Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 3
First case of pulmonary mucormycosis caused by Rhizomucor miehei
Fidaa Maatallah1,2; Latifa Mtibaa1,2*; Hela Stambouli1,3; Nawel Baccouchi2; Hela Ghdira1,3; Hana Souid2; Zriba Sami1,3; Fehmi Msadek1,3; Boutheina Jemli1,2
1 Faculty of Medicine of Tunis, University Tunis el Manar, Tunis, Tunisia.
2 Laboratory of Parasitology-Mycology, Military Hospital of Tunis, 1008 Monfleury, Tunis, Tunisia
3 Department of Hematology, Military Hospital of Tunis, 1008 Monfleury, Tunis, Tunisia.
*Corresponding Author: Mtibaa Latifa
Laboratory of Parasitology-Mycology, Military Hospital of Tunis, 1008 Monfleury, Tunis, Tunisia.
Email: mtibaalatifa@yahoo.fr
Received : Jan 12, 2022
Accepted : Feb 21, 2022
Published : Feb 28, 2022
Archived : www.jcimcr.org
Copyright : © Latifa M (2022).
Abstract
Mucormycosis is a rare and fatal infection that occurs commonly in immunocompromised patients such as those with hematological malignancies. Rhizomucor miehei usually cause bovine mycotic abortion and mastitis and is rarely described in human disease. Here, we report a rare case of pulmonary mucormycosis in a 29-year-old patient with an acute myeloid leukemia. PCR sequencing allowed the identification Rhizomucor miehei species in a bronchial biopsy. The patient died at home following disease progression after 6 months of antifungal therapy with amphotericin B.
Citation: Maatallah F, Mtibaa L, Stambouli H, Baccouchi N, Ghdira H, et al. First case of pulmonary mucormycosis caused by Rhizomucor miehei. J Clin Images Med Case Rep. 2022; 3(2): 1696.
Introduction
Mucormycosis is a life-threatening opportunistic fungal infection caused by fungi of the order Mucorales [1-3]. The most common manifestation is the rhino cerebral involvement and it constitutes almost half of the cases reported in the literature [4-6]. The pulmonary form is rare and observed essentially in patients with hematological malignancies. The disease has a high rate of mortality [7]. Prognosis is bettered with an early diagnosis and multidisciplinary treatment [8]. Here we report a case of pulmonary mucormycosis due to Rhizomucor miehei in patient with an acute myeloid leukemia.
Case report
A 29-year-old woman with a history of acute myeloid leukemia secondary to myelodysplastic syndrome for two years, was admitted in hematology department (day 0) for an intensive salvage therapy. The patient was put on chemotherapy with Fludarabine, high dose of cytarabine and Mitoxantrone. During her hospitalization, she developed fever, dyspnea and signs of sepsis. In biology she had pancytopenia with severe neutropenia. She was put on imipenem, vancomycin and colimycin. On day 11, there was resumption of fever with desaturation in the ambient air and hemoptysis. Due to the worsening of the respiratory symptoms and persistence of fever; chest Computed Tomography (CT) and Aspergillus antigenemia were indicated.
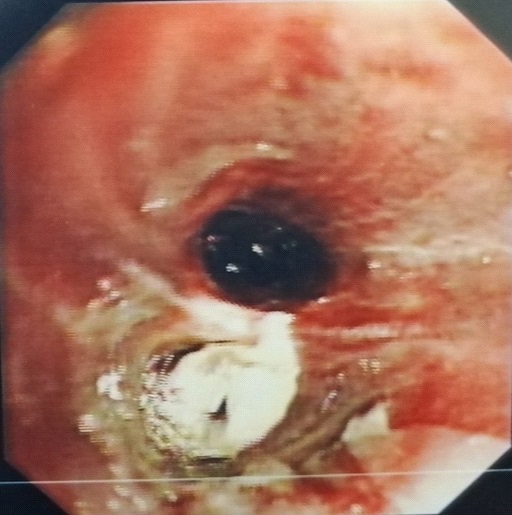
CT revealed intra-alveolar hemorrhages with halo sign causing suspicion of Invasive Pulmonary Aspergillosis (IPA) (Figure 1). Aspergillus antigenemia was negative. The patient was treated with voriconazole without improvement. Bronchoscopy was performed and it visualized an inflammatory and necrotic mucosa with pseudo membranes (Figure 2) that were biopsied. The specimen was sent to the laboratory with suspicion of mucormycosis.
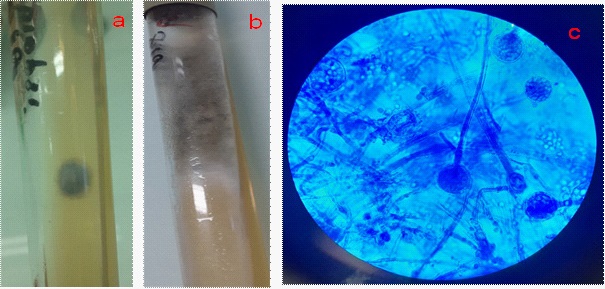
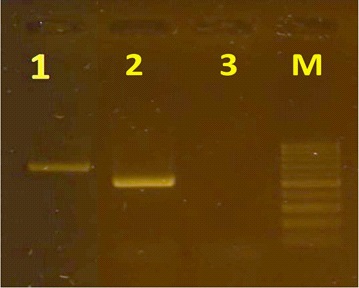
Direct examination of the specimen was negative. The culture on sabouraud medium showed a small greyish colony by aging after 5 days of incubation at 27°C (Figure 3). The microscopic examination allowed to identify Mucor sp (Figure 3). PCR sequencing identifies Rhizomucor miehei species
The diagnosis of pulmonary mucormycosis was carried. An antifongigram by the E-test technique on RPMI medium was made and showed sensitivity to amphotericin B (MIC=0.25 Ug/ ml). However, the strain was resistant to voriconazole (MIC >2 µg/ml), caspofungin (MIC > 32 µg/ml) and fluconazole (MIC >256 µg/ml). The patient was treated by amphotericin B. The evolution was marked by stableapyrexia. At the end of aplasia, chest CT showed multiple bilateral pulmonary abscesses, and bronchial fibroscopy found fistulized abscesses. The patient died at home following disease progression after 6 months of antifungal therapy with amphotericin B.
Molecular diagnosis
DNA was extracted from the fungal colony. The ITS2 region from isolate was amplified by PCR using the following pairs of primers: ITS1 (5’-TCCGTAGGTGAACCTGCGGC-3’) and ITS4 (5’-TCCTCCGCTTATTGATATGC-3’). One fragment of 700 pb was yielded (Figure 4). The sequence of the PCR product was analyzed by BLAST and compared with the published Gene Bank sequences (NCBI data base). It revealed homology with ex-type strain of Rhizomucor miehei.
Discussion
Mucormycosis is a destructive fungal infection that affect mostly diabetic patients and immunocompromised especially having neutropenia [9,10]. Besides diabetes and immunodeficiency, there are other predisposing factors such as renal failure, hepatic cirrhosis, malnutrition, human immunodeficiency virus deficiency and organ graft [11-13].
Its incidence is increasing, on the one hand given the progress of immunosuppressive therapies and chemotherapy and on the other hand the lack of use of antifungal prophylaxis covering the mucorales [14]. The most common clinical presentations of Mucorales infection are rhino cerebral and pulmonary. However neurological, renal, cardiac, cutaneous and disseminated disease are less frequent [2,6,15].
In the order Mucorales, 38 genera have been reported to cause infections in humans [16] with Rhizopus being the most commun genus [17]. Rhizomucor miehei is a rare agent of human disease and its specific epidemiology is unknown. However, the closely related R. pusillus has frequently been reported in human pathology. To the best of our knowledge, this case documents the first isolation of Rhizomucor miehei from a pulmonary specimen (biopsy) and thus further supports evidence for its pathogenicity.
Mucormycosis typically begins in the sinuses or the lungs after inhalation of fungal spores [11]. They penetrate the vessels due to an elastase-type enzyme causing an interaction with endothelial cells [6]. Then the mycelial invasion leads to thrombosis of the vessels, infarction and necrosis of the tissues causing hemorrhage, with eventual spread via the bloodstream to other organs [5,6,12].
The symptoms readily mimic IPA and the diagnosis difficulties are caused by the lack of specificity of the clinical and radiological presentation [2,5]. Mucormycosis usually presents with a persistent fever associated with pulmonary signs such as cough, chest pain, dyspnea and hemoptysis [5,13,18].
CT is the most useful radiological examination [7,19]. It shows images of parenchymal condensations, an excavated appearance, a gas crescent or single or multiple nodules [8,13,20]. The presence of the Reversed halo sign on CT was a strong indicator of pulmonary mucormycosis in several studies [21].
Diagnosis is established based on direct examination or histological study of mycelial filaments. Hyphae of Mucorales have a variable width (6 to 25 μm), are non-septate or pauci-septate and show an irregular, ribbon-like appearance. The angle of branching is variable and includes wide-angle (90°) bifurcations. Periodic acid-Schiff or Grocott Gomori’smethenamine silver staining are used to highlight fungal hyphae and hence to evaluate morphology in more details [22].
Mycological cultures on Sabouraud medium allow precise identification of the responsible fungus. The recommended incubation temperatures are 25°C and 27°C for a minimum of 5 days for optimize growth [13]. Phenotypic identification is based on macroscopic, microscopic and physiological characteristics. In addition, molecular identification by PCR sequencing is useful when phenotypic identification is not conclusive. The majority of the molecular assays target either the internal transcribed spacer (ITS) or the 18S rRNA genes [23-25].
Successful management of mucormycosis is based on a multimodal approach, including antifungal treatment, surgical debridement and correction of risk factors [10,26]. Mucoraceous fungi are resistant to most antifungals in vitro, including voriconazole. Antimycotic treatment options for mucormycosis are limited to posaconazole, isavuconazole, and amphotericin B [27]. Parenteral amphotericin B is the first-line recommended antifungal [18,24]. However antifungal susceptibility testing is highly proposed to adapt the treatment. But, the determination of susceptible categories is not possible for the agents of mucormycosis due to the lack of validated MIC breakpoints for any of the available antifungals [7].
The treatment duration is based on the severity and site of infection and the comorbidities of the patient. For pulmonary mucormycosis, the indication and timing of surgical management outside emergency care (hemoptysis) is still unclear although it may reduce mortality [7]. Surgical debridement should be as wide as possible to obtain healthy margins that allow the antifungal diffusion [22]. Immunologic and metabolomic profiling of the host, targeted immunotherapy and reversal of tissue hypoxia, may evolve in the future, leading to a better treatment of this devastating disease [22]. Mucormycosis is difficult to manage because of the clinico-radiological similarities with invasive aspergillosis. Early distinction from invasive aspergillosis is of utmost importance, as the treatment of aspergillosis (voriconazole) is not active on mucormycosis.
Conclusion
Mucormycosis is an aggressive opportunistic fungal infection, especially in hematological patients. The diagnosis and treatment of mucormycosis remain a challenge. Early distinction from invasive aspergillosis is mandatory and should be considered if the patient is presenting a pneumopathy resistant to the treatment. Despite new tools of molecular biology have been developed to obtain earlier diagnosis and start optimal treatment. Morbidity and mortality rates remains high and expanded studies should be carried to develop new therapies for this devastating fungal infection.
References
- Dimitrios F, Dimitrios PK. Mucormycoses. Infect Dis Clin North Am. 2016; 30: 143-146.
- George P , Anna S, Olivier L, Emmanuel R, Thomas JW, Dimitrios PK. Epidemiology and clinical manifestations of mucormycosis. Clin Infect Dis. 2012; 54: 23-34.
- Petrikkos G, Skiada A, Drogari-Apiranthitou M. Epidemiology of mucormycosis in Europe. Clin Microbiol Infect. 2014; 20: 67-73.
- Ramazan G , Uzeyir Y, Mehmet A, Kursat K, Fuat T, et al. A case of rhinoorbital mucormycosis in a leukemic patient with a literature review from Turkey. Mycopathologia. 2011; 172: 397-405.
- Chayakulkeeree M, Ghannoum MA, Perfect JR. Zygomycosis: The re-emerging fungal infection. European Journal of Clinical Microbiology Infectious Diseases. 2006; 25.
- . Brad S , John E, Ashraf I. Novel perspectives on mucormycosis: Pathophysiology, presentation, and management. Clin Microbiol Rev. 2005; 18: 556-569.
- Benoit P , Alexandre A , Olivier L , Fanny L. .Recent advances in the understanding and management of mucormycosis. F1000 Res. 2018; 7.
- Sheri KP , Tirdad TZ , Stephen AG , Michael GL. .An aggressive multidisciplinary approach reduces mortality in rhinocerebral mucormycosis. Surg Neurol Int. 2016; 7: 61.
- Anna S, Fanny L, Andreas HG, Livio P, Stephan Z, Raoul H et al. European Conference on Infections in Leukemia. Diagnosis and treatment of mucormycosis in patients with hematological malignancies: Guidelines from the 3rd European Conference on Infections in Leukemia (ECIL 3). Haematologica. 2013; 98: 492- 504.
- Russell EL, Dimitrios PK. Epidemiology and treatment of mucormycosis. Future Microbiol. 2013; 8: 1163-1175.
- Syeda NA , Rajani K , Guttikonda VR , Jayakiran M..Mucormycosis in a Diabetic Patient: A Case Report with an Insight into Its Pathophysiology. Contemp Clin Dent. 2017; 8: 662-666.
- Ayadi Kaddour ,E, Braham ,O, Ismail ,E, Saïji ,M, Bourguiba ,M, Zaïmi ,F, et al. Mucormycosepulmonaire. Revue de pneumologie Clinique. 2006; 26: 37.
- Latifa M , Chiraz H , Makram T , Siwar B , Hana S , Raja BS , et al. Successful treatment of rhino-facial mucormycosis in a diabetic patient. Med Mycol Case Rep. 2020; 27: 64-67.
- Bitar D, Van Cauteren D, Lanternier F. Increasing incidence of zygomycosis (mucormycosis), France, 1997–2006. Emerg Infect Dis. 2009; 15: 1395–1401.
- Jorge LH , Clifford JB. Mucormycosis. Treasure Island (FL): Stat Pearls Publishing. 2021: 26.
- Walther G, Wagner L, Kurzai O. Updates on the taxonomy of Mucorales with an emphasis on clinically important taxa. J Fungi (Basel). 2019; 5: 106.
- Jeong W, Keighley C, Wolfe R, Lee WL, Slavin MA, Kong DCM, et al. The epidemiology and clinical manifestations of mucormycosis: A systematic review and meta-analysis of case reports. Clin Microbiol Infect. 2019; 25: 26–34.
- Zhiming L, Lin Z. Diagnosis and treatment of pulmonary mucormycosis: A case report. Experimental and therapeutic medicine. 2017; 14: 3788-3791.
- Bo Da N , Tae Jung K, Kyung Soo L, Tae Sung K, Joungho H, et al. .Pulmonary mucormycosis: Serial morphologic changes on computed tomography correlate with clinical and pathologic findings. Eur Radiol. 2018; 28: 788-795.
- Feki W, Sellami S, Charfi S, Ketata W, Msaad S, et al. Successful Medical Treatment of Pulmonary Mucormycosis in Diabetic Patients. J Pulm Respir Med. 8: 444.
- Anna S, Ioannis P, Maria D. Epidemiology and Diagnosis of Mucormycosis: An Update J Fungi (Basel). 2020; 6: 265.
- Skiada A, Lass-Floerl C, Klimko N, Ibrahim A, Roilides E, Petrikkos G. Challenges in the diagnosis and treatment of mucormycosis. Med Mycol. 2018; 56: 93-101.
- Sanjeet SD, Dimitrios PK. Recent advances in the molecular diagnosis of Mucormycosis. Expert Review of Molecular Diagnostics. 2018; 18: 845-854.
- Alanio A, Garcia Hermoso D, Mercier Delarue S. Molecular identification of Mucor in human tissues: Contribution of PCR electrospray-ionization mass spectrometry. Clin Microbiol Infect. 2015; 21: 594.
- Rickerts V, Just-Nubling G, Konrad F. Diagnosis of invasive aspergillosis and mucormycosis in immunocompromised patients by semi-nested PCR assay of tissue samples. Eur J Clin Microbiol Infect Dis. 2006; 25: 8-13.
- Garrouch A, Tlili C, Zaatir N, Toulali L, Abdelghani A, Klabi N, et al. Résultats thérapeutiques de la mucormycose pulmonaire: A propos de deux observations. Revue des maladies respiratoires. 2009; 26.
- Jürgen Benjamin H , Martina F , Verena W , Donald B , Grit W , et al. First case of fatal Rhizomucor miehei endocarditis in an immuno compromised patient. Diagn Microbiol Infect Dis. 2020; 98.