Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 5
A fecaluria revealing a Crohn’s disease in a patient treated for vesical carcinoma: A case report
Ossama Jalal*; Omar Jendouzi
Military Hospital Oued Edd Ahab, Agadir, Morocco.
*Corresponding Author : Ossama Jalal
Military Hospital Oued Edd Ahab, Agadir, Morocco.
Email: ossama.jalal@gmail.com
Received : Nov 21, 2024
Accepted : Dec 05, 2024
Published : Dec 12, 2024
Archived : www.jcimcr.org
Copyright : © Jalal O (2024).
Abstract
We report a case of an uncommon complication of Crohn’s disease characterized by an enterovesical fistula responsible for fecaluria. our patient had a history of bladder tumor, which was initially considered the cause of his fecaluria. However, diagnostic imaging, specifically Computed Tomography (CT) scan and Magnetic Resonance Imaging (MRI), were used to confirm the presence of the enterovesical fistula, as these modalities are the most specific and sensitive for diagnosing this condition.
The management of vesicointestinal fistulas in the context of Crohn’s disease requires both medical and surgical interventions. Surgical treatment involves the resection of the diseased bowel segment, excision of the fistula, and reanastomosis of the bowel.
Citation: Jalal O, Jendouzi O. A fecaluria revealing a Crohn’s disease in a patient treated for vesical carcinoma: A case report. J Clin Images Med Case Rep. 2024; 5(12): 3385.
Introduction
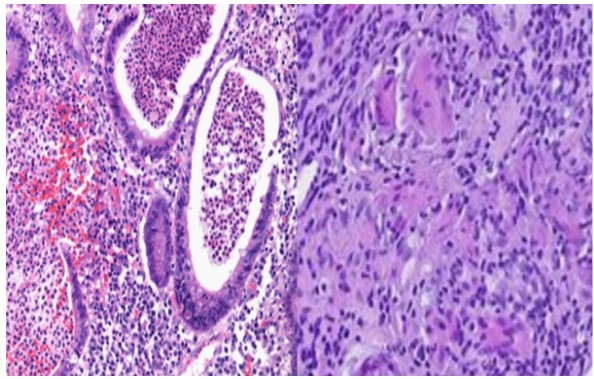
Crohn’s disease is a chronic inflammatory condition affecting the gastrointestinal tract, characterized by the development of intestinal ulcerations often complicated by the formation of fistulae, attributed to an overactive immune response. These complications may affect the genitourinary system [1].
An enterovesical fistula represents an anatomical abnormality, creating a passage that connects the bladder to the bowel [2].
Although the incidence of enterovesical fistula is rare, (ranging from 2% to 5% in patients with Crohn’s disease (CD) [3]), the impact on patients’ health is substantial.
This article presents a case study of a young patient with Crohn’s disease revealed by fecaluria.
Patient and observation
Patient information: The patient is a 43-year-old man with a medical history of cigarette smoking and a previous diagnosis of pTa low-grade urothelial tumor. This tumor was successfully treated with resection and Bacillus Calmette-Guérin (BCG) therapy, showing no recurrence or progression over a 5-year following. The patient recently presented a moderate gross hematuria with clots associated somtimes to fecaluria and diarrhea, weight loss, dysuria, pollakuria, and urgency, despite the absence of other digestive symptoms. Physical examination revealed a remarkable weight loss with low BMI of 19 kg/m², cloudy urine with visible fecal material. Blood tests indicated a normocytic-normochromic anemia and elevated Calprotectin (>1500). Urinary examination demonstrated an increased number of leukocytes and red cells, along with the presence of fecal material. A positive urinary culture for Escherichia coli was reported. Ultrasound findings showed thickening of the bladder wall, particularly in the superior region, with no evidence of bladder tumor recurrence. Abdominal and pelvic CT scans revealed diffuse wall thickening in the sigmoid and bladder, accompanied by the presence of gas in the bladder.
Discussion
Enterovesical fistulae represent an uncommon complication arising from both benign and malignant processes [4]. Crohn disease stands out as a frequent cause of uro-digestif fistula, predominantly affecting the ileovesical (64%), colovesical (21%), and rectovesical (8%) regions [4].
Among crohn’s-related vesicointestinal fistula the dome of the bladder is the most frequently affected site, which is the closest portion of the bladder to the terminal ileum (most commonly affected bowel segment) with male predominance attributed to the absence of uterine interposition [1-5].
The most common manifestation of this fistula is irritative voiding symptoms and recurrent cystitis despite appropriate antibiotic treatment (68%). Other prevalent symptoms include pneumaturia (64%), urinary tract infection (32%), fecaluria (28%) [6].
Hematuria has been reported in several cases [7]; however, it can be mistaken for tumoral hematuria, particularly when associated with tumoral risk factors or observed thickening in radiologic exploration. As well in the present described case where patient have a history of bladder tumors, the real cause of hematuria may be obscured. However, however presence of pneumaturia is considered a pathognomonic sign of fistula [8], in absence of infection or recent instrumentation [1].
CT scanning and MR imaging are recognized as the most specific and sensitive non-invasive tools for imaging vesicointestinal fistula [2]. CT scanning demonstrates a positive rate ranging from 55% to 66.3%, while MR imaging gives an accuracy rate of 77.2% [3].
These imaging modalities may reveal various characteristic features such as: bladder wall thickening adjacent to a loop of thickening colon, presence of colonic diverticula, and the critical finding of intravesical air, which suggest the presence of fistula [5].
In addition, these imaging may show signs of the causal pathology (Crohn’s disease, Diverticulitis, tumoral), as well as complications, which can guide management.
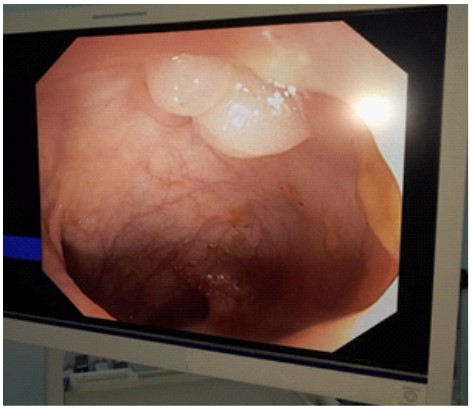
Cystoscopy can also be a valuable tool in identifying the fistula, although it can fail in >50% of patients and shows only intravesical oedema [9].
Cystoscopy detect associated signs such as erythema, edema, and congestion in the surrounding area. However, it often challenging to identify the fistula orifice and even visualize the lumen of the fistula endoscopically, particularly when the tract is very small [9,10].
In our case the only finding was diffused inflammation, which lacks specificity and may hide the identification of a possible fistula orifice, also the presence of fecal material caused a bad vision.
Recently, Intracavitary Contrast-Enhanced Ultrasound (ICCEUS) has emerged as a promising technique for detecting entero-vesical fistulas. This approach involves the local injection of a contrast agent (e.g., indocyanine green), administered orally or intrarectally, then detected in urine [11]. This method may be beneficial especially when standard methods are insufficient.
The management of vesicointestinal fistula in Crohn’s disease, involves both medical and surgical approaches. Medical treatment has been reported to achieve a long-term remission in up to 35% of cases, However, it’s important to note that rates of morbidity, including poor physical status, progression of malignant disease, and septic complications, tend to increase after medical therapy compared to surgical management [12].
Therefore, medical management may be a good option for those who are not fit for surgery due to a poor condition, intolerance to general anesthesia, or terminal disease.
The use of antibiotics helps improving the quality of life in patients with fistulizing Crohn’s disease, long term treatment especially based on 5-ASA compounds such as mesalazine, azathioprine, and systemic corticosteroids; and anti-TNF therapy such as infliximab and adalimumab [13].
The appropriate surgical management of Crohn’s fistulae is the principle of resection of the primary disease segment of the bowl with extirpation of the fistula, and reanastomose the offending bowel segment [14,15].
The path of the fistula in the bladder is usually located on the dome, facilitating debridement and closure without danger to the trigone [14]. After repair, the bladder is drained for many days.
Recurrent infections can weaken and thicken the vesical and intestinal walls, and that may increase the operative time and complications [12].
Conclusion
This case highlights the importance of considering Crohn’s disease as a potential cause of enterovesical fistula in patients presenting with fecaluria.
Colonoscopy and cystoscopy are the best tool for a positive diagnosis.
The management of vesicointestinal fistula, involves both medical and surgical approaches.
Surgery is required in most cases, it consist on suturing the wall of the bladder and resection of the fistuled segment of the bowel.
References
- Manganiotis AN, Banner MP, Malkowicz SB. Urologic Complications of Crohn’s Disease. Surgical Clinics of North America. 2001; 81(1): 197-215.
- Widia F, Firman M, Irdam GA, Syaiful RA. A six years’ experience with 41 cases of enterovesical fistula in a Tertiary National Hospital in Indonesia: A retrospective study. Annals of Medicine and Surgery. 2022; 73: 103102.
- Su YR, Shih IL, Tai HC, Wei SC, Lin BR, et al. Surgical Management in Enterovesical Fistula in Crohn Disease at a Single Medical Center. International Surgery. 2014; 99(2): 120-5.
- Saint-Marc O, Frileux P, Vaillant JC, Chevallier JM, Texeira A, et al. [Enterovesical fistulas in Crohn disease: diagnosis and treatment]. 1995; 49(5): 390-5.
- Karashmalakov A, Georgiev Y, Zafirov G, Kasabov S, et al. Diagnosis and treatment of enterovesical fistulas. Scripta Scientifica Medica. 2017; 49(3): 53.
- Simon P, Turin N, Comperat E, Benhamou Y, Bitker MO, et al. Une fistule rectovésicale révélatrice d’une maladie de Crohn. Progrès en Urologie. 2008; 18(3): 193-5.
- Then JK, Cohen GS. Colovesical Fistula: An Uncommon Cause of Hematuria and Rectal Bleeding. Giouleme OI, éditeur. Case Reports in Gastrointestinal Medicine. 2022; 2022: 1-3.
- Najjar SF, Jamal MK, Savas JF, Miller TA. The spectrum of colovesical fistula and diagnostic paradigm. The American Journal of Surgery. 2004; 188(5): 617-21.
- Li S, Chen Z, Zhang Q, Huang C, Wang Z, et al. Four cases of enterovesical fistula and the importance of CT in the diagnosis. BJR|case reports. 2017; 3(1): 20150124.
- Holroyd DJ, Banerjee S, Beavan M, Prentice R, Vijay V, et al. Colovaginal and colovesical fistulae: the diagnostic paradigm. Tech Coloproctol. 2012; 16(2): 119-26.
- Intracavitary Contrast-enhanced Ultrasonography to Detect Enterovesical Fistula in Crohn’s Disease.pdf.
- Hsu MW, Chen WC, Wei TN, Huang CP. Management of Enterovesical Fistula in a Patient with Crohn’s Disease: A Case Report and Literature Review. Diagnostics. 2023; 13(9): 1527.
- Kaimakliotis P, Simillis C, Harbord M, Kontovounisios C, Rasheed S, et al. A Systematic Review Assessing Medical Treatment for Rectovaginal and Enterovesical Fistulae in Crohn’s Disease. Journal of Clinical Gastroenterology. 2016; 50(9): 714-21.
- Michelassi F, Marogna P, Incidence, Diagnosis, Treatment of Enteric and Colorectal Fistulae in Patients with Crohn’s Disease.