Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
A rare case of pituitary apoplexy complicated by internal carotid artery occlusion: Severity obscured by primary collaterals
Klas Holmgren*; Lars-Owe D Koskinen; Peter Lindvall
Department of Clinical Science, Neurosciences, Umeå University, 901 87 Umeå, Sweden
*Corresponding Author : Klas Holmgren
Department of Clinical Science, Neurosciences,
Umeå University, 901-87 Umeå, Sweden.
Email: klas.holmgren@umu.se
Received : Apr 08, 2021
Accepted : May 04, 2021
Published : May 07, 2021
Archived : www.jcimcr.org
Copyright : © Holmgren K (2021).
Abstract
Pituitary apoplexy complicated by internal carotid artery occlusion was encountered in a patient with surprisingly moderate symptoms at presentation. For a short period of watchful waiting, primary collaterals obscured the emergent need for decompressive surgery, which after the sudden onset of neurological deterioration fortunately salvaged imminent cerebral infarction. Although a few similar cases have been described previously, the importance of collateral circulation has been left virtually without comment, while contrasting treatment strategies and high mortality rates suggest further case reports are warranted. Notably, a symptoms-based management seems likely to be insufficient in these rare situations, while our experience indicate early surgery could be judicious to consider.
Keywords: Pituitary apoplexy; Internal carotid artery occlusion; Collateral circulation.
Citation: Holmgren K, Koskinen LOD, Lindvall P. A rare case of pituitary apoplexy complicated by internal carotid artery occlusion: Severity obscured by primary collaterals. J Clin Images Med Case Rep. 2021; 2(3): 1125.
Introduction
Pituitary apoplexy constitutes a rare and emergent syndrome estimated to occur in only a few percent of patients with sellar adenomas [1]. Caused by either or both bleeding and infarction of the pituitary gland, the condition is typically characterised by sudden onset of headache, visual impairment and altered mental status [2]. While cases also complicated by secondary cerebral ischaemia have been reported, such events remain highly uncommon, hence with our current scientific understanding accumulated from a few case reports [3,4]. In these infrequent situations, surgical decompression has been advocated in patients with severe visual field deficits or a declining level of consciousness [3]; however, ideal management and timing of treatment remain controversial [5-7]. Notably, in cases with mechanical compression of cerebral arteries, the potentially treacherous role of sustained perfusion via primary collaterals have scarcely been commented upon in the literature. We herein present the unique case of a 57-year-old female who suffered haemorrhage from a pituitary macroadenoma, with subsequent occlusion of the right cavernous internal carotid artery and delayed ischaemia due to temporarily preserved cerebral perfusion via Willisian collaterals.
Case presentation
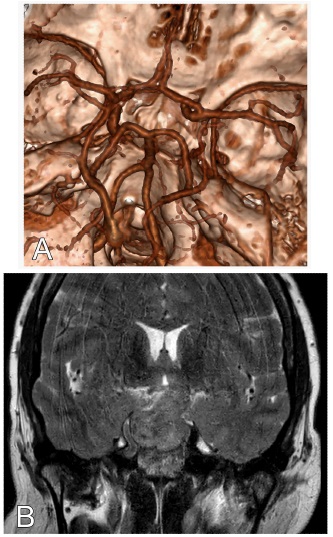
A 57-year-old female with a medical history of type 2 diabetes, systemic hypertension and hyperlipidaemia, presented through the local emergency department, roughly four hours after the ictus of headache and acute onset visual disturbance. Immediate Computerised Tomography (CT) scan of the brain, including a CT angiogram (CTA), displayed sellar haemorrhage from a suspect macroadenoma with occlusion of the right side cavernous internal carotid artery (Figure 1A). The supraclinoid carotid segment, nonetheless, seemed preserved and demonstrated normal filling due to primary collaterals (Figure 1A). More specifically, a thin anterior-communicating artery was identified, whereas a posterior-communicating artery never became visualised, however, seemed plausible in the presence of a posterior cerebral artery of non-fetal appearance (Figure 1A).
On crude initial examination the patient suffered from nausea and vomiting, although, was except from suspect bitemporal hemianopia neurologically intact. As symptoms first seemed moderate and stationary, preliminary plan was to await results of emergent Magnetic Resonance Imaging (MRI), formal ophthalmic examination and complete endocrine evaluation at the regional hospital. However, all investigations were instead arranged for at our referral hospital after swift transfer of the patient early the next morning. On admission, approximately 12- 14 hours after first symptoms, the patient had become slightly drowsy but corresponded to a Glasgow Coma Scale (GCS) score of 15. Her right pupil reacted normally although with a slightly delayed constriction to light on her left side. Motor functions were symmetrically intact, while endocrine assessment displayed hormonal levels were all within normal reference intervals. Subsequent MRI confirmed haemorrhagic pituitary apoplexy with an obliterated internal carotid artery cavernous segment on the right side, still, with vessel patency distal to the stenosis (Figure 1B).
In direct connection with the MRI, some 16 hours after ictus, the patient suddenly worsened during ophthalmic assessment. Still able to communicate, she complained of total blindness, however, had to cancel the examination moments later due to escalating lethargy. She was transferred to the neurointensive care unit, at which new examination revealed a left sided hemiparesis and a GCS score of 8 (E1/V2/M5).
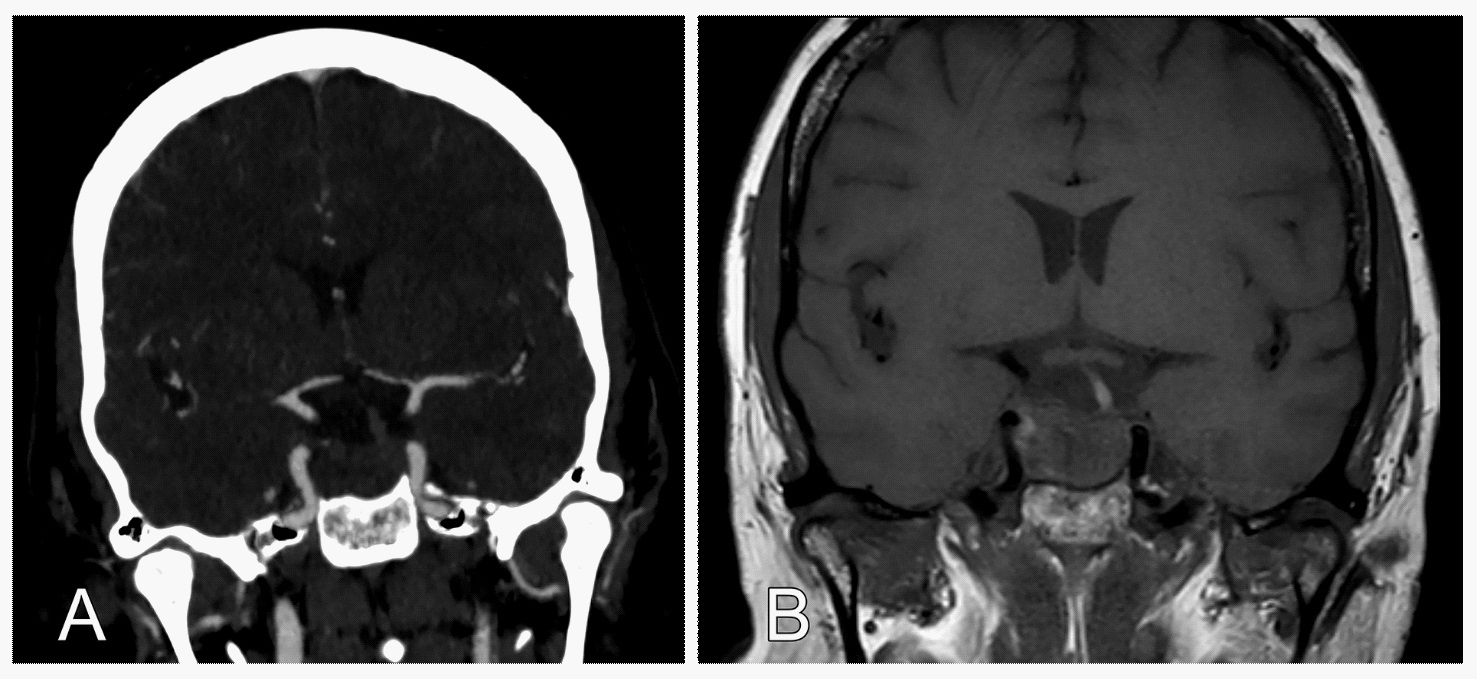
Decision was made to undertake surgical decompression through an endoscopic transsphenoidal approach, and the patient went straightway into the operating theatre. The procedure itself was uncomplicated and the patient was taken to the intensive care unit for postoperative monitoring and extubation. A few hours later, she still exhibited signs of a left side hemiparesis, mainly affecting the upper extremity, after which a new CT and CTA was performed. The studies displayed a restored luminal width of the previously narrowed right carotid artery segment (Figure 2A & B) without any signs of infarction. During the subsequent hours, the patient’s condition progressively improved and she had regained consciousness already the next day. At crude examination, her visual acuity and visual field also appeared dramatically well recovered, while the left side hemiparesis subsided completely within a few days. Except for a short period of cerebrospinal fluid leak terminating spontaneously, the postoperative period was otherwise uneventful, and the patient was transferred back to her regional hospital before discharge home. The final pathological diagnosis was non-functioning pituitary adenoma positive for Steroidogenic factor 1.
Discussion
Pituitary apoplexy followed by mechanical compression of the circle of Willis is a rare, nevertheless fatal, condition. The present report elucidates the importance of primary collaterals in these infrequent events, and how a symptoms-based management may not suffice, as severe ischaemia may evolve abruptly and later than expected.
To date, sellar haemorrhage with vascular occlusion has been described just over 20 times in the scientific literature [3,4,8,9]. While ideal management remains hard to substantiate, a 2015 comprehensive review by Banerjee et al. put forward some evidence in favour of surgery in cases with vascular compression [3]. Additionally, a declining level of consciousness, visual field deficits and visual acuity were suggested symptoms to advocate surgical intervention, whereas manifest cerebral infarction was deemed an insufficient determinant on its own. Interestingly, how collateral circulation may have influenced the severity of symptoms–and temporal facets in particular–were unaddressed. Only recently, however, Elarjani et al. reported on a similar case to the present, who also demonstrated with internal carotid artery compression and a delayed cessation of cerebral blood flow [4]. Although the authors acknowledged a corresponding time window before severe hypoperfusion occurred, underlying mechanisms, including the importance of collaterals, were omitted throughout a more general discussion and updated literature review.
Furthermore, in thromboembolic stroke, it is well established that collateral circulation plays a pivotal role in patient outcomes and the treatment window to draw benefit from reperfusion [10,11]. While primary Willisian collaterals, mainly referred to herein, may be kept distinct from secondary leptomeningeal anastomoses, corresponding mechanisms seem plausible in pituitary apoplexy with secondary ischaemia, and suggest time to treatment might be more crucial than has been previously appreciated. As the vascular anatomy and collateral capacity generally varies between individuals [12], the clinical course after onset of symptoms may differ as well, and thus make some patients more susceptible to secondary ischaemia than others. Hence, we read with interest the report on a similar case by Sussman et al., in which perfusion imaging identified a large penumbra in a comatose patient, who almost fully recovered with immediate sellar decompression [8]. Importantly, however, collateral status and tissue at risk should ideally be assessed early on–most preferably prior to escalating neurological deficits–as the mortality in cases with progressive symptoms is considerable [3,4]. As a consequence, reduced time to surgical decompression may speculatively triumph the need for perfusion imaging in such acute situations, as the superior outcome experienced with prompt intervention in the current report likely mirrors the efficacy recorded with early reperfusion in thromboembolic stroke [13]. Ultimately, principal arguments behind conservative management include the risk of haemorrhagic infarction after revascularisation [5,14]: The risk of which correlates with penumbral size and time to recanalization in particular [15]. Watchful waiting may therefore paradoxically put patients with vascular occlusion in an even worse situation, as the need of surgery seems to be merely postponed [4,8].
Conclusion
Pituitary apoplexy complicated by major vessel occlusion remains an exceptionally rare condition associated with profound morbidity and mortality; hypothetically to some extent due to the underrecognized importance of collateral circulation. More specifically, prior studies suggest a symptoms-based management likely to be insufficient in these settings, as primary collaterals may provide a window of treatment, during which impending cerebral ischaemia may go unnoticed, until abrupt hypoperfusion ensues. The present report will hopefully help add to our limited understanding of these challenging conditions, and foremost, make clinicians faced with similar situations aware of the risk of delayed neurological deterioration owing to collateral circulation.
Informed consent and ethics approval: Written informed consent was obtained from the patient for writing and publication of this report and may be enclosed upon request. The need for ethics approval was waived in accordance with the Umeå University policy on case reports. Research reported herein conforms to the Helsinki Declaration.
Human and animal rights: The work described has not involved experimentation on humans or animals.
Financial support: The Foundation for Medical Research in Skellefteå, Sweden.
References
- Cardoso ER, Peterson EW. Pituitary Apoplexy: A Review. Neurosurgery 1984; 14: 363-73.
- Dubuisson AS, Beckers A, Stevenaert A. Classical pituitary tumour apoplexy: Clinical features, management and outcomes in a series of 24 patients. Clinical Neurology and Neurosurgery 2007; 109: 63-70.
- Banerjee C, Snelling B, Hanft S, Komotar RJ. Bilateral cerebral infarction in the setting of pituitary apoplexy: A case presentation and literature review. Pituitary 2015; 18: 352-358.
- Elarjani T, Chen S, Cajigas I, Saway B, Sur S, et al. Pituitary Apoplexy and Cerebral Infarction: Case Report and Literature Review. World Neurosurg. 2020; 141: 73-80.
- Zhang CX, Feng F, Zhu YC, Wang RZ, Xing B. Cerebral Infarction Caused by Pituitary Apoplexy: Case Report and Review of Literature. Turkish Neurosurgery 2014; 24: 782-787.
- Bujawansa S, Thondam SK, Steele C, Cuthbertson DJ, Gilkes CE, et al. Presentation, management and outcomes in acute pituitary apoplexy: A large single-centre experience from the United Kingdom. Clinical Endocrinology 2014; 80: 419-424.
- Zou ZY, Liu CY, Sun B, Chen CM, Xiong WT, et al. Surgical treatment of pituitary apoplexy in association with hemispheric infarction. Journal of Clinical Neuroscience 2015; 22: 1550-1554.
- Sussman ES, Ho AL, Pendharkar AV, Achrol AS, Harsh GI. Pituitary Apoplexy Associated with Carotid Compression and a Large Ischemic Penumbra. World Neurosurgery 2016; 92.
- Nagure PV, Nikam VR, Garud AS. Pituitary Apoplexy Producing Internal Carotid and Basilar Artery Compression: A Rare Case Report. Asian J Neurosurg 2018; 13: 1264-1268.
- Bang OY, Saver JL, Kim SJ, Kim GM, Chung CS, et al. Collateral Flow Predicts Response to Endovascular Therapy for Acute Ischemic Stroke. Stroke. 2011; 42: 693-699.
- Liebeskind DS. Collateral circulation. Stroke. 2003; 34: 2279- 2284.
- Berkhemer OA, Jansen IGH, Beumer D, Fransen PSS, van den Berg LA, et al. Collateral Status on Baseline Computed Tomographic Angiography and Intra-Arterial Treatment Effect in Patients With Proximal Anterior Circulation Stroke. Stroke 2016; 47: 768-776.
- Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, et al. Randomized Assessment of Rapid Endovascular Treatment of Ischemic Stroke. New England Journal of Medicine 2015; 372: 1019-1030.
- Chokyu I, Tsuyuguchi N, Goto T, Chokyu K, Chokyu M, et al. Pituitary Apoplexy Causing Internal Carotid Artery Occlusion-Case Report. Neurologia Medico-Chirurgica 2011; 51: 48-51.
- Molina CA, Montaner J, Abilleira S, Ibarra B, Romero F, et al. Timing of spontaneous recanalization and risk of hemorrhagic transformation in acute cardioembolic stroke. Stroke. 2001; 32: 1079-1084.