Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
Extensive surgery for peritoneal tuberculosis, an ongoing diagnostic challenge in resource limited setup
Richard Kiritta1*; Fatma Mrisho1; Cosmas Mbulwa2 ; Andrea Solnes Miltenburg3; Albert Kihunrwa1
1 Department of Obstetrics and Gynecology, Bugando Medical Centre, Catholic University of Health and Allied Sciences, Mwanza, Tanzania.
2 Central Pathology Laboratory, Bugando Medical Centre, Catholic University of Health and Allied Sciences, Mwanza, Tanzania
3 Department of Obstetrics and Gynecology, Akershus University Hospital, Lorenskog, Norway
*Corresponding Author : Richard Kiritta
Department of Obstetrics and Gynecology, Bugando
Medical Centre, Catholic University of Health and
Allied Sciences, Mwanza, Tanzania.
Email: kiritta2002@yahoo.com
Received : Mar 31, 2021
Accepted : Apr 28, 2021
Published : Apr 30, 2021
Archived : www.jcimcr.org
Copyright : © Kiritta R (2021).
Abstract
Background: Peritoneal Tuberculosis is an abdominal form of Tuberculosis that affects the peritoneal cavity and enclosed organs. Clinical presentation of this rare form of extrapulmonary tuberculosis resembles that of advanced ovarian cancer and may results in unnecessary extensive surgery especially in resource limited setting.
Case presentation: A case of a 36 years old prisoner who presented to us with gradual onset of abdominal distension for one-month, mild abdominal pain and noticeable progressive weight loss. Physical examination revealed she was underweight, afebrile and had a healed sub umbilical median incision scar on a glossily distended abdomen with positive fluid thrill and shifting dullness. She was HIV negative, anemic and had marked elevation of Cancer Antigen 125 marker. Abdominal ultrasound scan showed ascites with multiple cysts originating from the left iliac fossa and the abdominal pelvic CT scan showing left ovarian cyst, ascites of 3 litres and diffuse peritoneal carcinomatosis. Advanced ovarian cancer was suspected and intra-operatively 2.5 liters of straw colored ascitic fluid was found, the bowels and the omentum were covered with diffuse intestinal nodules and multiple inclusion cysts occupying the pelvic cavity. Histopathological analysis of sampled tissues revealed Peritoneal Tuberculosis.
Conclusion: Peritoneal tuberculosis shares similarities in presentation to advanced ovarian cancer and should be ruled out in a woman suspected of ovarian cancer before proceeding with surgery. For proper differentiation of the two, histopathological analysis of sampled tissue through frozen section biopsy is the preferred approach in resource limited setup where laparoscopic biopsy or ultrasound guided biopsy is not feasible.
Keywords: Tuberculosis; Extrapulmonary Tuberculosis; Peritoneal Tuberculosis; CA-125; Laparotomy; Histopathology
Citation: Kiritta R, Mrisho F, Mbulwa C, Miltenburg AS, Kihunrwa A. Extensive surgery for peritoneal tuberculosis, an ongoing diagnostic challenge in resource limited setup. J Clin Images Med Case Rep. 2021; 2(2): 1093.
Introduction
Peritoneal Tuberculosis is a form of Extrapulmonary Tuberculosis that affects the peritoneal cavity and its enclosed organs. Like other form of EPTB, its clinical presentation is nonspecific and often mimics the presentation of advanced ovarian cancer. We present a case of Peritoneal Tuberculosis that we believe might be among many that undergo unnecessary extensive surgery under the presumptive diagnosis of ovarian cancer either due to lack of awareness of the condition or diagnostic limitations especially in resource limited setup like ours. We describe the clinical presentation, diagnostic modalities, challenges in making pre-operative diagnosis and the management plan for such a case.
Case presentation
We present a case of a 36 years old nulliparous lady, a prisoner who was referred to our facility 6 months after undergoing laparotomy for a suspected pelvic mass at a peripheral facility. In this current admission, she presented with abdominal distension which started gradually 1 month after the first surgery, mild abdominal pain and noticeable progressive weight loss. Six months before the current admission she was diagnosed to have a uterine myoma and underwent Total Abdominal Hysterectomy at the referring facility, full recovery was established and the patient was discharge home.
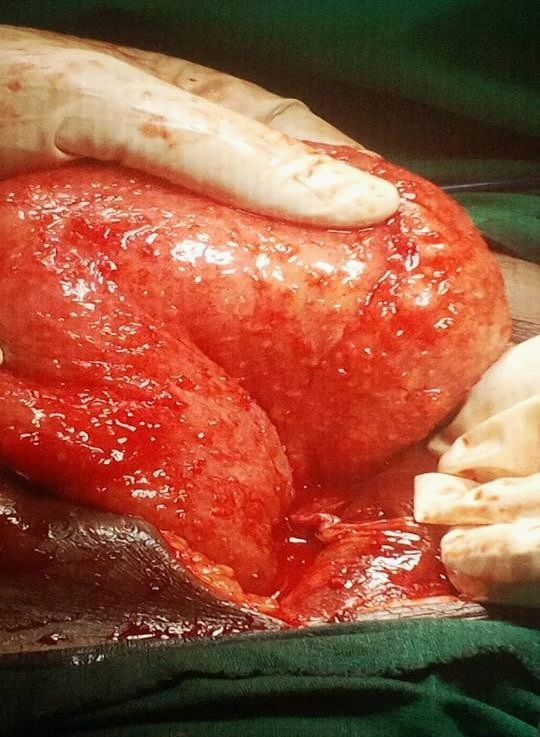
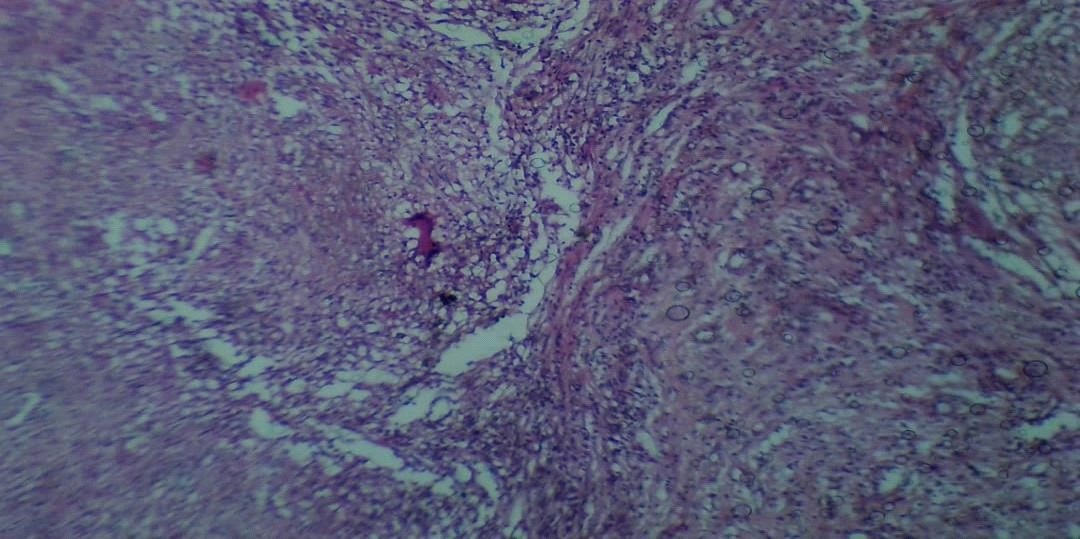
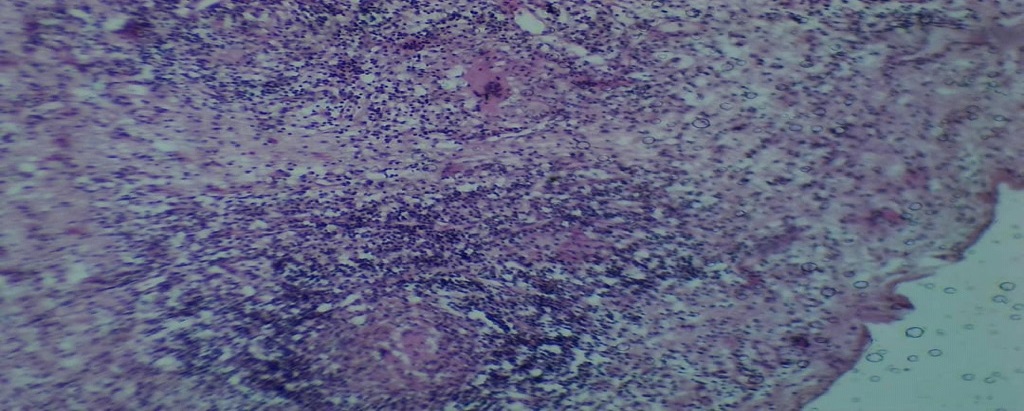
During the course of the current admission, she had undergone ascitic tapping twice at the periphery facility to relieve her of pressure symptoms however no analysis was done on the fluid that was removed. In her current admission, physical examination revealed a middle-aged lady, underweight with a Body Mass Index of 16.5 kg/m2 , afebrile at 37.40 C, and a blood pressure of 110/65 mmHg. Abdominal examination revealed a healed sub umbilical median incision scar on a glossily distended abdomen that had a positive fluid thrill and shifting dullness. Her blood work showed she was HIV negative, had mild anemia of 9.3 g/dl with normal leukocytes, normal range of renal and liver function test parameters for her age, and elevated Cancer Antigen 125 level of 366 ng/dl (normal range (0-35 ng/dl). Abdominal Ultrasound Scan showed massive ascites and multiple pelvic cysts with the largest measuring 5 X 4 cm originating from the left iliac fossa. The patient was taken for an abdominal pelvic CT scan which showed a left ovarian cyst of 4.76 X 5.46 X 6.7 cm with ascites of 3 litres. A provisional diagnosis of advanced stage ovarian cancer was made from the above-mentioned workout and patient was planned for explorative laparotomy and surgical staging. Intraoperatively 2.5 liters of straw colored ascitic fluid was found, the bowels and the omentum were covered with diffuse intestinal nodules (Figure 1) and multiple inclusion cysts with the largest approximately measuring 4 X 3 X 4 cm were also seen in the pelvic cavity enclosing the left ovary, the uterus was not present as it had been removed in the first surgery, the right ovary appeared normal. Complete surgical staging was done, ascitic fluid taken for cytology and gene expert while the sampled tissues were submitted for histopathological analysis. Gene expert for ascetic fluid taken was negative while tissue biopsy stained with H and E showed peritoneal tissue composed of focal areas of caseous necrosis, numerous langhans giant cells, histiocytes and lymphocytes, all suggesting peritoneal Tuberculosis (Figure 2 & 3).
Two weeks after laparotomy, the patient was seen at the TB clinic and antituberculosis drugs were initiated. A combination of isoniazid, rifampin, ethambutol and pyrazinamide was given for the first two months of intensive treatment phase followed by four months of continuous treatment phase that the patient was on rifampin and isoniazid. Marked improvement was seen during the course of treatment and she was finally discharge from TB-clinic 2 weeks after completion of her medication, on the day of discharge her body weight had slightly increased, had no fever, no abdominal distension, no ascites or tenderness.
Discussion
Tuberculosis is a chronic granulomatous disease caused by Mycobacterium Tuberculosis [1]. It is a disease that commonly affects young adults in areas where social and economic determinants of ill health prevail, with 95% of deaths occurring in the developing world [2]. Tuberculosis mainly affects the lungs leading to Pulmonary Tuberculosis which is the most transmissible form of the disease, but tubercle bacilli can spread to other parts of the body and cause Extra- Pulmonary Tuberculosis (EPTB) [3]. Globally, tuberculosis incidence rates have been on the decline since 2001 with absolute number of incident cases starting to fall slowly since 2000 [4], however, the rate of EPTB in particular has not been decreasing in most parts of the world [5].
Close contact with a Tuberculosis infected person, being a health care workers, overcrowding and indoor air pollution are recognized risk factors that may increase exposure to contracting Tuberculosis while malnutrition, HIV infection, cigarette smoking and diabetes mellitus may increase progression to infection upon exposure [6,7]. The patient presented in this case, like in other related case [8] did not have any co morbidities that could interfere with her immunity, however being an inmate (prisoner) in a correction facility in Tanzania increases an individual’s risk of contracting Tuberculosis [9], as is documented in other settings across Africa [6,10].
Unlike clinical presentation of PTB, the presentation of EPTB is usually so protean that diagnosis and identification is often delayed, and requires special clinical alertness to recognize the condition [11]. This was evident in our patient’s case in which an extensive surgery was done to a patient under the presumptive diagnosis of advanced ovarian cancer rather than peritoneal tuberculosis due to difficulties in diagnosis. Peritoneal Tuberculosis is an abdominal form of Tuberculosis that affects the intestinal tract, liver, spleen, female genital tract, the omentum, the parietal and visceral peritoneum. It represents 1-2% of all forms of TB [12,13]. Fever, abdominal pain, abdominal swelling with ascites and weight loss are among prominent features for peritoneal tuberculosis [14], however advanced ovarian cancer may share some of these clinical presentations, making differentiation of these two conditions necessary for proper case management. The patient in this case presented with abdominal swelling with ascites, mild abdominal pain and history of weight loss, all together of which were pointing towards the diagnosis of ovarian cancer or peritoneal tuberculosis.
Several laboratory blood work ups and imaging investigations are often utilized to help a clinician arrive to the correct diagnosis. CA 125 was found to be significantly elevated in our patient. This protein produced by ovarian surface epithelium has been used for surveillance of development of ovarian cancer and to monitor response of chemotherapy for ovarian cancer [15]. However, CA125 is not specific to ovarian cancers as it is found to be elevated in different benign and malignant conditions like pregnancy, endometriosis, uterine fibroid, pancreatitis and liver cirrhosis. Peritoneal derived CA125 significantly contributes to circulating CA125 and may cause the levels to rise in conditions that cause peritoneal irritation, as it may occur with hyperstimulation of the peritoneum, salpingitis, ruptured ectopic pregnancy, and peritoneal inflammation. The raised CA125 in our case was more likely a result of peritoneal irritation and inflammation by tuberculosis and not ovarian cancer as was observed in other related cases [16,17], highlighting the restriction on the use of CA 125 as a single diagnostic tool.
Abdominal pelvic CT scan on our patients revealed a left ovarian cyst and massive ascites, features that highly suggested a malignancy appearance. Similar observation was made in abdominal pelvic CT scan results in some other cases, all of which suspected ovarian malignancy [16,18]. Our image findings further concur with the observation that radiologic imaging techniques are not sensitive or specific for diagnosing peritoneal tuberculosis [19,20].
Diagnostic laparoscopy aiming at obtaining tissue sample for frozen-section analysis is currently the best, direct and least invasive procedure that can assist a clinician arriving to the correct diagnosis and avoid extensive surgery [17,21]. However, in our case, and few other related cases that occurred in resource scarce setting, equipment and human resource limitation resulted in failure to do diagnostic laparoscopy or frozen-section analysis respectively, resulting into an extensive surgery on suspicion of ovarian cancer. Peritoneal biopsy under percutaneous radiological guidance offers an alternative to surgery by providing a minimally invasive method in diagnosing peritoneal tuberculosis with minimal complications [22].
Ascites, small nodules in the peritoneum, omentum, small bowel loops, uterus and the pelvic walls together with adhesions between bowel loops are some of the noted macroscopic findings in peritoneal tuberculosis [16,23]. These findings are often noted in advance ovarian cancer and warrant additional analysis to avoid misdiagnosing these two conditions. Massive ascites, diffuse intra-abdominal nodules and multiloculated cysts on the left adnexa were observed in our patient’s case, and as of such additional analysis was requested.
Acid fast bacilli, Ziehl-Neelsen staining and Gene expert of aspirated ascitic fluid all came back negative for tuberculosis in our patient’s case. Our findings further highlight the reported low sensitivity rates of acid-fast bacilli and Ziehl-Neelsen staining in detection of Tubercle bacilli in ascitic fluid [24-26], and the poor sensitivity and specificity of Gene expert in detection of abdominal TB from ascitic fluid samples [27]. The diagnosis of peritoneal tuberculosis in our case, like other related cases [17,18] was made through histological examination of intraoperative collected tissue samples, further stressing the need of pathological examination of samples as the gold standard for definitive diagnosis of peritoneal tuberculosis [28,29].
Abdominal tuberculosis is generally responsive to medical treatment. Isoniazid, rifampin, pyrazinamide, ethambutol, and streptomycin are the five common first line medication for treatment of Tuberculosis with treatment duration consisting of a four-drug regimen administered for 2 months then continuation of treatment with rifampin and isoniazid for 4 or more months [30]. In our patients’ case, Isoniazid, rifampin, ethambutol and pyrazinamide were given for the first two months followed by isoniazid and rifampin for four months.
Though some authors are recommending longer treatment duration for up to twelve months [31,32], retrospective series [33] have seen no evidence to support such a recommendation because majority of patients are cured with the treatment regime of six months, as marked by resolution of symptoms and disappearance of ascites [30] as was seen in our patients’ case.
Conclusion
Lack of awareness and resource limitation offers diagnostic challenges for Peritoneal Tuberculosis in developed and less developed world respectively. High degree of suspicion is required to diagnose Peritoneal tuberculosis due to shared similarities in presentation to advanced ovarian cancer. Histology results to rule out the possibility of Peritoneal Tuberculosis through frozen section or mini laparotomy should be obtained before proceeding with extensive surgery especially in reproductive aged women suspected of having advanced ovarian cancer.
Patient’s perspective: The care provided was timely with full explanation of the diagnosis and prognosis and with a follow-up plan explained.
Acknowledgements: We are humbly grateful for the support given by the Gynecology Department and the Central Pathology Laboratory at Bugando Medical Centre.
Timeline: The patient was admitted on January 2020 were clinical workout and management was initiated immediately. Surgery was done on the 7th days post admission after which she stayed in the ward for one week for post-surgical care then discharged through medical outpatient Tuberculosis clinic where anti Tuberculous treatment was initiated and follow up continued. Preparation and completion of the case report took 3 months, with the case presented in Gynecology department.
Authors’ contributions: RK and FM played equal roles in the preparation of this case report. The other coauthors contributed to the management of the patient and the writing of the case report. All authors read and approved the final manuscript.
Funding: The cost of care offered to this patient was partly covered by the patient and some was waived by the hospital administration. The cost of preparing this manuscript was covered by the authors.
Ethics approval, consent to participate and publish: Written informed consent was obtained from the patient for publication of this case report and related images. A copy of the written consent is available for review by the Editor-in-Chief of this journal. Additionally consent was sought and ethical clearance number CREC/441b/2O2O was granted by the joint Catholic University of Health and Allied Sciences/ Bugando Medical Centre Research and Ethical review committee.
References
- Brändli O. The clinical presentation of tuberculosis. Respiration. 1998; 65: 97- 105.
- World Health Organisation, Global tuberculosis report. 2013.
- Kulchavenya E. Extrapulmonary tuberculosis: Are statistical reports accurate?. Therapeutic Advances in Infectious Disease. 2014; 2: 61-70.
- Glaziou P. et al. Global epidemiology of tuberculosis. In Seminars in respiratory and critical care medicine. Thieme Medical Publishers. 2013.
- Ben Ayed H, et al. Extrapulmonary tuberculosis: Update on the epidemiology, risk factors and prevention strategies. Int J Trop Dis. 2018; 1.
- Lienhardt C, et al. Investigation of the risk factors for tuberculosis: A case–control study in three countries in West Africa. International journal of epidemiology, 2005; 34: 914-923.
- Narasimhan P, et al. Risk factors for tuberculosis. Pulmonary medicine. 2013.
- Chow KM, et al. Tuberculous peritonitis–associated mortality is high among patients waiting for the results of mycobacterial cultures of ascitic fluid samples. Clinical infectious diseases. 2002; 35: 409-413.
- Rutta E, et al. Tuberculosis in a prison population in Mwanza, Tanzania (1994–1997). The International Journal of Tuberculosis and Lung Disease. 2001; 5: 703-706.
- O’Grady J, et al. Tuberculosis in prisons in sub-Saharan Africa– the need for improved health services, surveillance and control. Tuberculosis, 2011; 91: 173-178.
- Bukhary ZA, Alrajhi AA. Extrapulmonary tuberculosis, clinical presentation and outcome. Saudi Med J. 2004; 25: 881-885.
- Mimidis K, Ritis K, Kartalis G. Peritoneal tuberculosis. Annals of Gastroenterology. 2005.
- Koc S, et al. Peritoneal tuberculosis mimicking advanced ovarian cancer: A retrospective review of 22 cases. Gynecologic oncology. 2006; 103: 565-569.
- Cavalli Z, et al. Clinical presentation, diagnosis, and bacterial epidemiology of peritoneal tuberculosis in two university hospitals in France. Infectious diseases and therapy. 2016; 5: 193-199.
- Pepin K, et al. CA 125 and epithelial ovarian cancer: Role in screening, diagnosis, and surveillance. American Journal of Hematology/Oncology®. 2014; 10.
- Pepin K, et al. CA 125 and epithelial ovarian cancer: Role in screening, diagnosis, and surveillance. American Journal of Hematology/Oncology®. 2014; 10.
- Wu CH, et al. Disseminated peritoneal tuberculosis simulating advanced ovarian cancer: A retrospective study of 17 cases. Taiwanese Journal of Obstetrics and Gynecology. 2011; 50: 292- 296.
- Fahmi MN, Harti AP. A diagnostic approach for differentiating abdominal tuberculosis from ovarian malignancy: A case series and literature review. In BMC proceedings. 2019.
- Uzunkoy A, Harma M, Harma M. Diagnosis of abdominal tuberculosis: Experience from 11 cases and review of the literature. World journal of gastroenterology: WJG. 2004; 10: 3647.
- Patel SM, et al. Ovarian carcinoma or abdominal tuberculosis?. A diagnostic dilemma: Study of fifteen cases. The Journal of Obstetrics and Gynecology of India. 2012; 62: 176-178.
- Huang B, et al. Comparison between laparoscopy and laboratory tests for the diagnosis of tuberculous peritonitis. Turkish journal of medical sciences. 2018; 48: 711-715.
- Vardareli E, et al. Tuberculous peritonitis of the wet ascitic type: Clinical features and diagnostic value of image-guided peritoneal biopsy. Digestive and Liver Disease. 2004; 36: 199-204.
- Guirat A, et al. Peritoneal tuberculosis. Clinics and research in hepatology and gastroenterology. 2011; 35: 60-69.
- Sanches, I., A. Carvalho, and R. Duarte, Who are the patients with extrapulmonary tuberculosis?. Revista Portuguesa de Pneumologia (English Edition). 2015: 21: 90-93.
- Gutiérrez-Macías, A., et al., Tuberculous peritonitis in a patient with rheumatoid arthritis treated with adalimumab. Clinical rheumatology. 2007; 26: 452-453.
- Bulut Gökten D, et al. A case report of peritoneal tuberculosis: A challenging diagnosis. Case reports in infectious diseases. 2018; 2018.
- Ahmad R, et al. Diagnostic accuracy of peritoneal fluid GeneXpert in the diagnosis of intestinal tuberculosis, keeping histopathology as the gold standard. Cureus. 2018; 10.
- Muroni M, et al., Abdominal tuberculosis: Utility of laparoscopy in the correct diagnosis. Journal of Gastrointestinal Surgery. 2015; 19: 981-983.
- Guirat A, et al. Role of laparoscopy in the diagnosis of peritoneal tuberculosis in endemic areas. Medecine et sante tropicales. 2015; 25: 87-91.
- Sanai, F. and K. Bzeizi, Systematic review: Tuberculous peritonitis–presenting features, diagnostic strategies and treatment. Alimentary pharmacology & therapeutics. 2005; 22: 685-700.
- Tang LC, Cho HK, Taam VCW. Atypical presentation of female genital tract tuberculosis. European Journal of Obstetrics & Gynecology and Reproductive Biology. 1984; 17: 355-363.
- Amouri A, et al. Profil actuel de la tuberculose péritonéale: Etude d’une série tunisienne de 42 cas et revue de la littérature. La Revue de médecine interne. 2009; 30: 215-220.
- Demir K, et al. Tuberculous peritonitis–reports of 26 cases, detailing diagnostic and therapeutic problems. European journal of gastroenterology & hepatology. 2001; 13: 581-585.