial superinfection or (chronic) aspiration pneumonia [1,9]. Pleural effusion is reported in up to 5% and lymphadenopathy in 4-8% of cases [1,4]. The presence of pleural effusion suggests a more severe outcome [1,4,26].
Bronchial mucus plugs are not typically observed in COVID-19 pneumonia but can suggest bacterial superinfection [9,12].
Centrilobular branching nodules, or tree-in-bud opacities, almost always represent inflammation and fluid-filling of the small airways (Figure 16). The most common causes are infection or aspiration. Tree-in-bud pattern is reported in COVID-19 pneumonia but it’s a rare finding who is more suggestive for other viral, bacterial, fungal or mycobacterial infections [19]. Even more tree-in-bud pattern can be present in organizing pneumonia and invasive adenocarcinoma and can be mimicked by tumor emboli in de distal pulmonary arteries and veins.
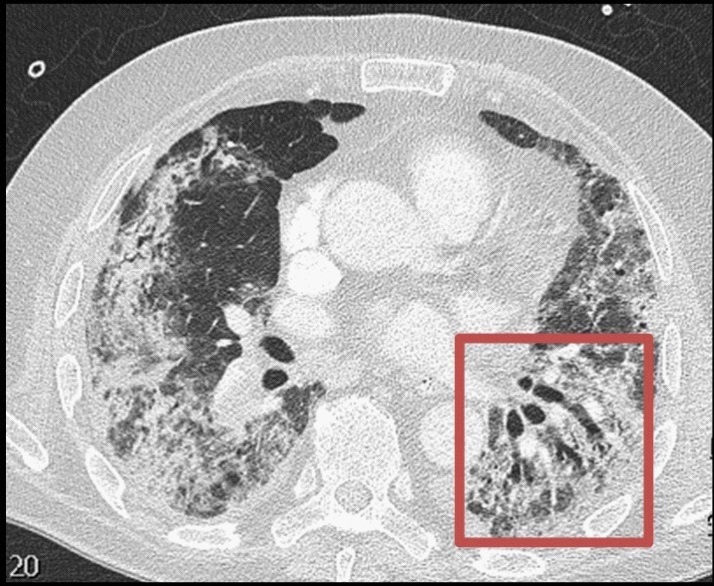
Lung parenchymal necrosis with cavitation (Figure 17) is very rare in COVID-19 pneumonia [23] and is reported in average 0.1% of cases [4]. Cavitations occurs more commonly in virulent bacterial pneumonias (e.g. S. aureus, S. pneumoniae, gram negative bacilli and anaerobic bacteria) [12] or other cavitating lung diseases (e.g. cavitating malignancy, granulomatous disease, pulmonary infarction). With central liquefaction in a lung abscess a communication with the bronchus can be formed, resulting in a cavity. Pneumatoceles can occur in patients with COVID-19 pneumonia [19,26], either from alveolar rupture (e.g. by mechanical ventilation with positive airway pressure [24]) or in an area of necrosis and cavitation in the more advances stages of COVID-19 pneumonia who are intubated for a long time.
The appearance of ground-glass opacities in a predominant peripheral and basal distribution is the most characteristic and usually the first radiological finding in COVID-19 pneumonia. They usually start as hazy nodular GGO who diverge at time. Later on other typical findings like vascular dilatation, repairing signs (subpleural band, subpleural reticulation and crazy paving pattern), a focal pleural thickening with or without pleural retraction sign and air bronchogram can appear. A rare and characteristic, but not specific sign of COVID-19 pneumonia is the ‘reversed halo’ sign. Atypical signs like centrilobular nodules, enlarged lymph nodes and pleural effusion are more suggestive for other pathologies but they can occur in COVID-19 pneumonia, typically secondary to bacterial superinfection or cardiac strain of which the last can be the result of acute myocarditis or pulmonary embolism secondary to COVID-19 infection.
The presence of these typical findings of COVID-19 pneumonia on a chest CT during the pandemic outbreak of SARS-CoV-2 helps in making the diagnosis with a reported sensitivity in up to 97-98% according to the recent literature [1,5,6,7,9,10,12]. However further analysis is necessary to confirm this high sensitivity in times when the virus is not endemic in the region or in times that other viral respiratory infections are circulating.
Declarations
Ethics approval and consent to participate: Ethics approval was obtained by the Ethics Committee Research UZ/KU Leuven. Written informed consent was waived by the Institutional Review Board.
Consent for publication: Not applicable.
Availability of data and materials: The figures and data that support the findings in this pictorial review are available on request from the corresponding author.
Competing interests: The authors declare that they have no competing interests.
Funding: There are no Funding Sources.
Author’s contributions: CB is the corresponding author who has written the pictorial review and collected the figures. The other authors read and approved the final manuscript.
References
- Ye Z, Zhang Y, Wang Y, et al. Chest CT manifestations of new coronavirus disease 2019 (COVID-19): A pictorial review. Eur Radiol. 2020; 30: 4381-4389.
- Rubin GD, Ryerson CJ, Haramati LB, et al. The Role of Chest Imaging in Patient Management during the COVID-19 Pandemic: A Multinational Consensus Statement from the Fleishner Society. Radiology. 2020.
- Homsi ME, Chung M, Bernheim A. et al. Review of chest CT manifestations of COVID-19 infection. European Journal of Radiology Open. 2020.
- Ojha V, Mani A, Pandey NN, et al. CT in coronavirus disease 2019 (COVID-19): a systematic review of chest CT findings in 4410 adult patients. European Radiology. 2020; 30: 6129–6138.
- Fang Y, Zhang H, Xie J, et al. Sensitivity of Chest CT for COVID-19: Comparison to RT-PCR. Radiology. 2020.
- Ai T, Yang Z, Hou H, et al. Correlation of Chest CT and RT-PCR Testing in Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology. 2020.
- Kalra MK, Homayounieh F, Arru C, et al. Chest CT practice and protocols for COVID-19 from radiation dose management perspective. Eur Radiol. 2020; 30: 6554-6560.
- Xie X, Zhong Z, Zhao W, et al. Chest CT for typical 2019-nCoV pneumonia: relationship to negative RT-PCR testing. Radiology. 2020.
- Hani C, Trieu NH, Saab I, et al. COVID-19 pneumonia: A review of typical CT findings and differential diagnosis. Elsevier, Diagnostic and Interventional imaging. 2020; 101: 263-268.
- Zhou S, Zhu T, Wang Y, et al. Imaging features and evolution on CT in 100 COVID-19 pneumonia. Eur Radiol. 2020.
- Prokop M, van Everdingen W, van Rees Vellinga T, et al. CO-RADS: A Categorical CT Assessment Scheme for Patients Suspected of Having COVID-19 - Definition and Evaluation. Radiology. 2020; 296.
- Simpson S, Kay FU, Abbara S, et al. Radiological Society of North America expert consensus statement on reporting chest CT findings related to COVID-19. Endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA. J Thorac Imaging. 2020; 35: 219-227.
- Revel M, Parkar AP, Prosch H, et al. COVID-19 patients and the radiology department - advice from the European Society of Radiology (ESR) and the European Society of Thoracic Imaging (ESTI). European Radiology. 2020; 30: 4903-4909.
- ACR recommendations for the use of chest radiography and computed tomography (CT) for suspected COVID-19 infection. 2020.
- Feng Z, Yu Q, Yao S, et al. Early prediction of disease progression in COVID-19 pneumonia patients with chest CT and clinical characteristics. Nature Communications. 2020.
- Huang L, Han R, Ai T, et al. Serial Quantitative Chest CT Assessment of COVID-19: Deep-Learning Approach. Radiology: Cardiothoracic Imaging. 2020.
- Bernheim A, Mei X, Huang M, et al. Chest CT findings in Coronavirus Disease-19 (COVID-19): Relationship to Duration of Infection. Radiology. 2020.
- Chung M, Bernheim A, Mei X, et al. CT imaging features of 2019 novel coronavirus (2019-nCoV). Radiology. 2020; 295: 202–207.
- Wu J, Pan J, Teng D, et al. Interpretation of CT signs of 2019 novel coronavirus (COVID-19) pneumonia. Eur Radiol. 2020; 30: 5455- 5462.
- Pan Y, Guan H, Zhou S, et al. Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): a study of 63 patients in Wuhan, China. Eur Radiol. 2020; 30: 3306-3309.
- Salehi S, Abedi A, Balakrishnan S, et al. Coronavirus disease 2019 (COVID-19): a systematic review of imaging findings in 919 patients. American Journal of Roentgenology. 2020; 215: 87-93.
- Ackermann M, Verleden SE, Kuehnel M, et al. Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in COVID-19. N Engl J Med. 2020.
- Kong W, Argwal PP. Chest Imaging Appearance of COVID-19 Infection. Radiology. 2020.
- Liu K, Zeng Y, Xie P, et al. COVID-19 with cystic features on computed tomography: A case report. Medicine (Baltimore). 2020; 99: e20175.
- Kanne JP. Chest CT findings in 2019 novel coronavirus (2019- nCoV) infections from Wuhan, China: Key points for the radiologist. Radiology. 2020; 295: 16–17.
- Shi H, Han X, Jiang N, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect. Dis. 2020; 20: 425–434.
- Kim SJ, Lee KS, Ryu YH, et al. Reversed Halo Sign on High-Resolution CT of Cryptogenic Organizing Pneumonia: Diagnostic Implications. AJR Am J Roentgenol. 2003; 180:1251–1254.
- Pan F, Ye T, Sun P, et al. Time course of Lung Changes at Chest CT during Recovery from Coronavirus Disease 2019 (COVID-19). Radiology. 2020; 295: 715–721.