Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
Refractory cluster-tic syndrome: The Hickam’s dictum
Membrilla JA*; Díaz de Terán J
Neurology Department, La Paz University Hospital, Madrid, Spain.
*Corresponding Author: Javier A Membrilla
Neurology Department, La Paz University Hospital,
Madrid, Paseo de la Castellana 261, 28046 Madrid,
Spain.
Email: membrillaja@gmail.com
Received : Jun 25, 2021
Accepted : Aug 06, 2021
Published : Aug 12, 2021
Archived : www.jcimcr.org
Copyright : © Membrilla JA (2021).
Abstract
A 50-year-old man debuted with right trigeminal neuralgia. In the following years, it became refractory to medical treatment and ipsilateral cluster headache appeared. He was diagnosed with cluster-tic syndrome. A brain magnetic resonance with high-spatialresolution 3D T2 sequences (FIESTA) excluded the existence of neurovascular conflict, but a surgical exploration was indicated due to its torpid evolution. A venous contact with the right trigeminal nerve was confirmed in the surgery and microvascular decompression was performed. The patient’s evolution was favorable, improving the trigeminal neuralgia as well as the cluster headache.
Keywords: Trigeminal neuralgia; cluster headache; cluster-tic syndrome; microvascular decompression.
Citation: Membrilla JA, Díaz de Terán J. Refractory cluster-tic syndrome: The Hickam’s dictum . J Clin Images Med Case Rep. 2021; 2(4): 1262.
Case presentation
A 50-year-old man started with paroxysmic episodes of severe facial pain, starting in the left hemipalate and irradiating to the infraorbital region with electric-like quality, lasting for a few seconds. They were daily, accounting for 5 to 10 episodes per day without time preference. The paroxysms were absent in the sleep. The patient reported talking and chewing as triggers. The pain was not associated with conjunctival injection, tearing or other autonomic symptoms. He consulted with an odontologist and a maxillofacial surgeon, who discarded an odontogenic origin of the pain. His general practitioner recommended initiation of gabapentin.
He was referred to the Pain Management Unit one year after the beginning of the symptoms. After an interictal neurological exam with normal results he was diagnosed with left trigeminal neuralgia of the second branch. He apported a brain Magnetic Resonance Imaging (MRI) without a specific sequence of thin slices for posterior fossa examination, with normal results. The gabapentin trial at 900 mg/day was successful in decreasing the frequency of the paroxysms, but the patient still reported pain with triggers. For this reason, carbamazepine 600 mg/day was initiated.
In following year, the paroxysms while speaking and eating still limited the patient’s quality of life. Triggers did not disappear completely even after reaching a carbamazepine dose of 2400 mg/day. Besides, this dose was related with dizziness as adverse event. Because of this, the physicians in the Pain Management Unit performed three sessions of sphenopalatine ganglion block ablation, without notorious response.
Two years after, he began to suffer another kind of facial pain in right periocular region, of throbbing quality and severe intensity, associated with ipsilateral ptosis, conjunctival injection, rhinorrhea and an important feeling of restlessness. These episodes lasted from 45 minutes to 1 hour, disrupted sleep and presented from 1 to 3 times a day. See Figure 1 for a picture of the patient while one of these episodes.
He was referred to the Headache Clinic and was diagnosed (in addition to the previously described trigeminal neuralgia) with episodic Cluster headache by a neurologist specialized in headache disorders, based on the International Classification of Headache Disorders (ICHD-3) diagnostic criteria of this disorder. Based on the history of trigeminal neuralgia, whose episodes continued to appear with the same triggers, this case corresponds with the so-called “cluster tic syndrome”. We start ed verapamil 240 mg/day for cluster headache management, lacosamide 200 mg/day was added for trigeminal neuralgia and carbamazepine was replaced for eslicarbazepine acetate 1200 mg/day. For the following 3 years, the patient remained symptomatic and the cluster headache bouts became chronic despite the introduction of topiramate 100 mg/day and greater occipital nerves anesthetic blocks. As the administration of botulinum toxin has proven to be a safe and effective therapeutic strategy in patients with drug- refractory idiopathic trigeminal neuralgia and could also help patients with cluster headache [1], 50 international units of onabotulinum toxin A were administered in the first and second branch territory of the trigeminal nerve, without a consistent response.
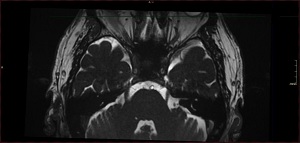
Following the recommendations of international guidelines [2], a new brain MRI with high-spatial- resolution 3D T2 sequences (FIESTA) was performed, without being able to confirm a compromise between the right trigeminal nerve and vascular structures (see Figure 2). Because of this refractoriness to medical treatment, the patient underwent a surgical posterior fossa exploration. In the surgery, neurovascular compromise between the right trigeminal nerve root and a vein was confirmed and Janetta decompression technique was performed (see Figures 3 & 4). The intervention resulted with the adverse event of sensorineural deafness, but the evolution of the pain of the patient was favorable, with his cluster headache manifesting becoming episodic and the trigeminal neuralgia absent under treatment with eslicarbazepine acetate 400 mg/24h.
Discussion
Cluster-tic syndrome is a term often used to describe the occurrence of cluster headache and ipsilateral trigeminal neuralgia in the same patient. This corresponds with a rare clinical scenario, with only around 50 cases reported [3]. This disorder is not recognized by the International Headache Society as a separate clinical entity, since the ICHD-3 specifies that these patients should be diagnosed as both cluster headache (code 3.1) and trigeminal neuralgia (code 13.1.1). Both diagnoses should be managed in order to improve the patient’s condition [4]. Table 1 displays their diagnostic criteria.
Table 1: International Classification of Headache Disorders third edition (ICHD-3) diagnostic criteria for cluster headache and trigeminal neuralgia [4].
Cluster headache |
Trigeminal neuralgia |
|
Recurrent paroxysms of unilateral facial pain in the distribution(s) of one or more divisions of the trigeminal nerve, with no radiation beyond, and fulfilling criteria B and C.
|
The underlying mechanisms of the cluster-tic syndrome are unknown. Some authors defend that a shared pathophysiological mechanism may not be plausible and the association of cluster headache and trigeminal neuralgia could be comorbidity. Oher authors hypothesize that the trigemino-cervical complex and its connection with the hypothalamus may play a role [3]. In this case, the overlapping syndromes and the significant clinical improvement after surgical treatment could point to a shared pathogenic mechanism. In other case reports of cluster-tic syndrome patients treated with microvascular decompression surgery, an improvement of both trigeminal neuralgia and cluster headache was also reported [5-7].
Surgical microvascular decompression for cluster-tic syndrome management has been reported before [5]. In that case, venous compression of the trigeminal nerve could be confirmed by MRI. Our case is, to the best of our knowledge, the first patient with cluster-tic syndrome to underwent an exploratory posterior fossa surgery that could confirm the neurovascular conflict.
A retrospective analysis of trigeminal neuralgia patients studied the predictability of vascular conflict by MRI with a thinsliced posterior fossa study protocol. It resulted in a sensitivity of 87%, a specificity of 50%, a positive predictive value of 95% and a negative predictive value of 27%. Specifically, MRI predicted absence of neurovascular contact in 11 patients, while surgery confirmed it in 8 patients (arterial contact in 6 patients and venous contact in 2) [8]. Therefore, even when the advance imaging techniques show no contact between the trigeminal nerve and a vascular structure, surgical exploration could be an option for patients with trigeminal neuralgia. Even though it has not been studied specifically, cluster-tic syndrome patients could benefit from this as well.
The effectivity of the microvascular decompression in classical trigeminal neuralgia was explored in a meta-analysis of 3879 patients from 46 observational studies, with 76.0% achieving pain freedom after surgery. Arterial compression has been suggested as a predictor of good outcome [9]. Classical trigeminal neuralgia is most likely to be caused by an arterial structure contacting the trigeminal nerve after it emerges from the pons. In a retrospective series of 22 patient with trigeminal neuralgia in which surgical microvascular decompression vas performed, venous neurovascular conflict was less common than arterial (15.3% vs 84.7%). The outcome of these two groups was compared, with a higher rate of delayed cure in the cases of decompress venous neurovascular conflict, but still as effective in the long-term as when arterial conflict was the case [10].
Acknowledgements: To our Neurology Department colleagues.
Contributorship: Conceptualization: Javier A. Membrilla. Writing - original draft preparation: Javier A. Membrilla. Writing - review and editing: Javier Díaz de Terán. All authors have read and agreed to the published version of the manuscript.
Ethical approval information: Approved by local ethics committee (CEIm: PI-3387). Written informed consent was obtained.
Key points
• Cluster-tic syndrome is an uncommon situation in which trigeminal neuralgia and cluster headaches occurs in the same patient. Both diseases need to receive their respective treatments.
• Even when brain MRI with High-spatial-resolution 3D T2 sequences fails to show a neurovascular conflict in trigeminal neuralgia patient, this can be confirmed by surgical exploration in some well selected patients.
• Cluster-tic syndrome patients in which neurovascular conflict is present, could improve trigeminal neuralgia and cluster headache after microvascular decompression. This fact could point to a common pathogenic origin.
References
- Freund B, Kotchetkov I. Rao A. The Efficacy of Botulinum Toxin in Cluster Headache: A Systematic Review. J. Oral Facial Pain Headache. 2020; 34: 129–134.
- Bendtsen L. et al. European Academy of Neurology guideline on trigeminal neuralgia. Eur. J. Neurol. 2019; 26: 831–849.
- Wöber C. Tics in TACs: A Step into an Avalanche? Systematic Literature Review and Conclusions. Headache. 2017; 57: 1635– 1647.
- Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018; 38: 1–211.
- de Coo I, van Dijk JMC, Metzemaekers JDM, Haan JA Case Report About Cluster-Tic Syndrome Due to Venous Compression of the Trigeminal Nerve. Headache. 2017; 57: 654–657.
- Alberca R, Ochoa JJ. Cluster tic syndrome. Neurology. 1994; 44: 996–996.
- Solomon S, Apfelbaum RI, Guglielmo KM. The Cluster-Tic Syndrome and Its Surgical Therapy. Cephalalgia. 1985; 5: 83–89.
- Hitchon PW. et al. Predictability of vascular conflict by MRI in trigeminal neuralgia. Clin. Neurol. Neurosurg. 2019; 182: 171–176.
- Holste K, Chan AY, Rolston JD, Englot DJ. Pain Outcomes Following Microvascular Decompression for Drug-Resistant Trigeminal Neuralgia: A Systematic Review and Meta-Analysis. Neurosurgery. 2020; 86: 182–190.
- Wang J, Niu H, Zhao K, Shu K. Lei T. Comparative Analysis of Trigeminal Neuralgia Caused by Sole Arterial and Venous Compression : Clinical Features and Surgical Outcomes From 222 Cases. 2021; 12: 1–8.