Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Research Article - Open Access, Volume 3
Evaluation of IL-1β and TNF-α level in endometrial flush in patients with recurrent implantation failure
Radu Harșa1; Irena Pintea2,3*; Romeo Micu1; Mihai Surcel1; Florin Stamatian1
1 Human Assisted Reproduction Department of 1st Gynecology Clinic, “Iuliu Hatieganu” University of Medicine and Pharmacy ClujNapoca, Romania.
2 Allergy and Immunology Department, “Iuliu Hatieganu” University of Medicine and Pharmacy Cluj-Napoca, Romania.
3 Allergy Ambulatory, “Professor Doctor Octavian Fodor” Regional Institute of Gastroenterology and Hepatology, Cluj-Napoca, Romania.
*Corresponding Author: Irena Pintea
Regional Institute of Gastroenterology and Hepatology, 19-21 Croitorilor street, Cluj-Napoca, Romania,
400162.
Email: irennedelea@gmail.com
Received : Jan 21, 2022
Accepted : Feb 28, 2022
Published : Mar 07, 2022
Archived : www.jcimcr.org
Copyright : © Pintea I (2022).
Keywords: IL-1β; TNF-α; recurrent implantation failure; unexplained infertility; in vitro fertilization.
Citation: Harșa R, Pintea I, Micu R, Surcel M, Stamatian F. Evaluation of IL-1β and TNF-α level in endometrial flush in patients with recurrent implantation failure. J Clin Images Med Case Rep. 2022; 3(3): 1718.
Introduction
Infertility is defined as the inability to conceive within a year of regular unprotected intercourse affecting one in six couples. The most common causes of infertility are ovulatory dysfunction, male factor infertility, and tubal disease [1]. Unexplained Infertility (UI) and Recurrent Implantation Failure (RIF) are diagnoses based on failed pregnancy attempts with current infertility treatment options. UI is diagnosed when testing is inconclusive and RIF is diagnosed after three failed In Vitro Fertilization (IVF) cycles. UI is the absence of conception despite 12 months of unprotected intercourse, not explained by anovulation, poor sperm quality, tubal pathology or other known cause of infertility. RIF is defined by three failed IVF cycles in which one or two high-quality embryos are transferred in each cycle or by two failures in oocyte donor recipients after the transfer of good quality embryos [1]. UI is a common cause of infertility affecting 10-30% of infertile couples [2], while RIF is present in around 10% of in vitro fertilization (IVF) cycles [3].
The process of embryo implantation, which is vital for a successful pregnancy, starts in a receptive endometrium. Endometrial receptivity and embryo-endometrial epithelium interactions for implantation are critical determinants of fertility. Failure of regulation of local immune processes may cause pregnancy failure and infertility, particularly in UI.
Several studies investigated the putative impact of endometrial cytokine levels on the outcome of in vitro fertilization in patients with recurrent implantation failure. Cytokines are secreted during both the innate and the adaptive immune responses and they are key mediators and regulators of the complex interplay between the fetus and uterine mucosa, which pleads for their major influence on endometrial receptivity [4,5].
Varying levels of Interleukin-1 Beta (IL-1β) and Tumor Necrosis Factor Alpha (TNF-α) and of other cytokines may contribute to an increased endometrial receptivity. Since the uterine fluid, collected by either lavage or aspiration, which is less invasive than tissue biopsy is indicative of the implantation microenvironment [6], we have assessed and correlated the endometrial flush levels of these two cytokines with embryo implantation and successful pregnancy in females with repeated implantation failure.
Materials and methods
The proposed investigation is a prospective study using samples from patients treated in the Assisted Human Reproduction Department of the Gynecology Clinic I Cluj-Napoca between 2018 and 2021. All patients received informed consent in which they could accept or refuse the use of biological samples collected for research purposes. We used only samples from patients who agreed with assessing endometrial flush samples for this purpose. To carry out this study, we obtained the agreement of the University of Medicine and Pharmacy Cluj-Napoca Ethics Committee. We performed data analysis according to the established statistical methods.
We enrolled 96 female patients with ages 26 to 46 years with repeated implantation failure (at least 3 previous failed IVF cycles, at least 2 consecutive cycles in which a total of at least 4 embryos were transferred in the cleavage stage or at least 2 embryos in the blastocyst stage, all embryos being of good quality). All patients followed the IVF / ICSI protocol. The exclusion criteria were: patients with metabolic or endocrine disorders, atrophic endometrium (<7 cm), OHSS, patients with uterine or adnexal pathology (fibroids, polyps, hydrosalpinx, endometriosis, etc).
All patients followed a short antagonist stimulation protocol. The initial dose for ovarian stimulation was 150-300 IU rFSH (Gonal F). To induce the final oocyte maturation, we used 10,000 IU of urinary-hCG. After thirty-six hours we performed the oocytes retrieval. Between 1 and 3 good-quality embryos were transferred. We performed serum beta-hCG dosing or a urine pregnancy test on day 14 in all patients. We performed endovaginal ultrasound between weeks 4 and 6, to detect the embryo and fetal heart rate.
Sample collection
Before ovarian puncture, the vagina and the cervix were washed with normal saline solution. We injected 2 ml of saline solution into the uterine cavity with a catheter and the liquid was aspired and stored at -18 degrees C. For evaluation of IL-1β and TNF-α levels, we used standard ELISA kits (Invitrogen, USA).
Statistical analysis of the collected data was performed through SPSS Software.
Results
The mean age of the patients included in the study was 35 ± 5.6 years (26-46), and the body mass index ranged from 16.8 to 36.4 kg/m2 . The average age of the partners was 38 ± 6.5 years (24-50), and the number of sperm varied between 0.2-80 X 106/ml. These couples had a history of sterility of 4.4 ± 2.7 years. The average number of obtained oocytes was 8 (1-22), and the average number of embryos was 5 (1-9). Of the 96 patients enrolled, 34 (35.41%) obtained a biochemical pregnancy (beta-HCG or positive pregnancy test after 2 weeks). Twelve of the pregnancies did not have an embryo with cardiac activity on 6-week ultrasound nor resulted in a first-trimester abortion, so only 22 (22.91%) patients went on to have live births. The second group did not result in pregnancy after the IVF protocol.
There were no statistically significant differences between the two groups in terms of age, BMI, duration of infertility, AFC, number of transferred embryos, number of oocytes obtained, or number of embryos obtained. (Table 1).
Table 1: Characteristics of pregnant and non-pregnant group
Characteristic |
Beta-hCG positive |
Beta-hCG negative |
P Value |
Age (years) |
35.1 ± 5.4 |
35.6 ± 5.6 |
0.7 |
BMI |
24.2 ± 5.7 |
23.7 ± 5 |
0.7 |
Duration of |
4.4 ± 2.1 |
4.5 ± 2.2 |
0.8 |
AFC |
12 ± 4 |
11 ± 4.3 |
0.3 |
Number of transferred embryos |
1.8 ± 0.7 |
1.8 ± 0.6 |
0.6 |
Data are presented as mean ± Standard Deviation; Beta-hCG: Beta-human chorionic gonadotropin; BMI: Body mass index; AFC: Antral follicular count.
Regarding IL-1β, a significantly higher level of endometrial secretion was observed in patients with biochemical pregnancy compared to patients who did not obtain pregnancy (Table 2). However, if we compare patients with biochemical pregnancy with patients with completed pregnancy, there are no statistically significant differences in IL-1β levels (Table 3).
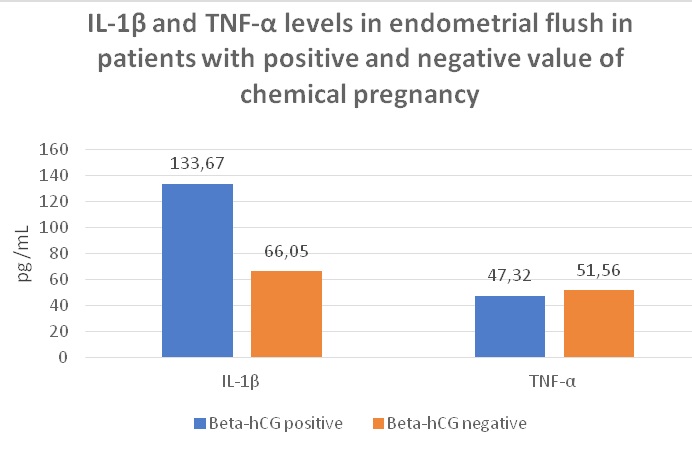
Table 2: IL-1β and TNF-α levels in endometrial flush of patients with a positive and negative chemical pregnancy
Characteristic |
Beta-hCG positive |
Beta-hCG negative |
P-Value |
TNF-α (pg / mL) |
47.3 ± 13.6 |
51.6 ± 18.5 |
0.3 |
IL-1β (pg / mL) |
133.7 ± 70.6 |
66.1 ± 55.8 |
<0.001 |
Data are presented as mean ± Standard Deviation; Beta-hCG: Beta-human chorionic gonadotropin; TNF-α: Tumor Necrosis Factor-alpha; IL-1β and Interleukin-1 beta.
Table 3: Comparison of IL-1β and TNF-α levels in endometrial flush of patients with positive chemical pregnancy and live birth pregnancy
Characteristic |
Beta-hCG positive |
Live birth pregnancy N = 22 |
P-Value |
TNF-α (pg / mL) |
47.3 ± 13.6 |
45.5 ± 18.9 |
0.7 |
IL-1β (pg / mL) |
133.7 ± 70.6 |
135.2 ± 70.3 |
0.9 |
Data are presented as mean ± Standard Deviation; Beta-hCG: Beta-human chorionic gonadotropin; TNF-α: Tumor Necrosis Factor-alpha; IL-1β and Interleukin-1 beta.
Although the group of patients who did not obtain pregnancy showed a higher level of TNF-α, there are no statistically significant differences between the analyzed groups (Chart 1).
Discussions
Embryo implantation occurs during a short period of time, the implantation window, in the mid-secretory phase of the menstrual cycle [7,8]. Current data plead to demonstrate that the endometrium is not a passive partner in the reproductive process, as it was initially regarded. Functionally, the endometrium is defined as a highly dynamic tissue encompassing a functional layer, which results in the implantation site of the embryo and is completely shed during menstruation, and a basal layer, which is crucial for the optimal reconstruction of the epithelium after the menstrual cycle [9-11].
The process of embryo implantation, which is vital for a successful pregnancy, starts in a receptive endometrium. Endometrial receptivity and embryo-endometrial epithelium interactions for implantation are critical determinants of fertility, and a wide array of biological factors, including cytokines and chemokines, prostaglandins, adhesion molecules, growth factors, and others, orchestrate successful implantation [4,12-15]. Several studies investigated the putative impact of endometrial cytokine levels on the outcome of in vitro fertilization in patients with recurrent implantation failure.
Cytokines are a heterogeneous family of more than 100 small molecules secreted during both the innate and the adaptive immune responses. They are crucial factors in regenerative and inflammatory–like processes such as the menstrual cycle in human endometrium and are also implicated in specific events like reproduction, ovulation and implantation [16]. Several cytokines are key mediators and regulators of the complex interplay between the fetus and uterine mucosa, which pleads for their major influence on endometrial receptivity [4]. Varying levels of Interleukin-1 Beta (IL-1β) and Tumor Necrosis Factor Alpha (TNF-α) may contribute to an increased endometrial receptivity. In the present study we have assessed and correlated the endometrial flush levels of these two cytokines with embryo implantation and successful pregnancy in females with repeated implantation failure.
IL-1β is a key mediator in the immunological and inflammatory responses, responsible for positively regulating the level of expression of β3 integrin, a cellular adhesion molecule involved in the successful implantation of the blastocyst [17]. IL-1β is produced by the stromal and glandular cells throughout the menstrual cycle with a peak at the luteal phase. A significant decrease, however, of the endometrial expression of IL-1β during the implantation window suggests the presence of specific regulatory mechanisms which, by the inhibition of its antagonist, supports its role in embryo implantation [18-20]. Moreover, further studies show an increased level of expression of IL-1β in women with successful implantation [21]. The dynamic changes of IL-1β with elevated expression during luteal phase and successful embryo implantation and a decreased expression during the implantation window are arguments in favor of its influence on embryo-endometrial interaction.
Our data also point out the effector role of IL-1β through the success of embryo implantation process. A significantly higher level of IL-1β in the endometrial secretion was observed in patients with biochemical pregnancy compared to patients who did not obtain pregnancy. However, when compared patients with biochemical pregnancy with patients with completed pregnancy, there are no statistically significant differences in IL-1β levels.
Regarding TNF-α, although the group of patients who did not obtain pregnancy showed a higher level in the endometrial secretion, there were no statistically significant differences between the analyzed groups.
Literature brings conflicting data regarding the levels of TNF-α. Some authors show that TNF-α levels show similar dynamics to those of IL-1β, with a positive correlation of high expression in women with successful implantation [21]. However, according to other authors, TNF-α is significantly increased in women with a history of recurrent abortion and infertility [22,23]. Other studies state the existence of a positive correlation between successful pregnancy and higher levels of TNF-α and lower levels of IL-1β in endometrial secretions [24]. Similar studies concluded that lower levels of TNF-α in endometrial secretions results in the improvement of endometrial reception, while not finding any significant difference between IL-1β of the two groups in terms of increasing chance of performing successful implantation [25].
A recent study on the association of IL-1β and TNF-α levels in endometrial secretion and success of embryo transfer in IVF/ ICSI cycles did not find any significant statistical relationship between higher levels of IL-1β in endometrial secretion and successful implantation nor any statistical significant difference of TNF-α level of expression between the two groups with successful and unsuccessful implantation [26].
Another aspect in reproductive medicine is immunologic tolerance, mandatory for the protection against precocious rejection of the blastocyst [27]. The embryo constitutes a potential target for the maternal immune system attack, as the blastocyst is a semi-allograft with 50% of its genome being paternally derived. It is estimated that in over 20% of the couples experiencing UI, the implantation failure is attributed to immune system alterations [28,29]. Cytokine homeostasis in the female reproductive tract is crucial for the induction of an immunologic tolerance [30] and it requires the involvement of numerous cellular and soluble factors. Th1/Th2 lymphocytes equilibrium in the endometrium is thus of interest in reproductive medicine. Th1 lymphocytes produce mainly pro-inflammatory cytokines, like IL-1β and TNF-α, while Th2 lymphocytes produce anti-inflammatory cytokines. Th1cytokines, which promote the immune system rejection, can be harmful for the pregnancy, while Th2 can promote the tolerance to the semi-allogeneic fetus, allowing the pregnancy to take place [31,32]. Assessment of cytokines that are representative for Th1/Th2 balance in the endometrial fluid may also be indicative of the immunological tolerance of the blastocyst. Another argument in favor of the role of TNF-α and cytokine disequilibrium in infertile women is brought on by the potential use of TNF-α inhibitors to counteract the increased production of Th1 cytokines associated with early reproduction failure [33].
Conclusions
UI affects a significant proportion of infertile couples and it poses a notable burden on the quality of life of affected individuals. The process of embryo implantation, which is vital for a successful pregnancy, starts in a receptive endometrium. Endometrial receptivity and embryo-endometrial epithelium interactions for implantation are critical determinants of fertility, and a better understanding of immunological factors that promote successful pregnancy in UI and RIF women might point to therapeutic targets and prognostic factors of treatment outcome. Our study identified a positive correlation of Il-1β and a negative correlation of TNF-α in the endometrial secretion and successful implantation, which suggests that IL-1β might be a favorable prognostic factor, while TNF-α could serve as target in the treatment of UI and RIF patients.
References
- Santamaria X, Simón C. Endometrial Factor in Unexplained Infertility and Recurrent Implantation Failure. Semin Reprod Med. 2021; 39: 227-232.
- Gunn DD, Bates GW. Evidence-based approach to unexplained infertility: A systematic review. Fertil Steril. 2016; 105: 1566- 1574.
- Bellver J, Simón C. Implantation failure of endometrial origin: what is new? Curr Opin Obstet Gynecol. 2018; 30: 229-236.
- Governini L, Luongo FP, Haxhiu A, Piomboni P, Luddi A, et al. Main actors behind the endometrial receptivity and successful implantation. Tissue Cell. 2021; 73: 101656.
- Guzeloglu-Kayisli O, Kayisli UA, Taylor HS. The role of growth factors and cytokines during implantation: Endocrine and paracrine interactions. Semin Reprod Med. 2009; 27: 62-79.
- Salamonsen LA, Edgell T, Rombauts LJ, Stephens AN, Robertson DM, et al. Proteomics of the human endometrium and uterine fluid: A pathway to biomarker discovery. Fertil Steril. 2013; 99: 1086-1092.
- Bergh C, Hillensjo T, Nilsson L. Sonographic evaluation of the endometrium in invitro fertilization IVF cycles. A way to predict pregnancy? Acta Obstet. Gynecol. Scand. 1992; 71: 624–628. https://doi.org/10.3109/00016349209006231.
- Wang X, Wu SP, De Mayo FJ. Hormone dependent uterine epithelial-stromal communication for pregnancy support. Placenta. 2017; 60: S20–S26. https://doi. org/10.1016/j.placenta.2017.07.003.
- Yamaguchi M, Yoshihara K, Suda K, Nakaoka H, Yachida N, et al. Three-dimensional understanding of the morphological complexity of the human uterine endometrium. iScience. 2021; 24: 102258. https://doi.org/10.1016/j.isci.2021.102258.
- Yoshimasa Y, Maruyama T. Bioengineering of the uterus. Reprod. Sci. 2021; 28: 1596–1611. https://doi.org/10.1007/s43032-021- 00503-8.
- Micu R, Petrut B, Zlatescu-Marton C, Traila A, Harsa R, et al. Current strategies and future perspectives in fertility preservation for cancer patients. J BUON. 2017; 22: 844-852.
- Fitzgerald HC, Salamonsen LA, Rombauts LJR, Vollenhoven BJ, Edgell TA, et al. The proliferative phase underpins endometrial development: Altered cytokine profiles in uterine lavage fluid of women with idiopathic infertility. Cytokine. 2016; 88: 12–19. https://doi.org/10.1016/j.cyto.2016.08.001.
- Harsa R, Nedelea I, Surcel M, Stamatian F, Micu R, et al. Natural Killer cells in embryo-implantation. Rom Biotechnol Lett. 2019; 24: 789-797.
- Zhao Y, Garcia J, Kolp L, Cheadle C, Rodriguez A, et al. The impact of luteal phase support on gene expression of extracellular matrix protein andadhesion molecules in the human endometrium during the window of implantation following controlled ovarian stimulation with a Gn RH antagonist protocol. Fertil. Steril. 2010; 94: 2264–2271. https://doi.org/10.1016/j.fertnstert.2010.01.068.
- Truta Z, Garlovanu M, Lerintiu S, Micu R. A new method for human semen glucose concentration evaluation. Rom Biotechnol Lett. 2010; 15: 5764-5772.
- Guzeloglu Kayisli O, Kayisli UA, Taylor HS. The role of growth factors and cytokines during implantation: Endocrine and paracrine interactions. Semin. Reprod. Med. 2009; 27: 62–79. https://doi. org/10.1055/s-0028-1108011.
- Simon C. Embryonic regulation of integrins 3, 4, and 1 in human endometrial epithelial cells in vitro. J. Clin. Endocrinol. Metab. 1997; 82: 2607–2616. https://doi.org/ 10.1210/jc.82.8.2607.
- Boucher A, Kharfi A, Al-Akoum M, Bossù P, Akoum A, et al. Cycledependent expression of Interleukin-1 receptor type II in the human Endometrium1. Biol. Reprod. 2001; 65: 890–898. https:// doi.org/10.1095/biolreprod65.3.890.
- Zhou L, Li R, Wang R, Huang HX, Zhong K, et al. Local injury to the endometrium in controlled ovarian hyperstimulation cycles improves implantation rates. Fertil Steril. 2008; 89: 1166-1176.
- Bourdiec A, Akoum A. Embryo implantation: Role of interleukin 1 family members. Med Sci (Paris). 2014; 30: 644-650.
- Sequeira K, Espejel-Núñez A, Vega-Hernández E, MolinaHernández A, Grether-González P, et al. An increase in IL-1β concentrations in embryo culture-conditioned media obtained by in vitro fertilization on day 3 is related to successful implantation. J Assist Reprod Genet. 2015; 32: 1623-1627.
- Loetscher P, Seitz M, Clark-Lewis I, Baggiolini M, Moser B, et al. Monocyte chemotactic proteins MCP-1, MCP-2, and MCP-3 are major attractants for human CD4+ and CD8+ T lymphocytes. FASEB J. 1994; 8: 1055-1060.
- Reid JG, Simpson NA, Walker RG, Economidou O, Shillito J, et al. The carriage of pro-inflammatory cytokine gene polymorphisms in recurrent pregnancy loss. Am J Reprod Immunol. 2001; 45: 35-40.
- Boomsma CM, Kavelaars A, Eijkemans MJ, Lentjes EG, Fauser BC, et al. Endometrial secretion analysis identifies a cytokine profile predictive of pregnancy in IVF. Hum Reprod. 2009; 24: 1427- 1435.
- Rahiminejad ME, Moaddab A, Ebrahimi M, Rabiee S, Zamani A, et al. The relationship between some endometrial secretion cytokines and in vitro fertilization. Iran J Reprod Med. 2015; 13: 557-562.
- Khadem N, Mansoori M, Attaran M, Attaranzadeh A, Zohdi E, et al. Association of IL-1 and TNF-α Levels in Endometrial Secretion and Success of Embryo Transfer in IVF/ICSI Cycles. Int J Fertil Steril. 2019; 13: 236-239.
- Piccinni MP. T cell tolerance towards the fetal allograft. J. Reprod. Immunol. 2010; 85: 71–75. https://doi.org/10.1016/j. jri.2010.01.006.
- Ali SB, Jeelall Y, Pennell CE, Hart R, McLean-Tooke A, Lucas M, et al. The role of immunological testing and intervention in reproductive medicine: A fertile collaboration? Am. J. Reprod. Immunol. 2018; 79 https://doi.org/10.1111/aji.12784.
- Murata H, Tanaka S, Okada H. Immune tolerance of the human decidua. J. Clin. Med. 2021; 10 https://doi.org/10.3390/ jcm10020351.
- Piccinni MP, Lombardelli L, Logiodice F, Kullolli O, Parronchi P, et al. How pregnancy can affect autoimmune diseases progression? Clin. Mol. Allergy. 2016; 14: 11. https://doi.org/10.1186/ s12948-016-0048-x.
- Zabrodskii PF, Germanchuk VG, Mandych VG, Kadushkin AM. Role of Th1 and Th2 lymphocytes and cytokines produced by these cells in suppression of immune reactions during subacute poisoning with anticholinesterase toxicants. Bull. Exp. Biol. Med. 2007; 144: 57–59. https://doi.org/10.1007/s10517-007-0253-1.
- Piccinni MP, Giudizi MG, Biagiotti R, Beloni L, Giannarini L, et al. Progesterone favors the development of human T helper cells producing Th2-type cytokines and promotes both IL-4 production and membrane CD30 expression in established Th1 cell clones. J. Immunol. 1995; 155: 128–133.
- Clark DA. Anti-TNF alpha therapy in immune-mediated subfertility: State of the art. J Reprod Immunol. 2010; 85: 15-24.