Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
Accessory liver lobe torsion presenting after blunt abdominal trauma
Jay A Patel*; Matthew Dixon; Joshua P Hazelton; Karima Fitzgerald
Department of Surgery, Penn State Health Milton S. Hershey Medical Center, Hershey, PA, USA.
*Corresponding Author: Jay A Patel
Department of Surgery, Penn State Health Milton S.
Hershey Medical Center, Hershey, PA, USA.
Email: jpatel13@pennstatehealth.psu.edu
Received : July 07, 2021
Accepted : Aug 20, 2021
Published : Aug 25, 2021
Archived : www.jcimcr.org
Copyright : © Patel JA (2021).
Abstract
Torsion of an Accessory Liver Lobe (ALL) is a rare cause of acute abdominal pain. The presence of ALL is associated with congenital abdominal wall abnormalities, such as omphalocele or umbilical hernia, and occurs secondary to abnormal liver morphogenesis and intraabdominal hypertension causing liver hypertrophy. Torsion may be triggered by blunt abdominal trauma. We report the case of a 29-year-old male who developed torsion of an ALL arising from hepatic segment 3 after falling. The patient required urgent operative intervention for the treatment of this torsion. This presentation and disease manifestation has been very rarely reported in the literature.
Citation: Patel JA, Dixon M, Hazelton JP, Fitzgerald K. Accessory liver lobe torsion presenting after blunt abdominal trauma. J Clin Images Med Case Rep. 2021; 2(4): 1281.
Background
Hepatic torsion is extremely rare with very few reports in the literature describing its presentation. This phenomenon is related to anatomical abnormalities from hepatic parenchymal hypertrophy, such as Accessory Liver Lobes (ALL) and Riedel’s lobe, which involves hypertrophy of segments 5 and 6. There is also an association with history of previous omphalocele repair or umbilical hernia [1-4]. The etiology of the hypertrophy may be related to congenital abnormalities in morphogenesis, intra-abdominal hypertension translated to the developing liver by development of the tunica muscularis recti, and congenital abdominal wall abnormalities [3-5]. ALL, present in less than 1% of the population, can be sessile or pedunculated, containing vessels and bile ducts, and are mostly right hepatic and infrahepatic in location [2]. The true incidence is likely underestimated as the majority of ALL are asymptomatic and are incidentally discovered on imaging or during time of surgery [1,2].
We report the case of a traumatic antecedent event which led to the torsion of an ALL arising from hepatic segment 3, a presentation and disease manifestation which has been very rarely reported in the literature.
Case presentation
Our patient is a 29-year-old Mennonite male with a history of DiGeorge syndrome, prior omphalocele repair, and ventricular septal defect who presented with a 1-week history of worsening abdominal pain, nausea, and emesis. The abdominal pain began after the patient sustained a ground level fall after tripping and falling backwards while pulling a wagon. Approximately 3.5 days after event, he developed nausea, emesis, and abdominal pain, prompting the initial medical evaluation.
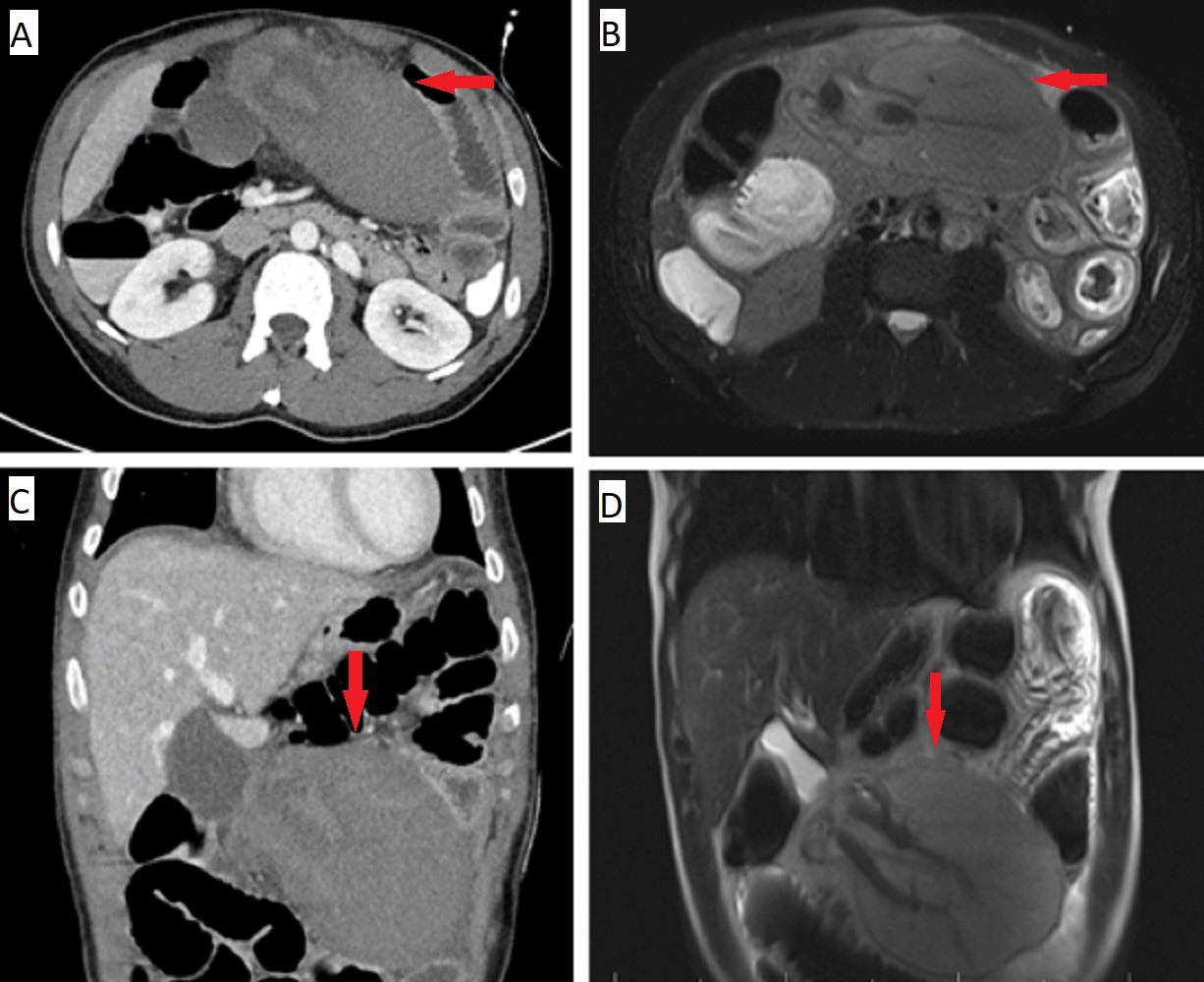
On evaluation at a referring facility, laboratory evaluation was notable for the following abnormalities: WBC 13380/microliter, AST 275 units/liter, ALT 999 units/liter, Total bilirubin 2.3 mg/deciliter, Alkaline phosphatase 120 units/liter. CT findings demonstrated a 12.6 x 9.7 x 14.2 cm mass arising from hepatic segment 3, concerning for hematoma. There was no evidence of active contrast extravasation, but there was an associated proximal small bowel obstruction due to mass effect. The patient was then transferred to our facility, a Level-1 trauma center. On physical exam, the patient had a palpable epigastric mass, focal tenderness, and mild abdominal distension. Nasogastric tube placement resulted in high output due to the bowel obstruction. Given unclear trauma presentation and atypical features of the mass, including location, continuity with the liver, and associated vascular appearing structures adjacent to the mass, CT angiogram was initially obtained, followed by MRI of the abdomen given diagnostic uncertainty, with representative images shown in Figure 1. These images demonstrated a large mass arising from segment 3 of the liver containing non-enhancing hepatic parenchyma with swirling of vascular structures entering the mass, concerning for ALL torsion with hepatic parenchymal ischemia.
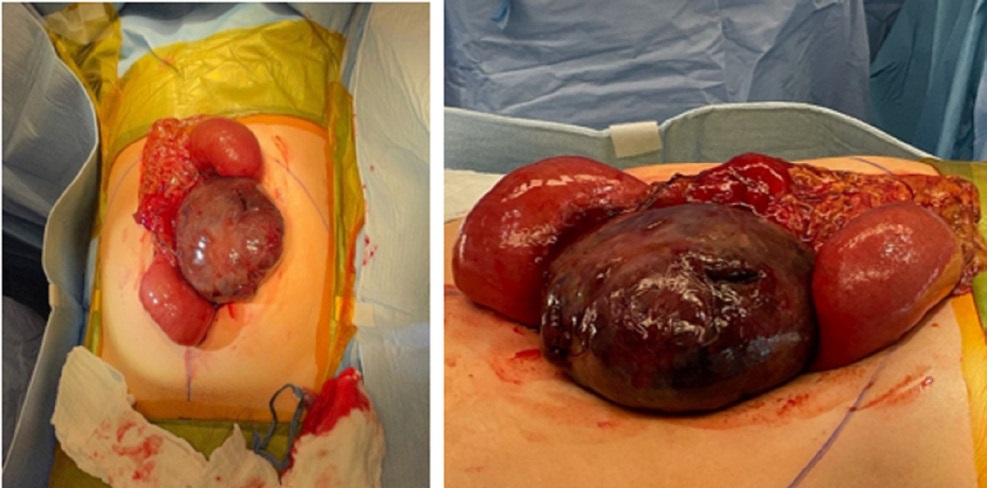
Given these findings, the patient was taken later that day to the operating room. In a combined case involving both trauma surgery and hepatobiliary surgery, an exploratory laparotomy was performed. There was small volume hemoperitoneum encountered upon entering the abdomen, as well as dilated loops of proximal small bowel. On further inspection, there was an ischemic appearing ALL arising off of a long pedicle attached to the inferior of segment 3. This had torsed around the ligamentum teres, which was causing the secondary bowel obstruction. Intraoperative findings are shown in Figure 2. The mass was detorsed with 720-degree counter clockwise rotation, revealing a long, thin pedicle feeding the ALL. Electrocautery was used to score the area of demarcation on the liver, and the mass was transected using multiple loads of a vascular stapler. There was no involvement of other segments of the liver and subsequent intra-abdominal inspection revealed no other abnormalities.
The patient progressed well post-operatively, and had return of bowel function and successful removal of nasogastric tube on post-operative day 2 and 3, respectively. He was discharged on post-operative day 5. He remained in good health on postoperative visits.
Discussion
Our patient presented after a fall and was initially thought to have a traumatic liver hematoma, later found to have torsion of an ALL. This was surgically managed with transection of the ALL from its pedicle without formal hepatic resection. Koplewitz et al. report torsion of an ALL and gallbladder in an 8-year-old female with history of omphalocele repair, which occurred after the patient’s brother jumped on her back [6]. Presentation, intraoperative findings, and surgical management were similar to that in our case. Umehara et al. report the case of a 14-yearold female with a history of omphalocele repair who developed torsion of a pedunculated ALL. The authors discuss the importance of including torsion of an ALL in the differential for acute abdominal pain in patients with a history of omphalocele repair [3]. Multiple other reports have been made of ALL torsion seen in patients with history of previous omphalocele repair, with multiple reports of this occurring in infancy [7,8]. A potential explanation for the association of omphalocele repair with ALL torsion is likely related to abnormal liver morphogenesis secondary to abnormal abdominal wall formation, leading to the formation of an ALL that is prone to torsion. Negru et al. present a similar case to ours where a 32-year-old female developed torsion of an ALL coming from hepatic segment 3, with associated bowel obstruction [9]. Diagnosis of ALL torsion may be made with various imaging modalities, with the potential role of biopsy in diagnosing the etiology of the mass, if imaging is inconclusive [10]. Most presentations may be managed with surgical resection of the ALL either by a laparoscopic or open approach. Ladurner et al. report a case of severe ischemia and hepatic dysfunction caused by ALL torsion, such that liver transplantation was required [4]. The presence of an ALL should be considered in patients with a history of abdominal wall defects in young age, such as omphalocele, and torsion should be considered as a rare cause of acute abdominal pain in this population, which may occur spontaneously or after a recent history of trauma.
References
- Lowther E, Corso O, Schammel C, Schammel D, Trocha S, Devane AM. Hepatic lobe torsion: A rare disease necessitating surgical management. Clin Imaging. 2021; 71: 121-125.
- Glenisson M, Salloum C, Lim C, Lacaze L, Malek A, Enriquez A, Compagnon P, Laurent A, Azoulay D. Accessory liver lobes: anatomical description and clinical implications. J Visc Surg. 2014; 151: 451-5.
- Umehara M, Sugai M, Kudo D, Hakamada K, Sasaki M, Munakata H. Torsion of an accessory lobe of the liver in a child: report of a case. Surg Today. 2009; 39: 80-2.
- Ladurner R, Brandacher G, Mark W, Iannetti C, Lottersberger C, Steurer W, Königsrainer A, Margreiter R. Complete hepatic ischemia due to torsion of a large accessory liver lobe: first case to require transplantation. Transpl Int. 2005; 18: 467-9.
- Natarajan S, Jayasudha, Periasamy M, Rangasamy S. Torsion of Accessory Hepatic Lobe. J Indian Assoc Pediatr Surg. 2017; 22: 55-56.
- Koplewitz BZ, Manson DE, Ein SH. Posttraumatic torsion of accessory lobe of the liver and the gallbladder. Pediatr Radiol. 1999; 29: 799-802.
- Elmasalme F, Aljudaibi A, Matbouly S, Hejazi N, Zuberi MS. Torsion of an accessory lobe of the liver in an infant. J Pediatr Surg. 1995; 30: 1348-50.
- Thakral CL, Shivalingam G, Dar FM, Thakral N. Torsion of an Accessory Hepatic Lobe with Embedded Gallbladder: In an 11-Month-Old Boy. European J Pediatr Surg Rep. 2017; 5: e62- e64.
- Negru D, Tudorache C, Marinescu M, Grigoraş M, Crumpei F, Georgescu S. Lob hepatic accesoriu torsionat si infarctat [Torsion and infarction of an accessory liver lobe]. Rev Med Chir Soc Med Nat Iasi. 2007; 111: 442-5.
- Carrabetta S, Piombo A, Podestà R, Auriati L. Torsion and infarction of accessory liver lobe in young man. Surgery. 2009; 145: 448-9.