Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
A case report of an intra-oral exophytic growth in reaction to Gore-Tex expanded PTFE membrane left in situ for eighteen years
Marc Harrington1; Jamie Toole2; Orlagh McPolin3 ; Nicola Holland1; Gerry McKenna4
1 Restorative Department, School of Dentistry, Royal Victoria Hospital, Belfast, United Kingdom.
2 Oral Surgery Department, School of Dentistry, Royal Victoria Hospital, Belfast, United Kingdom.
3 Dental & Maxillofacial Radiology, Glasgow Dental Hospital, United Kingdom.
4 Centre for Public Health, Queen’s University Belfast, United Kingdom.
*Corresponding Author : Marc Harrington
School of Dentistry, Royal Victoria Hospital, Belfast,
United Kingdom.
Email: marc.harrington@gmail.com
Received : Apr 02, 2021
Accepted : Apr 29, 2021
Published : May 04, 2021
Archived : www.jcimcr.org
Copyright : © Harrington M (2021).
Abstract
This case report explores the challenging multidisciplinary management of a gentleman over the course of 28 years. It begins with resection of a maxillary ameloblastoma, describes an 18-year period of elusive discomfort, culminating in an exophytic lesion associated with a retained Gore-Tex membrane. Retained foreign bodies can cause a multitude of complications including chronic infection, discomfort and reactive tissue growth. Imaging for foreign bodies may have a low diagnostic yield and surgical exploration should be considered when conventional methods fail to provide a diagnosis. The case concludes with successful prosthodontic rehabilitation, lessons with barrier membranes and foreign body management.
Citation: Harrington M, Toole J, McPolin O, Holland N, McKenna G. A case report of an intra-oral exophytic growth in reaction to Gore-Tex expanded PTFE membrane left in situ for eighteen years. J Clin Images Med Case Rep. 2021; 2(3): 1107.
Background
Barrier membranes are frequently used to direct bone regeneration for dental implants and halt the migration of epithelial cells into the regenerating site. Non-resorbable expanded PTFE (ePTFE) membranes, such as Gore-Tex, became standard for bone regeneration in the 1990s. Non- resorbable membranes feature predictable performance but require a second surgery for removal. Foreign bodies in the oral cavity can be difficult to detect, particularly when radiolucent. They may present as recurrent infection, purulent discharge, chronic inflammation, osteomyelitis, reactive soft tissue growth or non-specific pain.
Case report
In 1991 a 41-year-old gentleman was diagnosed with an ameloblastoma of the right maxilla. Oral and Maxillofacial Surgery successfully resected the benign tumour via partial maxillectomy of the UR1 to UR5 region. The defect was initially lined with a split thickness skin graft taken from the thigh and an obturator was constructed. In 1995 there were five general anaesthetics to attain satisfactory grafting of the deficit. This involved three iliac crest grafts and multiple local mucosal flaps.
In 2000 three Branemark implants were placed in the UR2, UR4 and UR6 region under general anaesthetic. Gore-Tex membrane was placed as part of guided bone regeneration for the UR2 and UR4 implants. The UR6 implant failed to integrate and was removed. The UR4 was utilised for magnetic retention of a removable partial obturator. The UR2 implant remained buried and unutilised. Later that year failed mucosal coverage led to a further general anaesthetic for a full thickness mucosal graft. In 2005 discomfort continued in the UR2 region for which the obturator was eased. Eight years later low-grade discomfort persisted in the upper right quadrant. Spiral CT indicated no ameloblastoma recurrence although benign inflammatory changes were noted in the region.
In 2013 the now 63-year-old gentleman was referred from Oral and Maxillofacial Surgery to Restorative Dentistry for prosthodontic management and review of the region of discomfort. The patient reported numerous complications since the resection of the ameloblastoma in 1991. His primary complaint was ongoing low-grade discomfort from his right maxillary incisor region, present for many years, but previous investigations and reviews simply indicated inflammation. Medical history included Parkinson’s, asthma and pernicious anaemia. His current implant retained removable partial obturator was functional, but retention relied primarily on one implant. The UR4 implant was diagnosed with peri-implant mucositis and managed with non-surgical periodontal treatment.
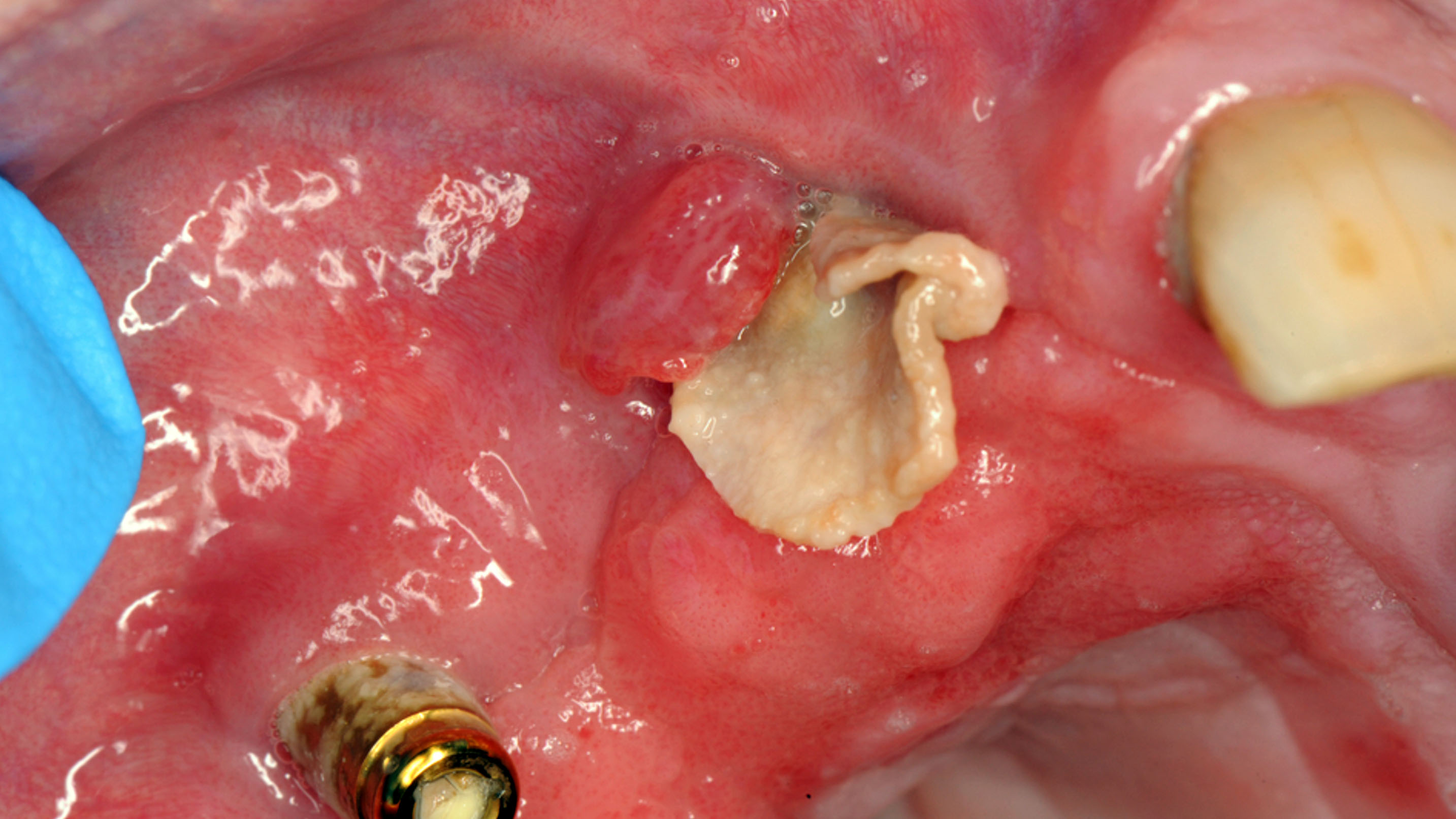
In 2017 the patient attended for review and continued to experience discomfort in the right anterior maxilla. Treatment planning began for a new removable prosthesis. It was discussed the buried implant in the UR2 region could be uncovered and utilised to improve prosthodontic function. A second stage surgery was undertaken under local anaesthetic and a healing cap was placed on the UR2 implant. However, as treatment progressed a concerning exophytic lesion developed buccal to the UR2 site. An urgent referral was made to the Oral Surgery department. Intraoral radiography failed to reveal any foreign bodies (Figure 1). Exploration of the site unveiled the corner of a flat, whitish, fabric-like material (Figure 2). This was removed and sent for analysis by histopathology.
Histological examination revealed a 14 X 9 mm laminated acellular membrane overrun by bacterial colonies. The features were that of a foreign body resembling Gore-Tex membrane. This section of Gore-Tex membrane for guided bone regeneration had been in-situ adjacent to the UR2 implant for eighteen years. This created a nidus for chronic infection. Following removal of this foreign body the chronic symptoms of discomfort finally resolved. The UR2 implant was then utilised for a bar retained prosthesis offering improved retention, stability and quality of life for the patient (Figure 3).
Discussion
Foreign bodies in the mouth may present as acute, recurrent or chronic infection, inflammation, purulent discharge, osteomyelitis, reactive soft tissue growth or non-descript pain [1]. Clinical presentation may mimic other more common conditions. Use of a surgical sieve expands our differential diagnoses and can prevent delayed definitive diagnosis with appropriate management.
An investigative history to understand the timeline of events can help identify a potential foreign body. This can be obfuscated by the transient nature of human memory and recall. Retrospective investigation of clinical notes can clarify the timeline, however multi-centre management of patients can make assimilation of information difficult.
Imaging is recommended for foreign body identification however remains vulnerable to false negatives. Radiographic imaging can have limited diagnostic yield; particularly when an object, such as ePTFE, is radiolucent. Plain film radiographs will not typically reveal ePTFE membranes. The differences in density between ePTFE and the rest of the body mean that high resolution CT and MRI imaging could reveal membranes [2]. In practice this may be difficult to discern, particularly with small scale oral applications of membrane and when scans are taken at standard resolution.
Ultrasound waves pass through established ePTFE but will initially be impeded in the immediate post-operative period, until the membrane is filled by cells and fluid [2].
With hindsight the retained Gore-Tex would have been removed within an appropriate timeframe. There are now evidence-based protocols for membrane use in guided bone regeneration, twenty years ago these were less established. Gore-Tex continues to be used and left permanently in-situ for procedures such as hernia repair. Gore-Tex is biocompatible and when covered should remain inert when strict aseptic protocol is followed.
When non-resorbable membranes are placed for guided bone regeneration, the second surgical intervention for removal of the membrane should be scheduled, typically 3-9 months post- augmentation [3]. ePTFE membrane exposure is a recognised complication that permits a communication of bacteria into the surgical site, risking infection and bone loss [3]. Infection should be treated aggressively as unresolved infection will require premature removal of the membrane.
Expanded PTFE membranes, such as Gore-Tex, are porous in nature, therefore at an increased risk of infection in comparison to dense PTFE [4]. Resorbable collagen membranes are increasingly used, offering progressively comparable outcomes to non-resorbable membranes [5,6]. They have numerous advantages including no barrier removal procedure required with subsequent reduced risk of tissue damage and morbidity [3]. Disadvantages include unpredictable rates of resorption and comparatively inferior mechanical properties which can lead to collapse [3].
Decision to commence surgical exploration should be made on a case-by-case basis. Advantages and disadvantages of exploration should be evaluated when history, examination and imaging have failed to adequately diagnose symptoms associated with a previous surgical site. This foreign body eventually presented as an exophytic lesion, otherwise it may have remained undetected.
This case demonstrates the long pathway a patient with a successfully resected benign tumour can endure. The ameloblastoma was successfully resected, however the defect took multiple surgeries over years to stabilise. The rehabilitation phase with dental implants should improve quality of life, but in this case an undiagnosed foreign body contributed to discomfort for eighteen years.
Conclusion
Retained foreign bodies can cause a multitude of complications including chronic infection and discomfort. The radiolucent nature of PTFE contributed to a protracted period featuring waves of low-grade discomfort and infection with an unknown cause. This case highlights the difficulties in diagnosing a foreign body, the potential limitations of imaging and the importance of considering surgical exploration. Exploration should be considered when clinical history, examination and imaging fail to provide a diagnosis. Surgical exploration comes with its own risks, which must be discussed with the patient as part of the consent process.
References
- Anderson JM, Rodriguez A, Chang DT. Foreign body reaction to biomaterials. Semin Immunol. 2008; 20: 86–100.
- W. L. Gore & Associates. How will ePTFE show up on CT, MRI, x-rays or Ultrasound?. 2021.
- Rakhmatia YD, Ayukawa Y, Furuhashi A, Koyano K. Current barrier membranes: Titanium mesh and other membranes for guided bone regeneration in dental applications. J Prosthodont Res. 2013; 57: 3–14.
- Ronda M, Rebaudi A, Torelli L, Stacchi C. Expanded vs. dense polytetrafluoroethylene membranes in vertical ridge augmentation around dental implants: A prospective randomized controlled clinical trial. Clin Oral Implants Res. 2014; 25: 859–866.
- Jung RE, Fenner N, Hämmerle CHF, Zitzmann NU. Long-term outcome of implants placed with Guided Bone Regeneration (GBR) using resorbable and non-resorbable membranes after 12- 14 years. Clin Oral Implants Res. 2013; 24: 1065–1073.
- Jensen SS, Terheyden H. Bone augmentation procedures in localized defects in the alveolar ridge: Clinical results with different bone grafts and bone-substitute materials. Int J Oral Maxillofac Implants. 2009; 24: 218–236.