Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
Rarely seen accelerated progression of hidradenitis suppurativa
Aquino Williams1*; Britney Clemen2; Rita Iyer1; Alexandre Shehata1; Isaac Soliman1; Ali El-Sayed1; Bijal S Mehta1
11\Department of Medicine, Hackensack Meridian Health Mountainside Medical Center, Montclair, New Jersey, 07028, USA.
2 Department of Internal Medicine, Maimonides Medical Center, Brooklyn, New York, 11219, USA.
*Corresponding Author : Aquino Williams
Department of Medicine, Hackensack Meridian Health Mountainside Medical Center, Montclair, New Jersey, 07028, USA.
Email: aquino.williams@mountainsidehosp.com
Received : Apr 09, 2021
Accepted : May 06, 2021
Published : May 11, 2021
Archived : www.jcimcr.org
Copyright : © Williams A (2021).
Citation: Williams A, Clemen B, Iyer R, Shehata A, Soliman I, et al. Rarely seen accelerated progression of hidradenitis suppurativa. J Clin Images Med Case Rep. 2021; 2(3): 1129.
Introduction
Malignant nodular hidradenoma, also known as Malignant Hidradenocarcinoma (MHA), is a rare tumor of sweat glands that accounts for less than 0.001% of all tumors [1-3,14]. Although it typically arises de-novo, MHA rarely progresses from hidradenitis suppurativa (HS), a disorder of apocrine glands characterized by chronic inflammation [5,6,9]. HS is due to recurrent follicular occlusion leading to painful debilitating cutaneous/subcutaneous abscesses requiring drainage [5,6,9]. Common sites include axillary, anogenital and inguinal regions [5,6,9]. The worldwide prevalence of HS is 1%-4% [5,6]. Incidence of all eccrine carcinomas is ~ 6% [14]. Risk-factors include family history, obesity, and smoking [5,6,9]. Severe complications associated with HS are squamous cell carcinoma and adenocarcinoma [2,6]. MHA progression is extremely aggressive with 60% cases having metastatic spread within the first 2 years of diagnosis [14].
Case presentation
20-year-old female with past medical history of left axillary HS, initially diagnosed as benign hidradenoma, presented to the emergency room for profuse bleeding from hidradenitis site. She had multiple emergency room visits and required several incision and drainage procedures over the last 2-years prior to initial presentation. She had grown accustomed to the recurrent bleeding episodes from the same location. Due to the history coupled with progression from purulent drainage to frank bleeding, additional work-up was pursued.
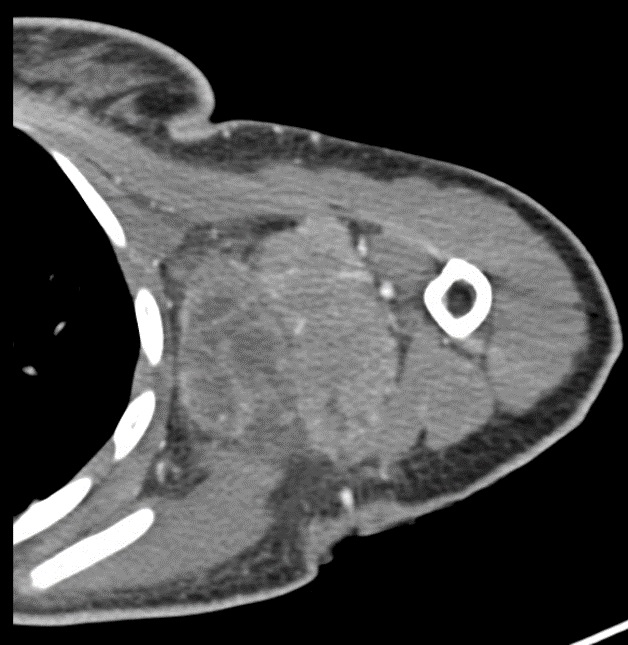
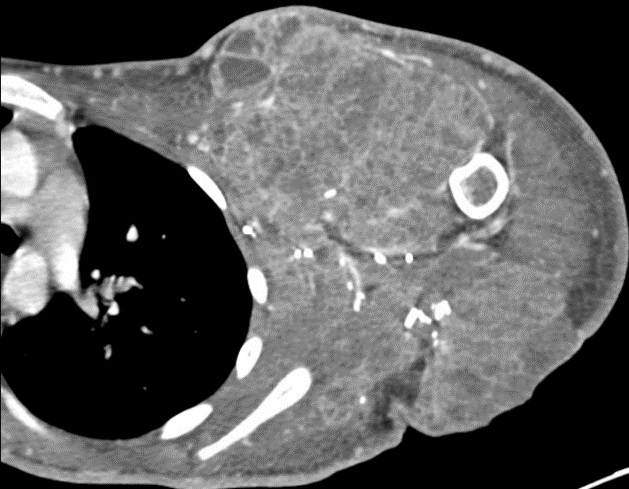
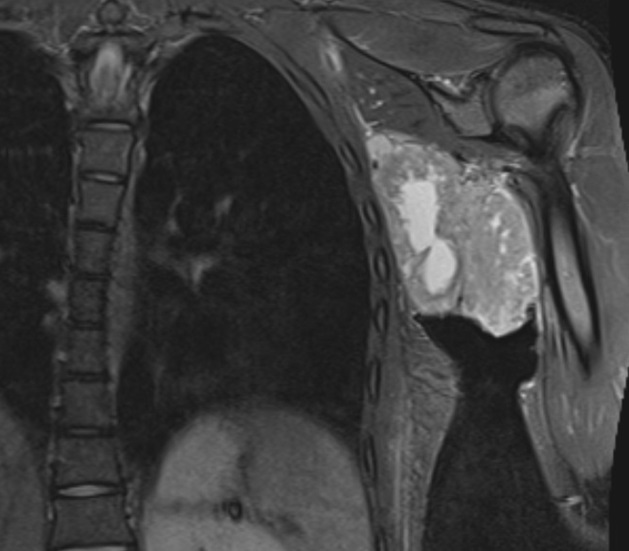
CT angiogram of the upper extremity showed a heterogeneous 8.4 X 5.7 X 11.0 cm mass in the left axilla with an area suspicious for necrosis. Concerning for malignancy (Figure 1), she was taken to the operating room for hemostasis as well as tissue biopsy. Biopsy results of the mass showed predominantly dermal proliferation of small monomorphic-appearing epithelioid cells arranged in a well-circumscribed nest with lobes and a few peripheral mitotic figures with various focal areas of necrosis. These histologic features were most consistent with the diagnosis of hidradenoma over hidradenocarcinoma. Hidradenocarcinoma was thought to be less likely due to absence of significant necrosis.
She was diagnosed with malignant hidradenoma with disease progression as well as metastatic lesions involving hepatic, adrenal, nodal, and osseous metastasis (Figure 1B). She was started on palliative radiotherapy and doxycycline. Unfortunately, she had unrelenting disease progression with bleeding complications and passed away.
Discussion
Hidradenitis suppurativa is a chronic condition characterized by recurrences that decrease in frequency over time [6,7]. A cohort study of 127 patient with hidradenitis suppurative followed for an average of 22 years showed disease improvement in 31.5%, remission in 39.4%, stable disease in 20.5%, and worsening in 8.7% [8]. Acute disease exacerbation is associated with premenstrual fares [6,7].
Hidradenitis suppurativa increases risk of developing adenocarcinoma and, more commonly squamous cell carcinoma, and typically arises from chronic lesions of 10-30 year [8,9]. Differentiation between Malignant Hidradenocarcinoma (MHA) and a benign hidradenoma is difficult; however, the distinguishing entities include greater mitotic activity, atypical mitotic figure and angiolymphatic invasion with loss of circumscription [14]. Histological characteristics describe two district cell types of MHA, darker fusiform cell with eosinophilic cytoplasm and larger cells with nuclear pleomorphism along with atypical mitotic figures [14].
Currently, there are no uniform treatment guidelines. Treatment approach is dependent upon disease severity. For example, localized tumors require a combination of surgical resection and possible external beam radiation [10,11,14]. There is a role for chemotherapy with 5-FU or capecitabine in the setting of metastatic disease [10]. Some studies have suggested using the following second line agents: bleomycin, cyclophosphamide, doxorubicin, platins and bleomycin [10,11]. Further targeted therapy includes the use of trastuzumab, PI3K/Akt/mTOR pathway inhibitors, epidermal growth factor receptor inhibitor as well as antiandrogen agents [13,14].
This novel case highlights the importance of maintaining an open mind and broad working differential as a “Simple Diagnosis” of hidradenoma proved later to be metastatic hidradenocarcinoma. It demonstrates how difficult it can be to differentiate benign hidradenoma from malignant hidradenocarcinoma. Furthermore, it stresses the importance of advanced imaging and histopathology staining as well as the use of biomarkers. The limited information about hidradenocarcinoma, coupled with the lack of treatment guidelines underscores the need for further research.
References
- Sweat gland carcinomas: A comprehensive review. Cruz DJ Semin Diagn Pathol. 1987; 4: 38-74.
- Bendary A, Tawfik W, Mahros M, Salem M. Fibrinolytic therapy in patients with ST-segment elevation myocardial infarction: Accelerated versus standard Streptokinase infusion regimen. J Cardiovasc Thorac Res. 2017; 9: 209-214.
- Eccrine adenocarcinoma. A clinicopathologic study of 35 cases. Mehregan AH, Hashimoto K, Rahbari H Arch Dermatol. 1983; 119: 104-114.
- Gouiaa N, Abbes K, Fakhfekh I, Ayadi L, Bahri I, et al. Hidradenocarcinoma arising from pre-existing hidradenoma]. Ann Dermatol Venereol. 2008; 135: 714-715.
- Skin adnexal neoplasms-part 2: An approach to tumours of cutaneous sweat glands. Obaidat NA, Alsaad KO, Ghazarian DJ Clin Pathol. 2007; 60: 145-159.
- Deckers IE, van der Zee HH, Prens EP. Epidemiology of hidradenitis suppurativa: prevalence, pathogenesis, and factors associated with the development of HS. Curr Dermatol Rep 2014; 3: 54-60.
- Danby FW, Margesson LJ. Hidradenitis suppurativa. Dermatol Clin. 2010; 28: 779-793.
- Deckers IE, van der Zee HH, Prens EP. Epidemiology of hidradenitis suppurativa: prevalence, pathogenesis, and factors associated with the development of HS. Curr Dermatol Rep. 2014; 3: 54-60.
- Kromann CB, Deckers IE, Esmann S, Boer J, Prens EP, Jemec GB. Risk factors, clinical course and long-term prognosis in hidradenitis suppurativa: A cross-sectional study. Br J Dermatol. 2014; 171: 819-824.
- Zouboulis CC, Desai N, Emtestam L, et al. European S1 guideline for the treatment of hidradenitis suppurativa/acne inversa. J Eur Acad Dermatol Venereol. 2015; 29: 619-644.
- Jouary T, Kaiafa A, Lipinski P, Vergier B, Lepreux S, et al. Metastatic hidradenocarcinoma: Efficacy of capecitabine. Arch Dermatol. 2006; 142: 1366-1367.
- Amel T, Olfa G, Faten H, Makrem H, Slim BA, et al. Metastatic hidradenocarcinoma: Surgery and chemotherapy. Am J Med Sci. 2009; 1: 372-374.
- Guillot B. From unusual cutaneous malignancies: Cutaneous adnexal tumors. In: Belkacemi Y, Mirimanoff R, Ozsahin M, editors. Management of rare adult tumors. Paris: Springer- Verlag France. 2009; 471–477.
- Kyrgias G, et al. Hidradenocarcinoma of the temporal area successfully treated with concomitant electrochemotherapy and radiotherapy. Head Neck Oncol. 2013; 5: 14.
- Sinhasan S, Harthimath B, Sylvia M, Bhat, R. Metastatic malignant nodular hidradenoma: A rare case report with review of literature. Clinical Cancer Investigation Journal. 2015; 4: 651.