Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
Complicated intra-abdominal focal fat infarction: Emphasis on falciform ligament infarction with abscess formation: A case series
Berton Monteiro1,2; Saurabh Joshi3,; Sunita Gopalan3; Ravikumar Hanumaiah1,4*
1 Columbia Asia Hospital, Whitefield, Bangalore, India.
2 Father Muller Medical College, Mangalore, India.
3 Columbia Asia Hospital, Yeshwanthpur, Bangalore, India.
4 SUNY Upstate Medical University, Syracuse, New York, USA.
*Corresponding Author : Ravikumar Hanumaiah
Columbia Asia Hospital, Whitefield, Bangalore, India
and SUNY Upstate Medical University, Syracuse, New
York, USA.
Email: h.ravi.k@gmail.com
Received : Apr 26, 2021
Accepted : Jun 01, 2021
Published : Jun 04, 2021
Archived : www.jcimcr.org
Copyright : © Hanumaiah R (2021).
Abstract
The term “Intra-Abdominal Focal Fat Infarction” (IFFI) encompasses a range of conditions where infarction of fatty tissue is the underlying pathological process, including Epiploic appendagitis, omental infarction, fat necrosis related to trauma or pancreatitis as well as rarer entities such as falciform ligament infarction. Uncomplicated IFFI is usually self-limiting and managed conservatively with oral antiinflammatory therapy. Rarely complications such as liquefaction and secondary abscess formation may arise with associated deterioration in symptoms and signs prompting a change in management including Laparoscopic resection or Percutaneous drainage. We present 3 cases of complicated IFFI with emphasis on the rarer Falciform ligament infarction with abscess formation.
Keywords: Falciform ligament; Omentum; Infarction; Intra-abdominal focal fat infarction; Abscess.
Citation: Monteiro B, Joshi S, Gopalan S, Hanumaiah R. Complicated intra-abdominal focal fat infarction: Emphasis on falciform ligament infarction with abscess formation: A case series. J Clin Images Med Case Rep. 2021; 2(3): 1183.
Introduction
Intraabdominal fat is a metabolically active tissue that may undergo necrosis through a few mechanisms including torsion of an epiploic appendage, infarction of the greater omentum, fat necrosis related to trauma/pancreatitis or falciform ligament infarction. It may cause abdominal pain, mimic findings of acute abdomen, or be asymptomatic [1]. The falciform ligament can be secondarily affected by surrounding inflammation, however primary pathologies are rare [2]. Primary infarction of the ligament is rare with very few cases reported in the literature.
Case 1
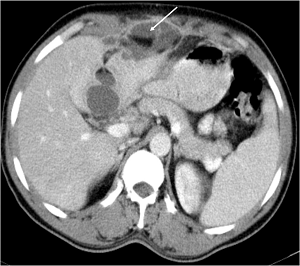
A 35-year-old gentleman presented with pain and tenderness in the right hypochondriac region accompanied by fever for 10 days. Lab Investigations demonstrated increased WBC count. Contrast enhanced CT of the abdomen demonstrated a well-defined lesion with both fat and fluid attenuation within and peripheral enhancement with adjacent fat stranding along the falciform ligament, anterior to the liver surface and in the ligamentum teres of the liver (Figure 1). The Gallbladder and the biliary system were normal. Findings were in keeping with infarction of the falciform ligament with secondary abscess formation.
Companion case 1
A 39-year-old gentleman with history of abdominal hernia repair 4 months back, presented with persistent pain in right lumbar region with a palpable mass. There was no history of fever with the WBC counts in the normal range. CT abdomen without contrast demonstrated a large well-defined lesion with fat fluid level within involving the omentum in the right lumbar region (Figure 2). A well-formed thick wall in the periphery with adjacent significant fat stranding was also noted. A diagnosis of complicated omental infarction with secondary liquefaction was made. Possibility of superimposed infection could not be determined since the patient refused aspiration of the lesion and was lost to follow up. However, abscess formation was thought to be less likely in view of normal WBC counts.
Case 2
Companion case 2
A 55-year-old gentleman with history of gastric bypass surgery one month back presented with pain and tenderness in right lumbar region accompanied by high grade fever. Lab investigations demonstrated increased WBC counts. CT Abdomen without contrast demonstrated a large well-defined lesion with fat fluid level and pockets of air within involving the omentum in the right lumbar region (Figure 3). A well-formed thick wall at the periphery with adjacent significant fat stranding was also noted. Findings were in keeping with omental infarction with secondary abscess formation. Surgical resection of the lesion confirmed the diagnosis.
Discussion
The Falciform ligament is a structure arising at the umbilicus and continues onto the anterior aspect of liver in continuity with the umbilical fissure. It is a double fold of peritoneum that anatomically divides the liver into the right and left lobes and extends from the superior edge of the liver to the inferior border of the diaphragm. The falciform ligament contains the ligamentum teres within the lower edge, paraumbilical veins, and variable amount of extraperitoneal fat. The ligamentum teres is a remnant of the obliterated umbilical vein [3].
The arterial supply of the falciform ligament originates from a thin branch of the right hepatic artery, which is anastomosed to the superficial inferior epigastric artery. Venous drainage flows directly into the paraumbilical vein and portal vein. Falciform ligament necrosis may likely develop if the embolization of this artery or venous thrombosis occurs. Necrosis due to an occlusion of arterial supply is a rare primary falciform ligament disease [2]. Review of the literature revealed limited data on falciform ligament necrosis with no case of secondary abscess formation reported.
On ultrasound, an infarcted fatty appendage of the falciform ligament appears as a hyperechoic, noncompressible, slightly heterogenous mass at the site of maximal abdominal tenderness. On CT, an infarcted fatty appendage of the falciform ligament appears as an area with increased fat density, associated with surrounding inflammatory changes in the adjacent fat planes [3]. These findings represent uncomplicated fat necrosis which can be managed conservatively. However, rarely fat necrosis can undergo complications such as liquefaction or secondary abscess formation as demonstrated in our case series which necessitates a change in the management in the form of percutaneous drainage or laparoscopic resection [4]. The presence of thick enhancing walls, fluid levels and air within the lesion heralds the formation of an abscess.
Omental infarcts, a form of IFFI, is much more common than infarction of falciform ligament.
Primary omental infarction is often a hemorrhagic infarction resulting from vascular compromise related to the tenuous blood supply to the right edge of the omentum or to kinking of veins, usually those on the right side, deep within the anterior pelvis at the inferior extent of omentum. It can occur in hypercoagulable states, congestive heart failure, vasculitis and in marathon runners.
Secondary omental infarction may occur after a traumatic injury or due to surgical trauma as demonstrated by Case 2 and 3 in our series. Often, the site of secondary infarction is near the surgical site rather than in the right lower quadrant, the typical location of primary omental infarction. Omental infarction demonstrates a variety of imaging appearances at CT. Classically, it appears as a large (>5 cm) encapsulated, fat density mass, with soft tissue stranding adjacent to the ascending colon. Early or mild infarction may manifest as mild haziness in the fat anterior to the colon [1]. Uncomplicated forms are managed conservatively. Rarely, an omental infarct may become infected and simulate a mass lesion or evolve into an abscess, necessitating a change in management as depicted in our case series.
References
- Kamaya A, Federle MP, Desser TS. Imaging Manifestations of Abdominal Fat Necrosis and Its Mimics. RadioGraphics. 2011; 31:2021–2034.
- Ozkecec ZT, Ozsoy M, Celep BJ, Bal A, Polat C. A Rare Cause of Acute Abdomen: An Isolated Falciform Ligament Necrosis. Case Reports in Emergency Medicine. 2014; 57075.
- Maccallum C, Eaton S, Chubb D, Franzi S. Torsion of Fatty Appendage of Falciform Ligament: Acute Abdomen in a Child. Case Reports in Radiology. 2015; 293491.
- Chauhan V, Stephenson JA, Shah V. Intra-abdominal focal fat infarction of the omentum: Diagnosis and percutaneous management. BJR Case Rep. 2015; 1: 20150134.