Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
Skin-to-spine distance as a risk factor for surgical site infection in pediatric scoliosis surgery
Maxwell Marshall; Samuel Abumoussa; Elizabeth Durante; James Mooney; Matthew Dow; William Barfield; Robert Murphy*
Department of Orthopaedics and Physical Medicine, Medical University of South Carolina, Charleston, SC 29425.
*Corresponding Author: Robert F Murphy
Department of Orthopaedics and Physical Medicine,
Medical University of South Carolina, Charleston, SC
29425.
Email: murphyr@musc.edu
Received : Jul 08, 2021
Accepted : Aug 09, 2021
Published : Aug 12, 2021
Archived : www.jcimcr.org
Copyright : © Murphy RF (2021).
Abstract
Introduction: Surgical Site Infection (SSI) is a rare but serious complication following Posterior Spinal Fusion (PSF) for pediatric scoliosis. Several studies have identified patient risk factors for SSI following PSF, including high Body Mass Index (BMI). The purpose of this study was to determine whether Radiographic Skin-to-spine Distance (RSD) can be used as a surrogate for BMI when evaluating the pediatric patient’s risk of developing a SSI after PSF.
Methods: This study was performed retrospectively and included patients ages 0-18 who underwent PSF for scoliosis over a four-year period. RSD, defined as the distance from the L5 spinous process to the skin, was measured using preoperative lateral radiographs.
Results: Of the 176 included patients, we identified eight (4.5%) who suffered from surgical site infection following PSF. Logistic regression analysis revealed no statistically significant predictors for SSI. However, there was a strong, statistically significant linear regression prediction between RSD and BMI (r = 0.71, p=0.001).
Discussion: RSD was not shown to be predictive of SSI in this patient cohort. However, the strong correlation found between RSD and BMI suggests that when assessing risk of SSI, RSD may be useful as a substitute for BMI when BMI cannot be easily ascertained.
Citation: Marshall M, Abumoussa S, Durante E, Mooney J, Murphy R, et al. Skin-to-spine distance as a risk factor for surgical site infection in pediatric scoliosis surgery. J Clin Images Med Case Rep. 2021; 2(4): 1264.
Introduction
Scoliosis is the most common spinal deformity seen in children, with a prevalence estimated from 1-3% [1,2]. For progressive curves with substantial deformity, the most common corrective technique used to treat pediatric scoliosis is Posterior Spinal Fusion (PSF). Surgical Site Infection (SSI) is a rare, but serious complication following pediatric PSF for scoliosis, with reported prevalence rates varying widely depending on the specific patient diagnosis. In their review of the relevant literature, Li, et al. found that the reported incidence of SSI following surgery for adolescent idiopathic scoliosis ranged from 0.5 to 6.7%, whereas the incidence following surgery for neuromuscular scoliosis ranged from 4.3 to 14.3% [3].
A number of studies have identified various patient risk factors for developing SSI after PSF, with a higher Body Mass Index (BMI) being one of the most commonly cited [4,5]. However, the difficulty of obtaining reliable height and body mass measurements for some patients, including many patients with neuromuscular scoliosis, presents a limitation of using BMI to assess the risk of developing a SSI. The identification of consistently available, measurable patient variables that can predict the risk of SSI could improve the orthopaedic surgeon’s ability to mitigate this risk. One tool routinely used in the preoperative assessment of scoliotic deformities is the plain radiograph.
The lateral radiograph not only allows for the assessment of spinal deformity, but soft tissue shadowing also allows for the assessment of the thickness of the soft tissue envelope from the skin to the spinal structures. The purpose of this study was to determine whether Radiographic skin-to-Spine Distance (RSD), measured as the distance from the L5 spinous process to the skin, can be used as a proxy for body habitus in pediatric patients when evaluating the risk of developing a SSI after PSF. Our hypothesis was that RSD would correlate positively with incidence of SSI.
Methods
Following institutional review board approval, a retrospective study was performed that included all patients ages 0-18 who underwent PSF for all types of scoliosis between January 2015-December 31, 2018 with a one year minimum follow up. Patients were identified by CPT codes for spinal fusion involving more than six vertebral body segments (22802, 22804). Demographic data was collected including age, gender, race, height, and body mass.
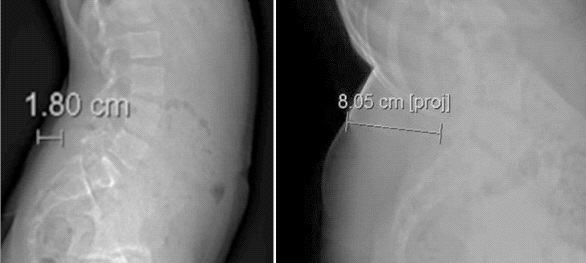
Immediate preoperative radiographs, including upright Postero-Anterior (PA) and lateral views, were used to measure radiographic markings. RSD was defined as the perpendicular distance from the L5 spinous process to the skin on lateral plain radiographs that were closest to surgery date. Each measurement was performed three times by one of two investigators and averaged for each patient (Figure 1).
All patients were queried for post-operative complications including SSI, defined as wound dehiscence, seroma formation, or return to the OR for irrigation and debridement and/or removal of hardware. Univariate descriptive statistics, Welch’s t-test, linear regression and logistic regressions were used to assess the relationship between RSD and SSI. Data analysis was conducted with IBM SPSS Statistics for Windows. V 27.
Results
During the five-year study period, we identified 202 total patients aged 0-18 years who underwent posterior spinal fusion. After excluding patients who did not have at least one year of follow-up or who had undergone prior spine surgery, 176 patients met the criteria for inclusion. One hundred fourteen (64.8%) patients had a diagnosis of idiopathic scoliosis, while 38 (21.6%) had neuromuscular diagnoses. The remaining 24 (13.6%) patients had either congenital or other spinal diagnoses. One hundred sixteen (65.9%) patients were female, 85 (48.3%) were white/non-Hispanic, 63 (35.8%) were black, 21 (11.9%) were of unknown race, six (3.4%) were Hispanic/Latino, and one (0.6%) was Asian. Further demographic analysis revealed a mean patient age of 13.26 ± 3.01 years and a mean BMI of 21.11 ± 6.66.
Of the 176 patients, we identified eight (4.5%) who suffered from SSI following PSF. Of the eight SSIs identified, one suture abscess and one superficial infection were managed conservatively in the clinic setting. Six infected patients, three with seroma, one with superficial, and two with deep infections, returned to the OR, including five for irrigation and debridement and one for removal of hardware (Table 1).
Table 1: Surgical Site Infection (SSI) management and patient-related factors.
Patient no. |
Age |
BMI |
Scoliosis diagnosis |
SSI type |
Description of SSI management |
42 |
15 |
32.59 |
idiopathic |
seroma |
irrigation & debridement |
44 |
11 |
26.91 |
neuromuscular |
deep |
irrigation & debridement |
49 |
2 |
18.31 |
congenital |
deep |
irrigation & debridement |
62 |
14 |
17.16 |
idiopathic |
seroma |
removal of hardware |
76 |
12 |
18.84 |
neuromuscular |
superficial |
clinic/conservative |
81 |
15 |
19.82 |
idiopathic |
superficial |
irrigation & debridement |
118 |
13 |
43.91 |
idiopathic |
seroma |
irrigation & debridement |
140 |
10 |
15.39 |
idiopathic |
suture abscess |
clinic/conservative |
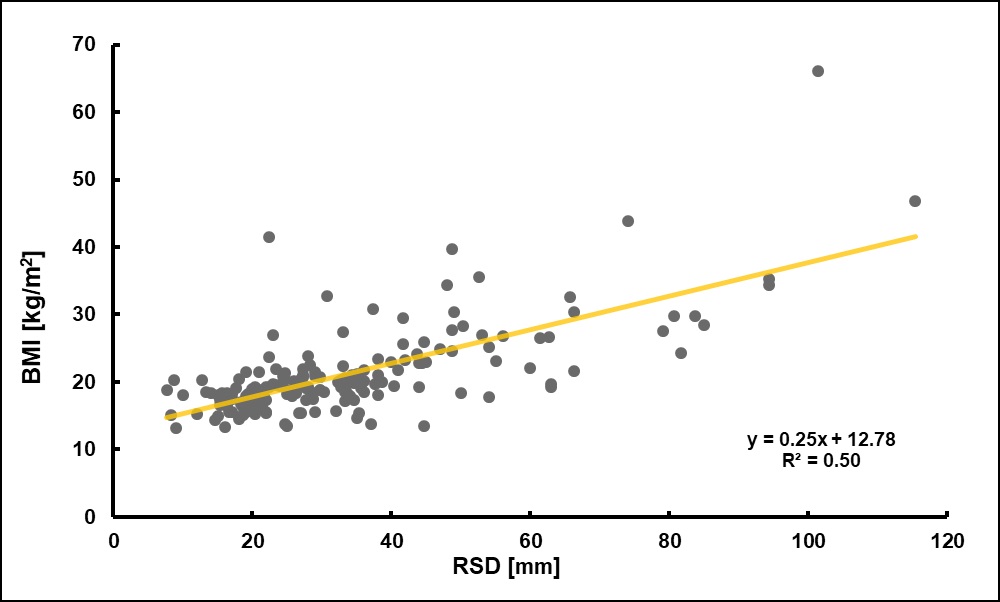
The mean RSD measured 33.9 ± 19.0 mm (range, 7.7-115.3) (Figure 2). There was no statistical significance comparing the mean RSD for subjects who had a SSI (33.6 mm) and for those who did not (35.1 mm). Backward stepwise logistic regression analysis yielded no statistically significant predictors for SSI. However, there was a strong, statistically significant linear prediction between RSD and BMI (r=0.71, p=0.001).
Discussion
Scoliosis is the most common spinal deformity seen in children, with reported prevalence ranging from 1-3% globally [1,2]. For cases in which deformity is severe or there is a high risk of progression, Posterior Spinal Fusion (PSF) is often employed to correct and stabilize spinal alignment. PSF carries a known risk of Surgical Site Infection (SSI). This risk varies widely depending on etiology, with idiopathic and neuromuscular scoliosis carrying the lowest and highest risks respectively [3].
The consequences of SSI following an orthopaedic procedure are numerous and include increased length of hospital stay, greater risk of rehospitalization, decreased physical mobility, and lower health-related quality of life [6]. Furthermore, the financial costs associated with treating an orthopaedic SSI are substantial [7], and while modern treatment methods are generally successful at eliminating deep infection, they are not without a high risk of morbidity [3,8]. In the case of PSF for scoliosis, hardware removal is often necessary, risking progression of the spinal deformity [9].
For patients in the current study, the incidence of SSI was 4.5% (n=176). Given our patient population’s mixture of diagnoses, including 21.6% with neuromuscular scoliosis, this falls within the wide range of previously reported incidence rates in the U.S., which are as low as 0.5% for idiopathic scoliosis and as high as 14.3% for neuromuscular scoliosis [3]. Our distribution of the severity of SSIs also mirrors that of previously published data, with a range from conservatively treated suture abscesses, to recalcitrant infections requiring hardware removal [9].
To varying degrees, both high BMI and subcutaneous fat thickness have been associated with incidence of SSI following PSF in adult patient populations [4,5,10,11]. Mehta et al. found the distribution of body mass to be more predictive of SSI risk following lumbar spinal fusion than BMI alone [11]. Thus, further characterization of the association between body habitus and the development of SSI is needed to increase the clinical utility of these findings. We sought to examine these associations in children. Our goal was to identify a more readily accessible patient variable to quantify body fat distribution around the surgical site. RSD is easily measurable, requiring only lateral plain radiographs to determine.
Although there was no statistically significant correlation between RSD and incidence of SSI, we did find a statistically significant correlation between RSD and BMI (r=0.71). This suggests that there may be utility for RSD as a surrogate for BMI in situations where obtaining an accurate height measurement is difficult, including cases involving patients with neuromuscular scoliosis.
This report contains several limitations. With a relatively small sample size of 176 subjects, just 8 instances of SSI were identified. We hypothesize that this study was underpowered to detect any statistically significant correlation between RSD and incidence of SSI. Additionally, obtaining height and body mass values for neuromuscular patients is notoriously difficult, and this may have affected the accuracy of BMI values recorded for such patients.
Conclusion
In conclusion, RSD was not shown to be correlated with incidence of SSI. However, a statistically significant correlation was found between RSD and BMI (R=0.71, P=0.001), which suggests RSD may be useful as a substitute for BMI when BMI cannot be easily ascertained. Future studies with larger patient samples are needed to investigate any associations between body habitus and incidence of SSI in children following PSF.
References
- Lonstein JE. Screening for spinal deformities in Minnesota schools. Clinical orthopaedics and related research. 1977; 33– 42.
- Ohtsuka Y, Yamagata M, Arai S, et al. School screening for scoliosis by The Chiba University Medical School screening program. Spine 1988; 13: 1251–1257.
- Li Y, Glotzbecker M, Hedequist D. Surgical site infection after pediatric spinal deformity surgery. Current reviews in musculoskeletal medicine. 2012; 5: 111–119.
- Abdallah DY, Jadaan MM, McCabe JP. Body mass index and risk of surgical site infection following spine surgery: A meta-analysis. European spine journal. 2013; 22: 2800–2809.
- Koutsoumbelis S, Hughes AP, Girardi FP, Cammisa FP, Finerty EA, et al. Risk Factors for Postoperative Infection Following Posterior Lumbar Instrumented Arthrodesis. Journal of bone and joint surgery. American volume. 2011; 93: 1627–1633.
- Whitehouse JD, Friedman ND, Kirkland KB, Richardson WJ, Sexton DJ. The Impact of Surgical‐Site Infections Following Orthopedic Surgery at a Community Hospital and a University Hospital: Adverse Quality of Life, Excess Length of Stay, and Extra Cost. Infection control and hospital epidemiology. 2002; 23: 183–189.
- Parker SL, Shau DN, Mendenhall SK, McGirt, MJ. Factors influencing 2-year health care costs in patients undergoing revision lumbar fusion procedures. Journal of neurosurgery. Spine. 2012; 16: 323–328.
- Levi AD, Dickman CA, Sonntag VK. Management of postoperative infections after spinal instrumentation. Journal of neurosurgery. 1997; 86: 975–980.
- Cahill PJ, Warnick DE, Lee MJ, Gaughan J, Vogel LE, et al. Infection After Spinal Fusion for Pediatric Spinal Deformity: Thirty Years of Experience at a Single Institution. Spine (Philadelphia, Pa. 1976), 2020; 35: 1211–1217.
- Mehta AI, Babu R, Sharma R, Karikari IO, Grunch BH, et al. Thickness of Subcutaneous Fat as a Risk Factor for Infection in Cervical Spine Fusion Surgery. Journal of bone and joint surgery. American volume. 2013; 95: 323–328.