Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
Diabetes insipidus as the first manifestation of granulomatosis with polyangiitis: A case report
Aram Behdadnia; Marjan Jeddi; Alireza Estedlal*
Endocrinology and Metabolism Research Center, Shiraz University of Medical Sciences, Shiraz, Iran.
*Corresponding Author: Alireza Estedlal
Health Policy Research Center, Institute of Heath,
Shiraz University of Medical Sciences, Shiraz, Fars,
Iran.
Email: estedlal.alireza@gmail.com
Received : July 12, 2021
Accepted : Aug 28, 2021
Published : Sep 02, 2021
Archived : www.jcimcr.org
Copyright : © Estedlal A (2021).
Abstract
Background: Granulomatosis with Polyangiitis (GPA) is a necrotizing granulomatosis vasculitis that may influence most organs, but posterior pituitary involvement as the first manifestation is unusual. However, there are some case reports in this regard.
Case presentation: A 49-year-old menopausal woman presented with polyuria, polydipsia and weight loss over time headache, purulent nasal discharge, malaise, ear pain developed. After right myringotomy due to secretory otitis media and nasal cavity biopsy, the symptoms exacerbated. Diabetes insipidus was documented by Deprivation test. Thus, 20 microgram nasal spray DDAVP was prescribed. Pituitary MRI +/- Gad demonstrated pituitary involvement. Pituitary axis hormone evaluation was consistent with menopausal state. Chest spiral CT scan showed speculated border soft tissue mass lesion.
GPA confirmed with ACR criteria and C-ANCA positive. Therefore, corticosteroid and rituximab were started. Symptoms of DI responded well to the treatment and the spray dosage was decreased.
Conclusion: DI can be the first manifestation of GPA; although it is rare, it is worth to be diagnosed early and serious treatment of vasculitis should be started to prevent irreversible damage to the hypophysis cell and unnecessary procedure.
Keywords: GPA; granalomatosis vasculitis; diabetes insipidus.
Citation: Behdadnia A, Jeddi M, Estedlal A. Diabetes insipidus as the first manifestation of granulomatosis with polyangiitis: A case report. J Clin Images Med Case Rep. 2021; 2(5): 1291.
Introduction
Granulomatosis with Polyangiitis (GPA) is a form of systemic vasculitis (polyangiitis) with necrotizing granulomatous inflammation of the upper and lower respiratory tracts, systemic necrotizing vasculitis, and necrotizing glomerulonephritis. It is usually associated with the presence of anti-neutrophil cytoplasmic antibodies (ANCAs).[1] Patients with Granulomatosis with Polyangiitis (GPA) typically have both upper airway and pulmonary involvement. Although neither sensitive nor specific, common complaints and signs of GPA include fatigue, fever, anorexia, weight loss, arthralgia, rhinosinusitis, cough and dyspnea, urinary abnormalities (an active urine sediment) with or without renal insufficiency, purpura, and neurologic dysfunction [2].
Patients with ANCA-associated vasculitides may less commonly develop clinical manifestations involving the nervous system. Peripheral Nervous System (PNS) involvement is noted in approximately 15 percent of patients with GPA, and Central Nervous System (CNS) involvement is much less common [3]. There are several case reports and experiences regarding pituitary involvement in GPA [4-7]. In addition, pituitary involvement leading to Central Diabetes Insipidus (CDI) is extremely uncommon and is generally thought to occur later in the disease course. Only a limited number of cases of pituitary involvement presenting as the initial manifestation of GPA have been reported [8,9].
The aim of this study was to describe the clinical and biological characteristics of a case of granulomatosis with polyangiitis with initial manifestation of diabetes insipidus and subsequently review the disease course, response to treatment, and the patient outcome.
Case presentation
A 49-year-old postmenopausal woman with no significant medical history presented with a 70-day history of polyuria, polydipsia and weight loss. With first impression of diabetes mellitus (DM), a complete evaluation of medical history and the laboratory tests showed that DM was unlikely (FBS: 105 mg/ dl). During the course of the disease, the patient had developed malaise, ear pain and fullness, tinnitus, facial pain and pressure, frontal headache and purulent nasal discharge. Otorhinolaryngologist requested spiral CT scan of the temporal bone and posterior fossa and spiral CT scan of paranasal sinuses. The findings were soft tissue density in the right middle ear surrounding the ossicles and right mastoid air cells suggestive of mastoiditis and otitis media. In addition, opacifications in the left maxillary sinus and left nasal cavity were seen. Hearing test revealed moderate conductive hearing loss in the right ear. With impression of secretory otitis media, right myringotomy was done and biopsy from the lesion in the left nasal cavity was obtained by an otorhinolaryngologist. After operation, the patient’s symptoms were exacerbated and she was admitted in the internal ward with complaints of malaise, polyuria, polydipsia, anorexia, weight loss, purulent nasal discharge, and headache. In the physical examination, the patient had moderate tenderness on the left maxillary sinus and a grossly necrotic appearing sputum. The other items were normal. Analysis of 24- hour urine collection showed a volume of 3.5 liters in 24 hours with urine specific gravity of 1.002. Water deprivation test was done for the patient for 4 hours. Urine specific gravity was the same with a significant rise of serum Na from 148 mEq/L to 151 mEq/L (135-145 mEq/L) and the patient developed decreased blood pressure from 120/80 to 105/60. Her weight decreased about 800g. Due to severe signs of dehydration, it was stopped, and 20µg desmopressin spray was administered for the patient. Urine specific gravity increased to 1.012 and serum Na changed to 143 mEq/L (135-145 mEq/L). There is no facility to check Copeptin in this department. These results were consistent with central diabetes insipidus. With this impression, a dynamic pituitary and hypothalamus MRI with contrast and brain MRI was requested. SagittalT2 WI MRI demonstrated 16*10*8.5mm non-homogenous pituitary mass.
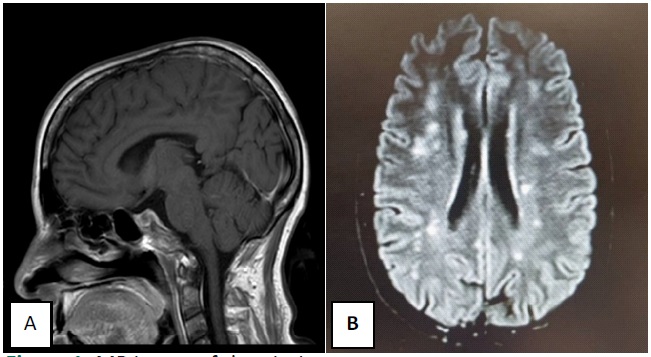
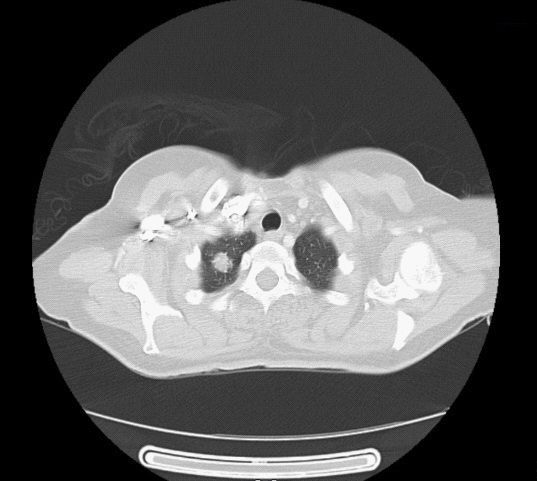
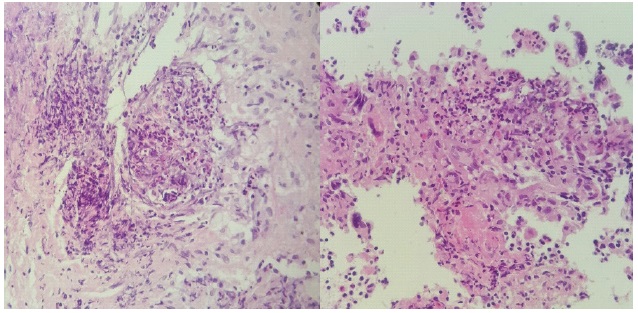
Axial, coronal and sagittal T1W MRI image before and after Gadolinium revealed non-homogenous enlarged pituitary gland and absent posterior Pituitary bright spot, The hypo signal area in the center and posterior aspect does not enhanced suggestive necrosis. Also, T2/FLAIR hypersignal foci were seen in deep periventricular white matter in favor of vasculitis (Figure 1). Spiral chest CT-scan also showed spiculated border soft tissue mass lesion with 18 x 17 mm in the apex of the right lung (Figure 2). Lung biopsy was recommended, but the patient did not accept. Besides, pathology of the nasal lesion showed necrotizing granulomatous vasculitis, highly suggestive of GPA (Figure 3). Diagnosis of GPA was determined, and the patient was candidate for treatment with intravenous pulse methylprednisolone and rituximab; subsequently, intravenous pulse methylprednisolone 500 mg was administered for 3 days. Polyuria and polydipsia were resolved predominantly after administration of desmopressin spray and the last urine specific gravity was 1.045. An overview for other pituitary axis insufficiencies was done; however, no significant finding was detected (Table 1).
Table 1: Laboratory data during admission:
Hematology |
White blood cells (WBC) count - 109/L |
6.7 |
|
Red blood cell (RBC) count - 1012/L |
3.64 |
||
Hemoglobin - g/dl |
10.1 |
||
Platelets count - 109/L |
326 |
||
Mean corpuscular volume (MCV) - µm3 |
89.3 |
||
Red cell distribution width (RDW) - % |
11.4 |
||
Biochemistry |
Blood urea nitrogen (BUN) – mg/dl |
6 |
|
Creatinine (Cr) – mg/dl |
0.7 |
||
Sodium (Na) – mEq/L |
134 |
||
Potassium (K) - mEq/L |
4.6 |
||
Fasting blood sugar (FBS) - mg/dl |
105 |
||
Magnesium (Mg) - mg/dl |
2.1 |
||
Calcium (Ca) - mg/dl |
9.7 |
||
Phosphorus (Ph) - mg/dl |
3.8 |
||
Blood gas analysis |
PH |
7.47 |
|
PCO2 |
39.4 |
||
PO2 |
33.4 |
||
HCO3 – mmol/L |
28.6 |
||
Coagulation profile |
PT - sec |
15.7 |
|
INR |
1.16 |
||
PTT - sec |
32 |
||
Liver function tests |
AST – U/L |
12 |
|
ALT – U/L |
16 |
||
Alkaline Phosphatase – U/L |
438 |
||
Total bilirubin – mg/dl |
0.4 |
||
Direct bilirubin – mg/dl |
0.2 |
||
Protein – g/dl |
7.9 |
||
Albumin g/dl |
3.6 |
||
Endocrine laboratory data |
FSH – mlu/ml |
31.5 |
|
LH – mlu/ml |
5.3 |
||
Prolactin ng/ml |
37 |
||
T3 – ng/ml |
1.2 |
||
T4 - µg/ml |
8.6 |
||
TSH - µlu/ml |
1.1 |
||
Anti-TPO – lu/ml |
56.1 |
||
Cortisol µg/dl |
12 |
||
Rheumatologic laboratory data |
C3 – mg/dl |
123 |
|
C4 – mg/dl |
19.9 |
||
ANA |
0.6 |
||
C-ANCA – AU/ml |
39.9 |
||
P-ANCA – AU/ml |
5.6 |
||
others |
Urine specific gravity |
1002 |
|
24h Urine |
Volume - ml |
3500 |
|
Cr - mg |
630 |
||
Protein - mg |
350 |
||
Blood culture |
Negative |
||
Urine culture |
Negative |
||
PCR for COVID-19 |
Negative |
||
ESR – mm/hr |
104 |
||
CRP – mg/L |
138 |
||
CPK – U/L |
20 |
||
LDH – U/L |
413 |
||
Discussion
Here, we present a case of central diabetes insipidus who presented with the initial symptom leading to the diagnosis of GPA. CDI was documented with deprivation test and pituitary and brain involvement was found in pituitary and brain MRI. Diagnosis of Wegner was established by ACR criteria: Nasal inflammation, Abnormal chest Ct scan, Granulomatous inflammation on nasal biopsy beside positive C-ANCA.
The patient responded well to desmopressin therapy, corticosteroid intravenous pulses and Rituximab. It is worth mentioning that after treatment with corticosteroid pulses, the patient responded to lower doses of DDAVP spray.
Diabetes insipidus is the most common manifestation of GPA with pituitary involvement [4]. However, Central Diabetes Insipidus (CDI) is a rare complication of GPA, which usually presents after pulmonary or kidney involvement [10,11], and CDI as a presenting manifestation of GPA is only reported in case reports [8,12-14]. Patients with GPA may develop clinical manifestations involving the nervous system. Presentations of neurologic Granulomatosis with Polyangiitis (GPA) are extremely varied with manifestations in the peripheral nervous system [15]. Other neurologic manifestations include seizures, cerebritis, stroke syndromes, and granulomas extending from the sinuses, which may affect the pituitary gland, resulting in diabetes insipidus [16,17]. Therefore, it is essential to remember that uncommon presentations may result in delay in diagnosis and may be mistakenly treated with ineffective treatments.
Given the radiological assessment, pituitary enlargement in computed tomography or MRI is the most common finding [18-21], while normal pituitary gland imaging was also reported [22-24]. This demonstrates the usefulness of MR imaging in the evaluation of diseases of the hypothalamic-pituitary axis. In our patient, there was a non-homogenous mass with hypo-signal area in the center and posterior aspect of it without enhancement and without bright spot in the posterior part of the pituitary. Moreover, regarding the laboratory data, in this patient anterior pituitary hormone levels were in the normal range for postmenopausal stage. Reviewing case reports, anterior pituitary dysfunction has been documented in three patients with diabetes insipidus secondary to GPA [8,9]. Our patient was successfully treated with a combination of corticosteroid pulses Rituximab. Diabetic symptoms resolved predominantly and DDAVP administration was decreased. Successful treatment of DI, as documented by discontinuation of vasopressin, was described in the previous reports [9,18], but our patient needed low dose of DDAVP spray. Other treatment regimens, with combination of prednisone and cyclophosphamide were also reported [13].
Acknowledements: The authors would like to thank Shiraz University of Medical Sciences, Shiraz, Iran and Center for Development of Clinical Research of Namazi Hospital and Dr. Nasrin Shokrpour for editorial assistance.
References
- Hoffman GS, Kerr GS, Leavitt RY, Hallahan CW, Lebovics RS, Travis WD, et al. Wegener granulomatosis: An analysis of 158 patients. Annals of internal medicine. 1992; 116: 488-98.
- Falk RJ, Hogan S, Carey TS, Jennette JC. Clinical course of antineutrophil cytoplasmic autoantibody-associated glomerulonephritis and systemic vasculitis. The Glomerular Disease Collaborative Network. Annals of internal medicine. 1990; 113: 656-63.
- Pagnoux C, Guillevin L. Peripheral neuropathy in systemic vasculitides. Current opinion in rheumatology. 2005; 17: 41-8.
- Kapoor E, Cartin-Ceba R, Specks U, Leavitt J, Erickson B, Erickson D. Pituitary dysfunction in granulomatosis with polyangiitis: the Mayo Clinic experience. The Journal of Clinical Endocrinology & Metabolism. 2014; 99: 3988-94.
- Liu S, Xu Y, Li N, Chen S, Zhang S, Peng L, et al. Pituitary involvement in granulomatosis with polyangiitis: A retrospective analysis in a single Chinese hospital and a literature review. International journal of endocrinology. 2019; 2019.
- De Parisot A, Puechal X, Langrand C, Raverot G, Gil H, Perard L, et al. Pituitary involvement in granulomatosis with polyangiitis: Report of 9 patients and review of the literature. Medicine. 2015; 94.
- Gu Y, Sun X, Peng M, Zhang T, Shi J, et al. Pituitary involvement in patients with granulomatosis with polyangiitis: case series and literature review. Rheumatology international. 2019; 39: 1467- 76.
- Garovic VD, Clarke BL, Chilson TS, Specks U. Diabetes insipidus and anterior pituitary insufficiency as presenting features of Wegener’s granulomatosis. American journal of kidney diseases: The official journal of the National Kidney Foundation. 2001; 37: E5.
- Czarnecki EJ, Spickler EM. MR demonstration of Wegener granulomatosis of the infundibulum, a cause of diabetes insipidus. AJNR American journal of neuroradiology. 1995; 16: 968-70.
- Hurst NP, Dunn NA, Chalmers TM. Wegener’s granulomatosis complicated by diabetes insipidus. Annals of the rheumatic diseases. 1983; 42: 600-1.
- Rosete A, Cabral AR, Kraus A, Alarcón-Segovia D. Diabetes insipidus secondary to Wegener’s granulomatosis: report and review of the literature. The Journal of rheumatology. 1991; 18: 761-5.
- Al-Fakhouri A, Manadan A, Gan J, Sreih AG. Central diabetes insipidus as the presenting symptom of granulomatosis with polyangiitis. Journal of clinical rheumatology: Practical reports on rheumatic & musculoskeletal diseases. 2014; 20: 151-4.
- Miesen WM, Janssens EN, van Bommel EF. Diabetes insipidus as the presenting symptom of Wegener’s granulomatosis. Nephrology, dialysis, transplantation: Official publication of the European Dialysis and Transplant Association - European Renal Association. 1999; 14: 426-9.
- Narvaez Ponce L, Carrio J, Soriano ER, Santos CD, Imamura PM, Catoggio LJ. [Insipid diabetes as initial presentation of Wegener’s granulomatosis]. Revista de la Facultad de Ciencias Medicas (Cordoba, Argentina). 2009; 66: 31-5.
- Söderström A, Revaz S, Dudler J. Cranial neuropathies in granulomatosis with polyangiitis (Wegener’s): A case-based review. Clinical rheumatology. 2015; 34: 591-6.
- Asakura K, Muto T. Neurological involvement in Wegener’s granulomatosis. Brain and nerve=Shinkei kenkyu no shinpo. 2013; 65: 1311-7.
- Huang Y-H, Ro L-S, Lyu R-K, Chang H-S, Wu Y-R, et al. Wegener’s granulomatosis with nervous system involvement: a hospitalbased study. European neurology. 2015; 73: 197-204.
- Rosete A, Cabral A, Kraus A, Alarcon-Segovia D. Diabetes insipidus secondary to Wegener’s granulomatosis: report and review of the literature. The Journal of rheumatology. 1991; 18: 761-5.
- Garovic VD, Clarke BL, Chilson TS, Specks U. Diabetes insipidus and anterior pituitary insufficiency as presenting features of Wegener’s granulomatosis. American Journal of Kidney Diseases. 2001; 37: e5.
- Berthier S, Gil H, Bonneville J, Magy N, De Wazieres B, Mallet H, et al., editors. Wegener’s disease and central diabetes insipidus. Annales D’endocrinologie. 2000.
- Yong TY, Li JY, Amato L, Mahadevan K, Phillips PJ, et al. Pituitary involvement in Wegener’s granulomatosis. Pituitary. 2008; 11: 77-84.
- Goebel R, Jakse R, Passath A, Michlmayr G. Wegener’s granulomatosis causing diabetes insipidus. Fortschritte der Medizin. 1982; 100: 1400-2.
- Hurst N, Dunn N, Chalmers T. Wegener’s granulomatosis complicated by diabetes insipidus. Annals of the rheumatic diseases. 1983; 42: 600-1.
- Xue J, Wang H, Wu H, Jin Q. Wegener’s granulomatosis complicated by central diabetes insipidus and peripheral neutrophy with normal pituitary in a patient. Rheumatol Int. 2009; 29: 1213-7.