Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
Lingual swelling: A clinical conundrum
Rukma Bhandary; S Poojitha*
Department of ENT, AJIMS, Mangalore, India
*Corresponding Author : S Poojitha
Department of ENT, AJIMS, Mangalore, India
Email: s.pooj97@gmail.com
Received : Feb 02, 2021
Accepted : Feb 26, 2021
Published : Mar 03, 2021
Archived : www.jcimcr.org
Copyright : © Poojitha S (2021).
Abstract
Swelling of the tongue usually pose a clinical dilemma, especially when presenting at an early age. Growths from all of these heterogeneous components may occur resulting in a wide variation in clinical features and behaviour, ranging from self-limiting to aggressive lesions. Here we present a case of a 9 year old female child, with complaints of swelling over the tongue and floor of mouth. She previously had a similar lesion at the age of 1 year, which was diagnosed to be a hamartoma. The aim of this study is to discuss how to proceed regarding the further management.
Keywords: Lingual swelling, Hamartoma, Lymphangioma, Paediatrics
Citation: Bhandary R, Poojitha S. Lingual swelling: A clinical conundrum. J Clin Images Med Case Rep. 2021; 2(2): 1019.
Introduction
Tongue controls critical function such as speech, taste sensation, swallowing, and cleansing of the oral cavity. If lingual deformation or pathology occurs, these functions become impaired [1]. Tongue lesions may be classified according to their location, nature, composition, depth, and behaviour. They are commonly classified into developmental, reactive, benign, or malignant lesions. Recognition and diagnosis of these lesions require adequate knowledge about the basic anatomy of the tongue, proper history and comprehensive examination. As a rule, most of the tongue lesions resolve fast as regards the high blood supply unless they have to be biopsied to exclude the malignancies [2,3].
Case presentation
A 9 year old female child presented to the otolaryngology outpatient department with c/o swelling over the floor of the mouth since the age of 1 year- insidious in onset, no increase or decrease in size over the years. She also c/o swelling over the dorsum of tongue - since 1 month, insidious in onset, gradually progressive in size, bleeds on eating food. No complaints of difficulty in swallowing, respiratory discomfort, or pain. Parents give a past history of excision of a similar lesion over the dorsum of tongue- at 1 year of age- histopathological examination was suggestive of Hamartoma.
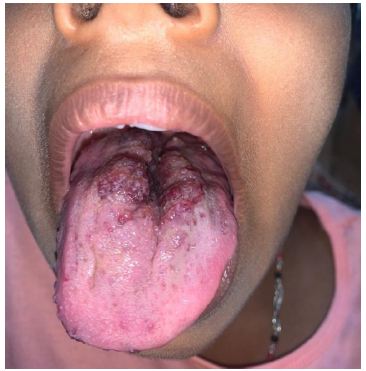
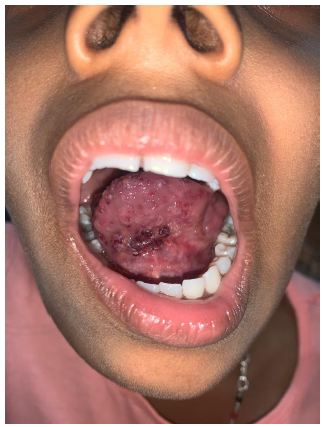
On examination: 7 X 3 cm lesion with irregular surface was noted on the dorsal surface of tongue, extending from posterior portion of anterior 2/3 of tongue till the sulcus terminalis. 2 X 1 cm lesion with irregular surface noted over the floor of mouth. Size and movements of tongue- normal. Bilateral submandibular and jugulodigastric nodes palpable- soft, non-tender, mobile, discrete.
Differential diagnosis:
a) Lingual swelling- Lymphangioma, vascular hamartoma;
b) Sublingual swelling- Plunging ranula, lymphangioma, pleomorphic adenoma or cystic hygroma.
How to proceed?
To narrow down a diagnosis, further investigations are to be done. These may be non-invasive or invasive. Non-invasive investigations include imaging such as ultrasound or CT/MRI, which can reveal if the swelling is cystic/solid, hypo-/hyper-dense, if it is extending to involve the intrinsic or extrinsic muscles of the tongue, and other surrounding structures. Invasive procedure includes excisional biopsy. Histological examination is the only safer way to determine the exact nature of the tongue swellings for the selection of appropriate treatment [4].
Histopathological image of a lingual hamartoma would reveal a mass covered with normal stratified squamous epithelium and mainly composed abundant homogeneous adipose tissue containing muscle tissue and small salivary glands; whereas lymphangioma would be composed of numerous subepithelial lymphatic vessels, some of which may contain coagulated lymph.
Discussion
Swelling in the tongue present a diagnostic and therapeutic dilemma due to their different histo-pathogenesis, nature and subsequently their behavior. Slowly growing, painless, non-ulcerative growths are usually benign while presence of pain, bleeding, ulcer, and induration are characteristic for malignancy. However, some overlapping clinical features are encountered. Therefore, biopsy is usually required to differentiate benign lesions from premalignant and malignant lesions [2,5,6].
Hamartoma is derived from the Greek word ‘hamartia’ meaning fault or defect and ‘oma’ denoting tumour. It is defined as a non-neoplastic developmental malformation, comprising of normal mature cells which are native to the anatomic location [7].
Lingual hamartoma is a rare tongue mass, primarily diagnosed in childhood presenting as an exophytic growth or flat pigmented lesion. Most of the lingual hamartomas demographically occur in young aged children, with female preponderance. According to definition, all lesions are present at birth but age of presentation for excision ranges between 1 month to 61 years [8-10].
Lymphangioma are hamartomatous, congenital malformations of the lymphatic system. In the oral cavity, this lesion is common in the first decade of life and mostly occurs on the dorsal surface and lateral border of the tongue. It rarely arises on palate, gingival, buccal mucosa and lips.
Treatment depends on their size, location and infiltration to the surrounding tissues [11]. Nonsurgical therapy like sclerosing therapy has been suggested for recurrent and unresectable cases. Presently OK-432 is the preferred intralesional sclerosant. It is a lyophilized mixture of low virulent Su Strain of type III group A Streptococcus pyogenes. When administered intralesionally it causes inflammation and infiltration with neutrophils and macrophages. These not only change the consistency of the tumour but also cause a marked reduction in size and improvement in cosmetic appearance. With respect to the current case, this mode of treatment will be chosen as the child has already undergone surgery previously. In recent years, Carbon dioxide and Neodymium Yttrium Aluminium Garnet (Nd-YAG) laser photocoagulation surgery has become popular. Otherwise, surgical excision is the treatment of choice with the inclusion of a surrounding border of normal tissue. But this may cause injury to muscles and nerves. Furthermore, in-toto excision is only possible in about 40% of the cases, and these anomalies have high incidence of recurrence (as in this case).
Conclusion
In general, although not that common, lingual hamartoma and lymphangiomas should be considered as a differential diagnosis of a tongue lesion, especially in paediatric age group. Proper history, clinical examination, imaging techniques and histopathological examination help us derive at the final diagnosis, for which appropriate treatment modality is chosen.
Complete surgical excision of the lesion, is almost always suggested, but there are chances of recurrences as mentioned.
References
- RJ Gilbert, VJ Napadow, TA Gaige, VJ Wedeen. Anatomical basis of lingual hydrostatic deformation. The Journal of Experimental Biology. 2007: 210(23); 4069-4082.
- BV Reamy, R Derby, CW Bunt. Common tongue conditions in primary care. American Family Physician. 2010: 81(5); 627-634.
- Sunil J, Kurien A, Mukunda A, Basheer, Deepthi. Common superficial tongue lesions. Indian Journal of Clinical Practice. 2013: 23(9); 534-542.
- Manar A, Yussif NM. Nonneoplastic tongue swellings of lymphatic and lymphocytic origin: Three case reports. Case reports in dentistry. 2016: 3180239; 5 pages.
- S Bansal, S Dhingra, R Kanojia, A Gupta. Lymphangioma neck presenting as a secondary lesion of the tongue. Online Journal of Health and Allied Sciences. 2012: 11(1); 18.
- S Verghese, V Rupa, S Kurian. Schwannoma of the base of tongue. Indian Journal of Otolaryngology and Head and Neck Surgery. 1996: 48(3); 228-229.
- Patil S, Rao RS, Majumdar B. Hamartomas of the oral cavity. J Int Soc Prev Community Dent. 2015: 5; 347-353.
- Kreiger P, Ernst L, Elden L, Kazahaya K, Alawi F, Russo P. Hamartomatous tongue lesions in children. The American Journal of Surgical Pathology. 2007; 31(8): 1186-90.
- Nava-Villalba M, Ocampo-Acosta F, Seamanduras-Pacheco A, Aldape-Barrios B. Leiomyomatous hamartoma: Report of two cases and review of the literature. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontology. 2008; 105(4): e39–e45.
- Goold A, Koch B, Willging J. Lingual Hamartoma in an Infant: CT and MR Imaging. American Journal of Neuroradiology. 2007; 28(1): 30-31.
- Usha V, Sivasankari T, Jeelani S, Asokan GS, Parthiban J. Lymphangioma of the tongue– A case report and review of literature. J Clin Diagn Res. 2014; 8: ZD12-4.