Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
Acute stroke management and late referrals-Clinician and community unawareness, A one month case series from Tumbi regional referral hospital Pwani, Tanzania
Adam M Gembe*; Erhad Bilaro
Internal Medicine Department, Tumbi Regional Referral Hospital, Tanzania.
*Corresponding Author : Adam M Gembe
Internal Medicine Department, Tumbi Regional
Referral Hospital, Tanzania.
Email: dr.adamgembe@gmail.com
Received : Mar 30, 2021
Accepted : Apr 28, 2021
Published : Apr 30, 2021
Archived : www.jcimcr.org
Copyright : © Gembe AM (2021).
Abstract
Stroke is among the common emergency department presentations in Tanzania at large. In the developing world, still there are challenges in diagnosis, management and monitoring of these cases hence high morbidity and mortality.
A one month case series is presented here, from Pwani region Tanzania, to demonstrate the encountered challenges.
Keywords: Acute stroke management clinician; Community unawareness.
Citation: Gembe AM, Bilaro E. Acute stroke management and late referrals-Clinician and community unawareness, A one month case series from Tumbi regional referral hospital, Pwani, Tanzania. J Clin Images Med Case Rep. 2021; 2(2): 1092.
Introduction
Stroke is defined as rapidly developing clinical signs of focal (or global) disturbance of cerebral function, with symptoms lasting 24 hours or longer or leading to death, with no apparent cause other than of vascular origin [1]. Stroke is among the leading cause of admissions, disability and deaths both locally and globally [2]. Various factors such as poor healthy seeking behaviors, lack of sophisticated diagnostic tools (CT scan) and timely referral/management of stroke patients, up to 70% of stroke related deaths have been recorded in middle and low income countries [3]. In addition, lack of dedicated stroke units, ambulance services and neurologists further increases mortality among the stroked patients in Sub Saharan Africa (SSA) [4]. On the other hand, In SSA high mortality is observed even in centres where diagnostic tools (CT scan) and neurologist are available due to factors such as unavailability of thrombolytic agents, endovascular thrombectomy, post stroke complications such as aspiration pneumonia and deep vein thrombosis [5].
Despite the ongoing burden, the disease still lacks a thoughtful attention [3].
As it is with other cardiovascular diseases, the risk factors of stroke are numerous to mention a few; hypertension, elevated lipids, diabetes, smoking, low physical activity levels, unhealthy diet and abdominal obesity [3].
The primary goal in management of acute stroke is minimization of neurological damage via timely diagnosis and management [4]. Even though stroke guidelines address the importance of timely management of acute strokes, awareness among clinicians and the community at large remains low in our setup. We present some few cases of stroke referred from satellite health facilities in Pwani region, Tanzania to the regional referral hospital-Tumbi from 1st-31st March 2020 that would have benefited from timely diagnosis and management.
Case 1
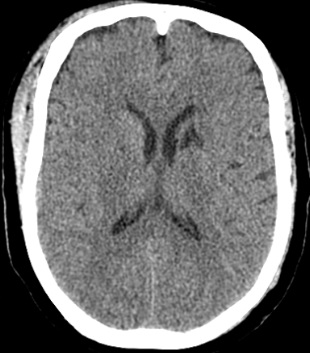
A 47 years male, hypertensive on erratic medications, nondiabetic and non-smoker, referred from one health centre with a diagnosis of severe hypertension. He had an hour history of loss consciousness by the time he arrived at a primary health centre. Assessment was done where recorded Blood Pressure (BP) was 210/100 mmHg, regular pulse of 103 beats per minute, Glasgow Coma Score (GCS) 12/15. Sublingual nifedipine of 20 mg was given and patient was referred to the regional hospital TRRH (Tumbi Regional Referral Hospital) 3 hours later with a BP of 180/90 mmHg. On assessment he had a facial asymmetry and dense hemiplegia on the left side. A diagnosis of stroke due to uncontrolled hypertension was reached and patient was urgently referred to the national hospital for a CT scan images depicted in Figure 1 below.
There is hyper-attenuating lesion involving the right basal ganglia and the right thalamus associated with minimal surrounding edema causing compression of the right lateral ventricle. No significant brain midline shift is noted.
Conclusion: Right basal ganglia and right thalamus hemorrhagic stroke.
Case 2
A 67 years female, newly diagnosed hypertension was referred from a primary health centre with a 12 hours history of loss of consciousness and convulsions despite repeated doses of diazepam. On arrival to the regional hospital TRRH he had a BP of 200/120, GCS of 3/15, equal pupils reacting to light, swollen protruded tongue, obvious facial asymmetry and no signs of menignism. A diagnosis of stroke due to uncontrolled hypertension was made and patient was referred to the national hospital for CT scan images below.
There is hyper-attenuating lesion in the RT basal ganglia with associated intraventricular extension.
Conclusion: RT basal ganglia hemorrhagic stroke with associated intraventricular extension.
Case 3
A 42 years female, hypertensive on erratic medications, presented at the primary health facility with acute speech difficult and dense weakness on the right side. BP noted on the referral letter was 180/100 mmHg. The attending clinician made a diagnosis of “Neurological Disease” and the patient was referred to the regional hospital TRRH on the third day of admission for further management. At arrival the admitting team reviewed and came up with a diagnosis of a stroke and patient was referred to the national hospital for CT scan images below.
There is hypo-attenuating lesion in the left basal ganglia
Conclusion: LT Basal ganglia ischemic stroke
Discussion
The above cases are among many other patients that we receive on daily basis in our regional hospital. Although, there are challenges in early hospital presentation among patients, but also insufficient diagnosis formulation and late referrals from primary health facilities is still a problem. In a study done in Asia, Philippines, failure to recognize symptoms of stroke, nonneurologist consultation and lack of CT scan were the factors associated with inadequate acute stroke management [6]. On the other hand, in SSA most patients seek for traditional healers or prayers. Furthermore, there is lack of required medical personnel, late referrals and inadequate medical instrument at large [4,7].
Use of thrombolytic agents in ischemic stroke is limited in our set up not only due to unavailability of CT scans in all regional hospitals but also late hospital presentation. In Asia, India, Lack of public awareness, inaccessibility to emergency medical services, lack of prioritizing triage system at emergency rooms, radiology, stroke units and lack of a multi‑disciplinary stroke care team contributed to barriers to thrombolysis [8]. In addition, window period to tissue plasminogen activator administration remains a challenge to most General Practitioners (GP) as revealed among GPs in Pakistan [9]. On the other hand, in some SSA countries where diagnostic imaging facilities are available still thrombolysis remains to be a night mare. This is due to a number of reasons; late arrival to thrombolytic capable centres, costs and medical team incapability to administer the agents [5,10].
Lack of stroke awareness at the community, primary and occasionally secondary health facility level has been a setback to adequate acute stroke management in our setup. In the same way a study done in Indonesia revealed up to 67.3% of patients delayed to medical services due to unawareness of stroke symptoms and lack of transport [11]. Similar findings were found in a systematic review of stroke care services in Africa [10]. A community based study in the Northern part of Tanzania further found that up to 61% of study participants were unaware of the stroke symptoms however, 88.3% of them responded that they would have seek for hospital services if they would have had a stroke [12].
Furthermore, non-adherence to hypertensive medication is a huge problem among hypertensive patients in developing countries, especially among symptoms free patients [13]. Non adherence to medication is also compounded by the clinician inexperience with management of hypertension and the patient feeling that anti-hypertensive medications should only be taken for a short time [14]. Considering the anticipated rise of hypertensive cases, more complications are to be expected if proper education is not provided [15].
Conclusion
In reference to this case series, acute stroke management remains unaddressed burden in our setup that leads to increased morbidity and mortality. Furthermore, we think it’s high time to perform outreach programs to satellite health facilities to raise awareness of common stroke presentation and immediate response of attending clinicians to transfer these patients to facilities where adequate management can be given. Additionally, regional hospitals should be equipped with brain CT scans and thrombolytic agents should be made available at affordable costs.
References
- Truelsen T, Begg S, Mathers C. The global burden of cerebrovascular disease. 2001.
- Hertz JT, Sakita FM, Limkakeng AT, Mmbaga BT, Appiah LT, et al. African Journal of Emergency Medicine The burden of acute coronary syndrome, heart failure, and stroke among emergency department admissions in Tanzania: A retrospective observational study. African J Emerg Med. 2019; 0–1.
- Johnson W, Onuma O, Sachdev S. Stroke: A global response is needed. 2016.
- Bc E. Challenges of the Management of Stroke in Sub Saharan Africa: Evaluating Journal of Pediatric Neurology & Challenges of the Management of Stroke in Sub Saharan Africa: Evaluating Awareness, Access and Action. 2018.
- Regenhardt RW, Biseko MR, Shayo AF, Mmbando TN, Grundy SJ, Xu AI, et al. Opportunities for intervention: Stroke treatments, disability and mortality in urban Tanzania. 2018; 1–8.
- Yu RF, Cristina M, Jose ZS, Manzanilla BM, Oris MY, et al. Sources and reasons for delays in the care of acute stroke patients. 2002; 199: 49–54.
- Gadama YG, Mwangalika G, Kinley LB, Jackson B, Mwandumba HC, et al. Case Report Challenges of stroke management in resource-limited settings: A case-based reflection. 2017; 189–193.
- Gurav SK, Zirpe KG, Wadia RS, Pathak MK, Deshmukh AM. Problems and limitations in thrombolysis of acute stroke patients at a tertiary care center. 2013; 265–269.
- Shahzad W, Hassan M. Awareness of stroke among general Practitioners. 2018; 13: 13–19.
- Akinyemi RO, Adeniji OA. Stroke Care Services in Africa: A Systematic Review. 2018; 1: 55–64.
- Misbach J, Ali W. Stroke in Indonesia: A first large prospective hospital- based study of acute stroke in 28 hospitals in Indonesia. 2001; 8: 245–249.
- Hertz JT, Madut DB, William G, Maro VP, Crump JA, et al. Perceptions of Stroke and Associated Health-Care-Seeking Behavior in Northern Tanzania: A Community-Based Study. 2019; 27710: 41–47.
- Osterberg L, Blaschke T. Adherence to Medication. 2005; 487– 497.
- Article O. Determinants of high blood pressure and barriers to diagnosis and treatment in Dar es Salaam, Tanzania. 2016; 2353–2364.
- Risk NCD, Collaboration F. Trends in adult body-mass index in 200 countries from 1975 to 2014: A pooled analysis of 1698 population-based measurement studies with 192 million participants. Lancet. 2014; 387: 1377–1396.