Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
A rare etiology of posterolateral pain subsequent to a total knee arthroplasty
Olden Theresa Rebecca 1 *; Vallotton, Jacques 2
1 Orthopedic Surgery Residency, Medicol - Ouchy Orthopedic Center, Av. D’Ouchy 41, CH - 1006 Lausanne, Switzerland.
2 Specialist in Orthopedic Surgery, Sports Medicine, Medicol - Centre or-thopédique d’Ouchy, Av. d’Ouchy 41, CH - 1006 Lausanne, Switzerland.
*Corresponding Author: Olden Theresa Rebecca
Orthopedic Surgery Residency, Medicol - Ouchy
Orthopedic Center, Av. d’Ouchy 41, CH - 1006
Lausanne, Switzerland.
Email: theresa.olden@icloud.com
Received : Apr 19, 2021
Accepted : May 19, 2021
Published : May 21, 2021
Archived : www.jcimcr.org
Copyright : © Olden TR (2021).
Abstract
This case report illustrates a very rare problematic after Total Knee Arthro-plasty (TKA), yet that you have to think of if posterolateral pain appears. The postoperative outcome of our patient was initially very good, but pain appeared after 6 weeks, in an atypical mode, that couldn’t be attributed to the most common differential diagnosis. The characteristics of the symptoms directed us to a mechanical cause and the solution finally came up by means of a radiography: the images showed an impingement between one of the tibial tuberosity fixation screw’s head and the fibular neck. What couldn’t be seen on the primary images was an irritating callus, that was detected at 3 months postoperatively. The pain disappeared after surgical removal of the screw.
Keywords: Total knee arthroplasty; Posterolateral knee pain; Pain after total knee ar-throplasty; Tibial screw impingement.
Abbreviations: TKA: Total Knee Arthroplasty; TTT: Tibial Tuberosity Transposition; HO: Heterotopic Ossifications.
Citation: Older TR, Vallotton J. A rare etiology of posterolateral pain subsequent to a total knee arthroplasty. J Clin Images Med Case Rep. 2021; 2(3): 1159.
Introduction
Multiple studies and publications [1-7] were carried out in relation to the etiology of postoperative pain after TKA. The most frequently cited etiologies, besides infection, concerned mostly the implants: Loosening [2,6], malpositioning [1,3,7], or malalignment [4,5]. More specifically, in case of posterolateral pain, the most common determined etiology is the mispositioning of the tibial component [3,7]. The posterior overhang can cause an impingement with soft tissue, in particular the tendon of the popliteus muscle. The impingement can concern the metallic component or the polyethylene, which is more difficult to detect because radiologically the implants seem to have the right dimensions [1]. The solution is generally operative, reaching from arthroscopy to the revision of TKA. The case that we present here is far from ordinary and illustrates a very different problematic, that we have to think of before starting a hazardous revision.
Clinical case
The patient is a 58-year-old female, suffering from fibromyalgia and obesity. She underwent a subtotal medial meniscectomy on her right knee in 1982, at the age of 20, and she was operated of a left TKA in 2013, with a good outcome.
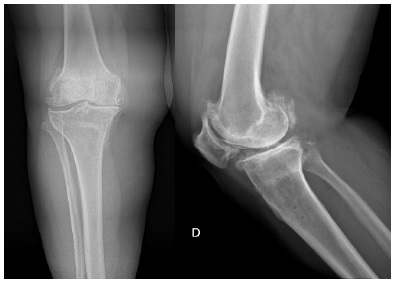
In February 2020, we proceed to a right TKA, with SCORE® implants (AMPLITUDE SUISSE SA, Geneva, Switzerland), associated with a Tibial Tuberosity Transposition (TTT), because of a low sitting patella, and a lateral retinaculum plasty. The preoperative radiographies are illustrated here below and show the low position of the patella and the severe osteoarthritis (Figure 1).
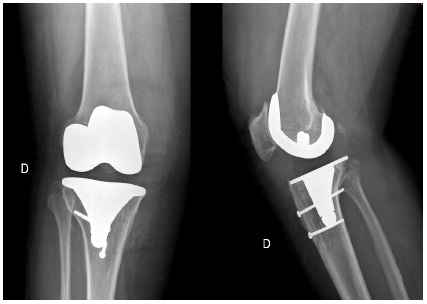
The postoperative radiographies are judged satisfying (Figure 2) and the follow-up of this operation was initially very favorable. The knee is evolving less well during the following period and, when the patient came for her 3 months radiographic and clinical control, she complains about posterolateral pain, that appeared recently and is particularly present during walking.
The pain, when it is vivid, forces her to stop after having walked about 100 meters on a flat ground. It disappears spontaneously while resting and can reappear if she resumes activity. There are no inflammatory signs and no pain during night. The physical exam shows a contracture of the popliteus muscle, a dysfunctional proximal tibiofibular and subtalar joint on the right side. Moreover, the proximal tibiofibular joint is very painful at mobilization. The knee itself is not swollen, with no effusion and free in movements with 130° of flexion and a full extension.
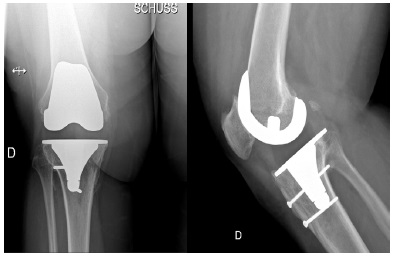
The radiologic assessment shows a good evolution of the implants at 3 months postoperatively. Nevertheless, on the profile film, we can observe a newly formed little calcification on the extremity of one of the fixation screws of the tibial tuberosity. The screw is discretely overlapping on the posterior border, just above the proximal tibiofibular joint (Figure 3).
The case history, physical exam and the Radiography raised the suspicion of a bony impingement at the head of one of the two antero-posterior screws and the conservative treatment wasn’t efficient. That is why we decided to remove the screw surgically. The symptomatology disappeared after the intervention, confirming the etiology of the pain.
Discussion
The impingement caused by the head of a screw as the origin of invalidating posterolateral pain is an extremely rare etiology of pain after TKA and no case has been described until this day in literature, as soon as we know. This complication results from a very lateral positioning of the screw head and it’s posterior overhang. This is very common when the screwing is for compression, because the screw cannot hold on one cortical bone. That’s why we have to be sure of a sufficient holding, by making some turns exceed the posterior cortical bone. The very lateral position of the screw head is related to the type of implant and particularly to the width of the tibial peg. The implant type that we used here (mobile bearing) can predispose to this kind of complication.
This problem could be avoided by a different mode of fixation of the tibial osteotomy segment (cerclage wire fixation), but the screw fixation is providing a better hold and therefore represents a supplementary security to obtain the consolidation of the tibial tubercule osteotomy. This is why we use this type of fixation almost systematically in this situation. The posterolateral pain after TKA is not that rare and its differential diagnosis includes principally the painful bony impingements related to the implants or impingements of other origins as Heterotopic Ossifications (HO), as seen here with an irritating callus. The HO are induced by bone trauma, or they are caused by an inflammatory or neurologic process [8]. The etiologies are summarized in the chart below, that regroups the cases of posttraumatic or inflammatory origin, related to a systemic pathology, an infection or a neurologic injury [9] (Table 1).
Table 1: Summary of the two different forms of heterotopic ossification, trauma-induced of genetic [9].
|
Trauma-induced |
Genetic |
Injury Type |
Deep tissue burns |
Fibrodysplasia ossificans progressive (FOP) |
Inductive stimuli |
Systemic inflammation |
Inflammatory flares |
Affected tissues |
Perimysium |
|
Bone type |
Enchondral |
|
Diagnostic modality |
Radiography, CT, Spect-CT, Ultrasound |
|
Treatment modality |
Surgical Excision |
|
If we consider posterolateral pain of mechanical origin after TKA, we can very often observe a mispositioning of the implants or an inappropriate size of the tibial baseplate or its polyethylene. Michel Bonnin provided a good explication in his article that references the implant type, anatomic or not, and their size [1]. The frequency of this type of complication is related to the fact that the surgeon tends to slightly oversize the tibial component in order to avoid a subsidence, whilst assuring a good support of the baseplate on the cortical bone. Yet, the tibia is naturally convex in the sagittal plane, but the implant is flat (rectangular). Even if the metallic baseplate of the tibial plateau is well-sized, the thickness of the polyethylene insert, that has the same size in a fixed bearing, creates a discrete hangover in relation to the anatomical position. This posterior hangover can cause a painful impingement with the popliteus tendon. It’s thereby important to make sure to prevent this impingement by choosing the appropriate size of the tibial baseplate. This problem appears essentially in the case of fixed-bearing prothesis and this diagnosis hasn’t been retained for our case because it’s a mobile-bearing knee prothesis.
Conclusion
This clinical case demonstrates that even if there is a wide range of differential diagnosis for a posterolateral pain of the knee (Table 2), there are rare etiologies that aren’t described yet. This case highlights the importance to analyze and correlate in the symptoms, the clinical picture and the radiologic assessment in an exhaustive way. After having excluded the most current diagnosis, one cannot rely on a diagnosis called “idiopathic”. It’s important to consider the knee in its union of the patellofemoral joint, the femorotibial joint and also the proximal tibiofibular joint, that is the most concerned here. To study the movements and examine the over-and underlying joints can accessorily guide us towards the right diagnosis.
Table 2: Differential diagnosis of posterolateral pain of the knee without a prosthesis [10].
Structure |
Etiology |
Characteristics |
Clinical Diagnosis |
Postero-lateral corner |
Traumatic injury |
Varus-Flexion-Internal rotation stress |
1. Dial test. |
Popliteus tendon |
Tendino-pathy |
Runner’s knee |
Painful palpation of its insertion on the outer side of the lateral condyle of the femur |
Biceps femoris |
Tendino-pathy |
Mostly sportive patients |
Flexion-external rotation of the knee against resistance while the foot is positioned in internal rotation |
Fabella |
Arthrosis |
Diagnosis of exclusion |
Painful palpation of the posterior side of the external femoral condyle |
Iliotibial tract |
Tendino-pathy |
Runner’s knee, pain is present especially when running downwards |
Elective pain on the external epicondyle |
Practical implications
- An impingement at the screw head occasioning invalidating posterolateral pain constitutes an extremely rare etiology of pain post-TKA.
- The posterolateral knee pain after TKA isn’t that uncommon and their differential diagnosis includes essentially painful impingements related to the implants and impingements of other origin, as heterotopic ossifications (OH), as in this case with an irritating callus.
- For fixed bearing protheses, don’t oversize the tibial implant in order to avoid posterior impingements .
- Consider the mechanical interaction of joints to look for the symptom’s origin.
References
- Bonnin MP, de Kok A, Verstraete M, Van Hoof T, Van Der Straten C et al. Popliteus impingement after TKA may occur with wellsized prosthe-ses. Knee Surg Sports Traumatol Arthrosc. 2017; 25: 1720-1730. Erratum in: Knee Surg Sports Traumatol Arthrosc. 2017; 25: 3654.
- Lim HA, Song EK, Seon JK, Park KS, Shin YJ, et al. Causes of Aseptic Persistent Pain after Total Knee Arthroplasty. Clin Orthop Surg. 2017; 9: 50-56.
- Momoli A, Giarretta S, Modena M, Micheloni GM. The painful knee after total knee arthroplasty: Evaluation and management. Acta Biomed. 2017; 88: 60-67.
- Planckaert C, Larose G, Ranger P, Lacelle M, Fuentes A, et al. Total knee arthroplasty with unexplained pain: New insights from kinematics. Arch Orthop Trauma Surg. 2018; 138: 553-561.
- Park CN, White PB, Meftah M, Ranawat AS, Ranawat CS. Diagnostic Algorithm for Residual Pain After Total Knee Arthroplasty. Orthopedics. 2016; 39: e246-e252.
- Bonnin M, Amendola A, Bellemans J, MacDonald S, Ménétrey J. The painful total knee arthroplasty. 2012; 969-981.
- Simsek ME, Akkaya M, Gursoy S, et al. Posterolateral overhang af-fects patient quality of life after total knee arthroplasty. Arch Orthop Trau-ma Surg. 2018; 138: 409-418.
- Edwards DS, Clasper JC. Heterotopic ossification: A systematic re-view. J R Army Med Corps. 2015; 161: 315-321.
- Dey D, Wheatley BM, Cholok D, et al. The traumatic bone: trauma-induced heterotopic ossification. Transl Res. 2017; 186: 95- 111.
- https://www.orthobullets.com/knee-and-sports/3012/posterolateral-corner-injury.