Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
Third trimester ovarian pregnancy: A diagnostic dilemma
Glaiza S de Guzman, MD*; Alexis M Martinez, MD; Joselito A Santiago, MD
Department of Obstetrics and Gynecology, Philippine General Hospital, University of the Philippines, Philippines.
*Corresponding Author : Glaiza S. de Guzman
Department of Obstetrics and Gynecology, University
of the Philippines, Philippine General Hospital, Taft
Avenue, Manila, Philippines.
Email: gsdeguzman1@gmail.com
Received : Jan 28, 2021
Accepted : Feb 19, 2021
Published : Feb 22, 2021
Archived : www.jcimcr.org
Copyright : © De Guzman GS (2021).
Abstract
Ovarian pregnancy is a type of ectopic pregnancy where the fertilized ovum is implanted in the ovary. It is a rare entity and preoperative diagnosis remains problematic due to its nonspecific clinical presentation and sonographic findings. Here, we present a case of an advanced ovarian pregnancy at 28 weeks’ age of gestation initially managed as a case of suspected abdominal pregnancy. Preoperative aortogram and embolization were done to minimize intraoperative blood loss. Upon exploration of the abdomen, the products of conception were contained within an intact right ovary. The patient underwent right salpingo-oophorectomy. We obtained a stillborn baby girl weighing 1410 grams with no gross deformities. Histopathology confirmed the diagnosis of an ovarian pregnancy. This case highlights the difficulties in diagnosing ovarian pregnancy despite advances in imaging and the use of preoperative embolization to minimize intraoperative blood loss and morbidity.
Keywords: Ectopic pregnancy, Ovarian pregnancy, Third trimester.
Citation: De Guzman GS, Martinez AM, Santiago JA. Third trimester ovarian pregnancy: A diagnostic dilemma. J Clin Images Med Case Rep. 2021; 2(1): 1015.
Introduction
Ovarian pregnancy is a rare variant of ectopic pregnancy, accounting for 0.5 to 3% of all extrauterine pregnancies [1]. Even with the advent of accessible and reliable diagnostic methods, accurate assessment is often difficult. Patients typically present with nonspecific symptoms including abdominal pain and vaginal bleeding. Devastating sequelae include hemodynamic compromise from rupture and hemorrhage. Early and accurate diagnosis with imaging modalities is vital due to the high maternal and neonatal mortality rates. However, the diagnosis is more often made intraoperatively [1,2].
Case Report
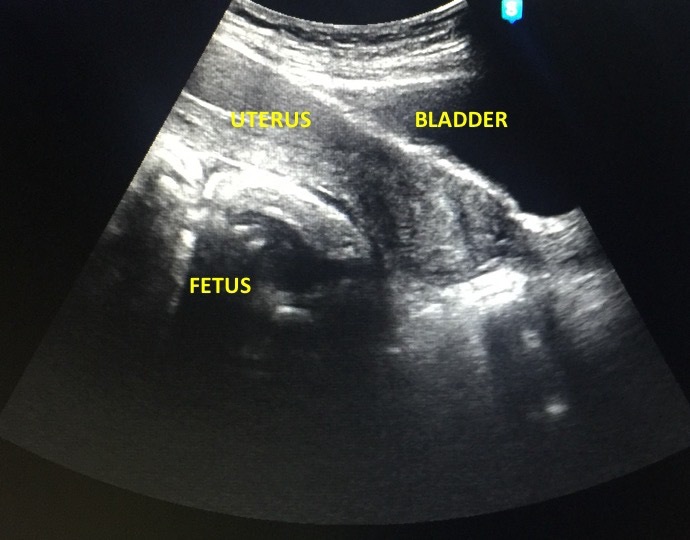
A 37-year-old G3P2 (2002) consulted at the emergency room of a tertiary training hospital with findings of intrauterine fetal demise on sonography. She has no previous surgeries, history of sexually transmitted infections, contraceptive use, or use of assisted reproductive technology. The fetus was palpated to be in breech presentation with an estimated fetal weight of 1200 to 1400 grams. On internal examination, her cervix was closed, uneffaced, posterior, and firm. Transvaginal ultrasound showed a single fetus in breech presentation with no cardiac and somatic activities at the cul-de-sac, posterior to a normal empty uterus (Figure 1). There was overlapping of cranial sutures and exaggerated spinal curvature. Sonographic impression was an abdominal pregnancy, single fetal demise at 28 1/7 weeks age of gestation by femoral length. The sonographic estimated fetal weight was 1044 grams by Hadlock.
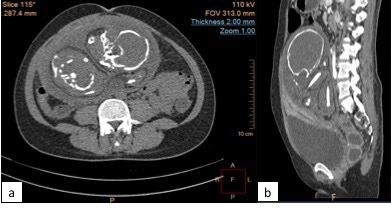
An abdominopelvic computed tomography (CT) scan showed a large, globular abdominal mass measuring 16.7 x 13.6 x 13.9 cm, likely representing a gestational sac with internal fetal structures (Figure 2). It was intimately related to the posterior aspect of the uterine isthmus. A heterogeneously enhancing curvilinear focus, likely representing the placenta is noted in its right superoanterior aspect. Feeding vessels were seen arising from a branch of the right internal iliac artery.
Preoperative embolization of the feeding vessels was done under total intravenous anesthesia. An abdominal aortogram mapped the feeding vessels of the placenta. Angiograms showed its arterial supply from tiny and tortuous branches of a parasitic artery arising from the right internal iliac artery. No other arterial supply from the branches of the abdominal aorta was noted. Using Progreat microcatheter, polyvinyl alcohol particles were injected into the feeding artery until complete cessation of flow was achieved.
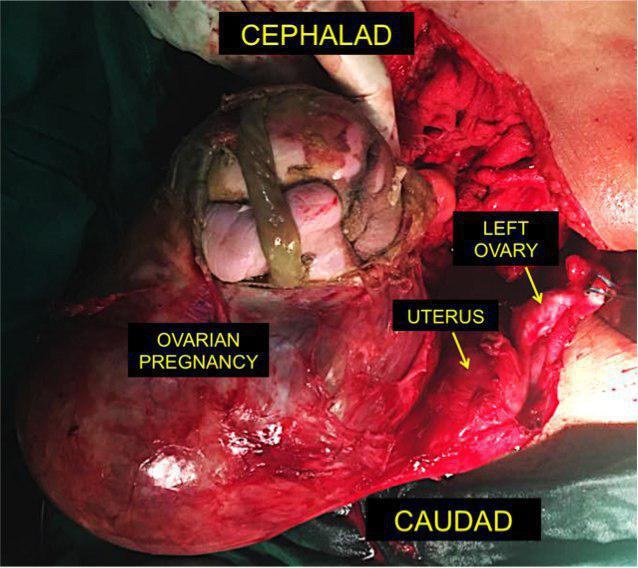
Exploratory laparotomy was done the following day. Intraoperatively, there was no hemoperitoneum. No normal right ovary was visualized.Occupying its place was an irregular cystic mass with intact capsule measuring 23.0 x 16.5 x14.5 cm with a demised fetus inside (Figure 3). There were dense adhesions to the cul-de-sac and right pelvic sidewall. Inadvertent rupture of the capsule was incurred during adhesiolysis. From the point of rupture, the fetal parts were visualized. Cut section of the cystic mass revealed a meconium-stained stillborn baby girl weighing 1410 grams (Figure 4). The left adnexa and the uterus were grossly normal.
The patient tolerated the procedure well with minimal blood loss. She had an unremarkable postoperative course and was discharged well on the second postoperative day. Histopathology result is consistent with an ovarian pregnancy at the right ovary.
Discussion
The ovaries are rare sites for ectopic implantation. Ovarian pregnancy frequently poses diagnostic dilemma for obstetricians due to its varied and nonspecific clinical presentation.The various hypotheses postulated to explain implantation anomalies causing ovarian pregnancy include ovum liberation delay, tunica albuginea thickening, and tubal dysfunction [4]. These hypotheses are due to an increased risk of ovarian pregnancy in patients with pelvic inflammatory disease. The inflammation causes thickening of the tunica albuginea which will eventually delay the liberation of ovum. Tubal dysfunction likewise increases the risk of ovarian pregnancy. The use of an intrauterine device was disproportionately associated with ovarian pregnancy [2]. Other risk factors reported are endometriosis, sexually transmitted diseases, ovulation induction agents, tubal sterilization and a history of abdominal surgery [1]. Despite not having the documented risk factors, the patient still developed ovarian pregnancy.
Common complaints include abdominal pain and vaginal bleeding, similar to tubal pregnancies. The mean age of gestation of ovarian pregnancies reported in literature is 45 days [5]. Rupture usually occurs before the end of the first trimester and may often present with hemodynamic instability. Most cases (91.0%) present with rupture during the first trimester, with 5.3% and 3.7% occurring during the second third trimesters respectively [6]. In our case, the ovarian pregnancy continued up to the third trimester without ovarian rupture.
Diagnosis is difficult since it mimics other forms of ectopic pregnancies as in our case. In earlier age of gestation, sonologic findings may mimic those of tubal pregnancies, ruptured corpus luteum, or adnexal masses in the absence of a yolk sac or fetal heart motion [1]. In a case series by Comstock et al., [7] an ovarian pregnancy is seen sonologically as a wide echogenic ring with an internal echolucent area compared to a thin tubal ring of tubal pregnancies or a corpus luteum cyst [7]. The use of 3D ultrasound has been reported to improve early detection. However, when presented with an advanced pregnancy, imaging studies may at times be difficult to interpret. In our patient, the first ultrasound showed an intrauterine pregnancy. The diagnosis of an ectopic pregnancy may have been missed if focus was only on biometry of the fetus. Sonographic diagnostic accuracy is operator-dependent and careful examination of pregnancy locations must be undertaken to avoid catastrophic events such as rupture, hemorrhage, and cardiovascular compromise [3,4].
The classic management option for ovarian pregnancies is surgical in the forms of wedge resection, cystectomy, or oophorectomy either through laparoscopy or laparotomy [4]. Medical management has also been described in literature for cases of unruptured ovarian pregnancies [2,4]. Etoposide and methotrexate have been used for persistence of trophoblastic tissues [8]. Decision making becomes more difficult when the diagnosis is made at an advanced age of gestation. As pregnancy progresses, vascular supply through feeding vessels to the ectopic gestation become abundant. This may necessitate devascularization techniques or preoperative embolization as in this case.
Locating the sites of ectopic pregnancies remains a diagnostic challenge. Despite benefits of imaging procedures, definitive diagnosis can only be made during surgery [1,6]. Careful preoperative planning should be undertaken. In our case, embolization was done preoperatively to map the vascular supply of the ectopic gestation and to minimize risk of bleeding from its feeding vessels. Minimal blood loss was incurred during the operation.
Conclusion
While recent advances in biochemical testing and sonology has allowed for the earlier detection and diagnosis of ectopic pregnancies, diagnosis of ovarian pregnancy remains to be problematic. Diagnostic imaging accuracy is imperative in the recognition of this entity. High index of suspicion, early recognition and prompt intervention are needed to avoid both maternal and fetal compromise in cases of viable gestation.
References
- Melcer Y, Smorgick N, Vaknin Z. Primary ovarian pregnancy: 43 years experience in a single institute and still a medical challenge. 2015. The Israel Medical Association Journal 2015; 17: 687-690.
- Mann B, Meranza DR, Leff B. Ovarian pregnancy, primary or secondary? American Journal of Obstetrics & Gynecology 1941; 41(20): 322-326.
- Tehrani HG, Hamoush Z, Ghasemi M, Hashemi L. Ovarian pregnancy: A rare case. Iran J Reprod Med. 2014; 12(4): 281-284.
- Bangal VB, Madhumita G, Shashant SH. Primary ovarian pregnancy: a rare entity. Journal of Dental and Medical Sciences. 2016; 15(9): 111-113.
- Das S, Kalyani R, Lakshmi V, Harendra Kumar ML. Ovarian pregnancy. Indian J Pathol Microbiol. 2008; 51: 37-8.
- Comstock C, Huston K, Lee W. The ultrasonographic appearance of ovarian ectopic pregnancies. Obstet Gynecol. 2005; 105: 42-5.
- Juan YC, Wang PH, Chen CH, Ma PC, Liu WM. Successful treatment of ovarian pregnancy with laparoscopy-assisted local injection of etoposide. Fertility and Sterility. 2008; 90(4): 1200-e2.