Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
Adrenocortical adenoma in a six-year-old Egyptian boy
Eman B Kamaleldeen1*; Shimaa Kamal Mohamed1; Kotb Abbass Metwalley1; Hamdy M Ibrahim2; Rania Makboul3; Hassan A Abolella4; Hanaa A Mohammad1
1Pediatrics Endocrinology Unit, Department of Paediatrics, Faculty of Medicine, Assiut University, Egypt.
2Department of Radiology, Faculty of Medicine, Assiut University, Egypt.
3Department of Pathology, Faculty of Medicine, Assiut University, Egypt.
4Department of Urology, Faculty of Medicine, Assiut University, Egypt.
*Corresponding Author : Eman B Kamaleldeen
Pediatrics Endocrinology Unit, Department of Pediatrics, Faculty of Medicine, Assiut University, Assiut,
71515. Egypt.
Email: eman.kamaleldeen@aun.edu.eg
Received : Mar 01, 2021
Accepted : Apr 05, 2021
Published : Apr 07, 2021
Archived : www.jcimcr.org
Copyright : © Kamaleldeen EB (2021).
Abstract
Although adrenal cortical tumors are rare in children, pediatricians should be very cautious about it. Neoplasm is a rare but significant cause of Cushing’s syndrome. Unfortunately, they can be missed very easily, as there is often a time lag between the onset of the symptoms and final diagnosis.
Here, we present a case of adrenal adenoma in a six-year - old Egyptian boy who regrettably misdiagnosed twice as exogenous Cushing syndrome and simple obesity. Diagnosis of an adrenal cortical tumor was confirmed by laboratory data, MRI and histopathological examination after more than 2 years of the onset of his symptoms. After resection of the tumor, serum steroids normalized, and clinical signs receded. The child received no additional treatment and remains disease-free after 18 months of close observation. The possibility of neoplasms should always be considered early to avoid delayed diagnosis and treatment of Cushing’s syndrome.
Keywords: Cushing’s Syndrome, Adrenal Tumors, Obesity.
Citation: Kamaleldeen EB, Mohamed SK, Metwalley KA, Ibrahim HM, Makboul R, et al. Adrenocortical adenoma in a sixyear-old Egyptian boy. J Clin Images Med Case Rep. 2021; 2(2): 1043.
Case report
This male patient is the first live-born baby to his non-consanguineous parents after an uneventful pregnancy and delivery. His birth weight was average, and he was breastfed and had normal dietary habits. He showed normal physical and mental development during the first two years of life. At the age of 2 years, he developed recurrent wheezy chest for which he was treated empirically by bronchodilators and repeated courses of corticosteroids. At the age of 4 years, he started to be obese without other manifestations. When parents sought medical advice for this obesity, 24 hours urinary cortisol was assessed, and it was normal. Parents were told that this obesity may be attributed to recurrent steroid courses and advised to stop steroid therapy. In spite of this, the patient continued to gain weight and he was interpreted as simple obesity.
At the age of 6 years, the boy was presented to the endocrinology clinic of Assiut University Children Hospital because of the progressive unexplained weight gain. There was no family history of obesity and the patient did not receive exogenous steroid for 2 years. Child’s anthropometric measurements showed a weight of 35 kg (>97th percentile), height was 105 cm (<3rd percentile) with BMI >95th percentile for age and sex. On examination: the child had plethoric moon face with truncal obesity, centripetal obesity, abdominal purple cutaneous striae, pubic hair (Tanner stage P2) and prepubertal testicular size, with no axillary hair, hyperpigmentation or acne (Figure 1a).
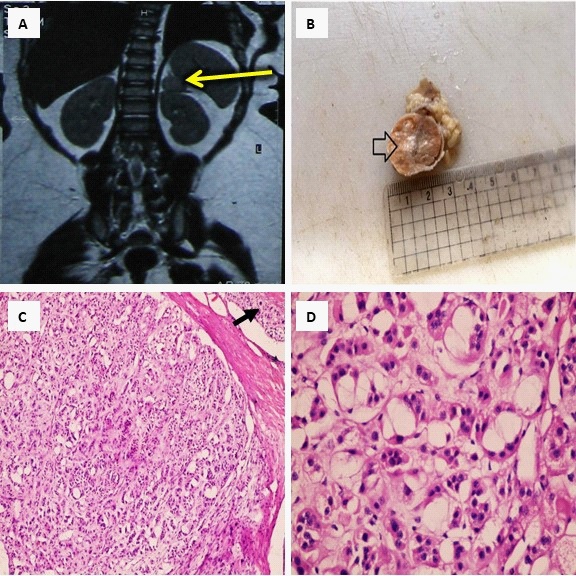
His blood pressure was 120/80 (>95 centile for age). Abdominal examination revealed no palpable masses. Other systems examination was normal. Bone age was delayed; corresponding to the chronological age of 4 years. Laboratory investigations revealed normal fasting and postprandial blood glucose and serum electrolytes. The adrenal hormones study showed normal serum cortisol at 8 Am (16.41 μg/dl) and raised at 8 Pm (21.4 μg/dl), while serum ACTH was low at both Am and Pm (1.53 and 1.00 pg/ml). Twenty-four hours urinary cortisol was high (295 μg/24hs) and testosterone level was 0.4 ng/dl. Serum TSH, fT4 was normal, FSH and LH levels were in the prepubertal levels, and urinary Vanillylmandelic Acid (VMA) was within normal ranges. Abdominal ultrasonography showed fatty infiltrated liver with normal both adrenal glands, while MRI abdomen showed a well-defined near rounded soft tissue mass lesion seen in left adrenal gland measuring about 2 X 2 X 1.5 cm being isointense signal in T1W1, intermediate signal in T2W1, and hyperintense signal in STIR (Figure 2a). Left adrenalectomy was done by pediatric urology surgeon after preoperative preparation of the patients with steroid. The oral steroid was continued after the operation and withdrawn gradually to avoid adrenal crisis. The gross picture showed 2.4 X 2 X 1 cm single mass with a firm to soft smooth capsulated orange outer surface and surrounded partially by fat (Figure 2b). Serial sections revealed soft to firm orange cut sections with some white and grayish areas. The microscopic picture revealed capsulated benign neoplasm formed of cells with abundant foamy cytoplasm in some areas and eosinophilic cytoplasm in other areas. No picture of atypia, necrosis or mitosis (Figure 2c & 2d). Diagnosis of adrenocortical adenoma was confirmed. Eighteen months follow up showed that the boy’s height increased to 116 cm (75th percentile) with a weight reduction to 25 kg (75th percentile) as shown in (Figure 1b), and disappearance of the pubic hair. Postoperative hormonal levels normalized, and MRI at 18 months of follow up is free.
Discussion
Adrenal Cortical Tumors (ACTs) constitutes less than 0.2% of all pediatric neoplasms and account for 6% of all adrenal tumors in children with an estimated incidence of 0.3 per million population. However, the incidence of ACTs varies across geographic regions and is remarkably high in southern Brazil [3].
Here, we present this male patient who started progressive obesity at the age of 4 years but diagnosed at the age of 6 years. The erroneous empiric use of steroids for the management of wheezy chest may add to the misleading interpretation of obesity in this case. Epidemiologic data have suggested that ACTs are more common in girls than in boys, with a 2.5:1 ratio, and there is bimodal occurrence by age, with a peak incidence at less than 5 years and a second peak in the 4th and 5th decades of life [1]. These tumors have been reported to occur more frequently in the left than in the right adrenal gland and high-risk groups include patients with Congenital anomalies of the kidney and congenital adrenal hyperplasia, Li Fraumeni and Beckwith-Wiedemann syndrome [4].
The presenting symptoms of this case were progressive obesity, stunted growth, hypertension, delayed bone age, and striae. These manifestations are consistent with Cushing syndrome due to excess glucocorticoids which could be either of the exogenous or endogenous source. Endogenous production of glucocorticoids may be secondary to increased pituitary ACTH level or primary due to overproduction from the suprarenal gland. The presence of pubic hair, in this case, denotes increased production of androgens as well and highly suggest the suprarenal gland as a source of excess hormones. Although adrenocortical tumors are rare in pediatrics it must be considered as a cause of any unexplained endocrinal symptoms and signs. Functional ACTs secrete hormones, resulting in Cushing's syndrome, virilization, hyperaldosteronism or feminization, while the non-functioning ones are unusual [2]. In general, virilization is the most frequent symptom of ACTs, followed by Cushing syndrome, with hyperaldosteronism being extremely rare.
Laboratory study of adrenocortical tumors should include blood glucose, electrolytes, serum cortisol, androgens, adrenal hormones, and urinary cortisol. These investigations help to differentiate between functioning and non-functioning adrenal neoplasm. The striking lab finding in the present case was the loss of circadian rhythm of cortisol secretion with raised pm level than the am level with suppression of the ACTH levels.
Twenty-four-hour urinary cortisol level was normal when evaluated at the onset of symptoms but became raised lately. The most unusual findings in our case is the presence of pubic hair with normal serum testosterone level. This finding may be attributed to measurement of the total testosterone instead of the free testosterone which is more related to pubic hair development. Also, we didn’t measure testosterone level in the early morning where the highest level is expected due to diurnal variation of testosterone in pre-pubertal boys. Radiological diagnosis of our case was confirmed with MRI while the abdominal ultrasonography was unreliable. It has been reported that ultrasound examination has its limitations in the diagnosis of ACTs. However, it is an important modality for evaluating tumor extension into the inferior vena cava and right atrium. MRI is the most useful imaging procedure for the diagnosis of adrenocortical tumors and may discriminate between benign and malignant lesions.
Surgery is the most effective treatment for adrenocortical tumors, and it seems to be the only hope of a cure. Preoperative corticosteroid replacement is mandatory in the management of adrenocortical tumors as the contralateral adrenal gland is often suppressed. The chemotherapy role is still unclear and reserved for patients with recurrent or metastatic disease or those at high risk of relapse [4]. The role of radiotherapy has not been established [3].
There is a great difference between pathology and clinical outcome, that’s why adrenocortical tumors that lie in this age group should be classified as neoplasms of unknown malignant potential. The pathologic classification of pediatric ACT is troublesome. Even an experienced pathologist can find it difficult to differentiate carcinoma from adenoma. The size of the tumor is larger than 5 cm in diameter, there is more likelihood of carcinoma [1].
Eighteen months follow up of our case showed improvement of anthropometric measurements, hypertension, and disappearance of pubic hair. The hormonal study became within normal range and the MRI abdomen was free. It was reported that among patients who undergo complete tumor resection, favorable prognostic factorsinclude age <4 years, girls, localized tumors, smaller tumor size, signs of virilization alone at presentation, patients with a disease-free interval of >12 months and adenomatous tumor histology [3].
Conclusion
Endocrinal symptoms and signs should be carefully evaluated and followed-up as slowly growing neoplasm can take many years before can be detected by lab and imaging. The most favorable outcome is achieved by early diagnosis and total surgical excision.
Consent: Ethical approval was obtained from the Ethics Board of the Assiut University Children Hospital, Egypt. Written informed consent was obtained from the patient’s parents on behalf of the child for acceptance of publication.
References
- Budhwani KS, Ghritlaharey K, Debbarma MK. Adrenal cortex tumour in a six year girl: A case report and review of literature. Indian Journal of Medical and Paediatric Oncology. 2004; 25: 71.
- Narang GS, Pahwa JS. Cortisol Secreting Adrenal Adenoma in a 5 Year Old Child. Online Journal of Health and Allied Sciences. 2011; 9.
- Ribeiro RC, Figueiredo B. Childhood adrenocortical tumours. European Journal of Cancer. 2004; 40: 1117-26.
- Cho MJ, Kim DY, Kim SC, Kim TH, Kim IK. Adrenocortical tumors in children 18 years old and younger. Journal of the Korean Surgical Society. 2012; 82: 246-50.