Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
Clinical evolution of hepatitis delta virus genotype 3 infection in patients from the Western Amazon, Brazil
Suyane da Costa Oliveira1,2; Eugênia de Castro Silva2; Miriam Ribas Zambenedetti4; Soraya dos Santos Pereira1,2; Ivo Alberto Borghetti4; Mariana Pinheiro Alves Vasconcelos3; Lourdes Maria Pinheiro Borzacov3; Fabricio Klerynton Marchini4,5; Luis Gustavo Morello4,5; Marco Aurélio Krieger5; Juan Miguel Villalobos Salcedo1,2,3; Deusilene Souza Vieira1,2; Rita de Cassia Pontello Rampazzo3*
1 Laboratório de Virologia Molecular da Fundação Oswaldo Cruz Rondônia, Porto Velho, RO, Brazil.
2 Universidade Federal de Rondônia, Programa de Pós-Graduação em Biologia Experimental, Porto Velho, RO, Brazil
3 Ambulatório Especializado em Hepatites Virais do Centro de Pesquisa em Medicina Tropical, Porto Velho, RO, Brazil.
4 Instituto de Biologia Molecular do Paraná, Curitiba, PR, Brazil.
5 Instituto Carlos Chagas-ICC/FIOCRUZ, Curitiba, PR, Brazil.
*Corresponding Author: Rita de Cassia Pontello
Rampazzo
Specialized Outpatient Clinic in Viral Hepatitis,
Research Center in Tropical Medicine, Porto Velho,
RO, Brazil.
Email: rcprampazzo@gmail.com
Received : July 13, 2021
Accepted : Sep 03, 2021
Published : Sep 08, 2021
Archived : www.jcimcr.org
Copyright : © Rampazzo RDCP (2021).
Abstract
Background: Chronic infection with the Hepatitis Delta Virus (HDV) is often associated with severe liver decompensation and fulminant hepatitis, but in some cases, it can present a stable clinical presentation.
Objectives: This study evaluated the clinical evolution of HDV-3 carriers from an endemic region of the western Brazilian Amazon.
Methods: Cross-sectional study was carried out with Anti-HDAg reagent patients, seen at an outpatient clinic specialized in viral hepatitis located in Rondônia, Brazil.
Findings: A total of 19 patients, 68.4% male and 31.6% female, aged between 23 and 65 years old, were evaluated; 84.2% were clinically classified as carriers of the decompensated disease and 15.8% as carriers of the inactive disease. The results of the clinical evaluation were related to viral load; 30.8% had detectable viral RNA, and even though it was not possible to establish an association between the stage of the disease and persistent viral replication (p> 0.05), persistent viral replication was predictive of early evolution for liver cirrhosis.
Conclusion: The results demonstrate the possibility that viral load can be used as a noninvasive hepatic marker in the clinical management of Hepatitis Delta.
Keywords: chronic; hepatitis D; hepatitis delta virus; liver diseases.
Citation: Oliveira SDC, Silva EDC, Zambenedetti MR, Pereira SDS, Borghetti IA. Clinical evolution of hepatitis delta virus genotype 3 infection in patients from the Western Amazon, Brazil. J Clin Images Med Case Rep. 2021; 2(5): 1303.
Introduction
The hepatitis Delta, or D, virus (HDV) is a defective virus, which depends on the Hepatitis B virus (HBV) [1] to complete its replicative process [1–3]. Cases of simultaneous HBV/HDV infection show resolvability more than 95% of the time [4], but more than 70% of chronic HBV carriers who subsequently become infected with HDV evolve to chronicity and present persistent viral replication [5].
After chronicity, patients may present a stable clinical state or progress to severe hepatic decompensation [6–9]. Clinical studies demonstrate that the risk of developing cirrhosis is three times higher compared to patients who are monoinfected with HBV and it occurs in about two-thirds of cases [10] in periods shorter than 5 years [11]. In addition, HDV infection increases the possibilities of developing Cellular Hepatocarcinoma (HCC) by 3.2 times [12].
The determinants for clinical evolution still remain difficult to interpret and pathogenesis is generally related to the viral genotype [5]. Genotype 1 is ubiquitous and has been linked to sporadic outbreaks in indigenous populations [13]; however, HDV-3, restricted to the Amazon basin, is considered the most virulent strain, associated with acute liver failure and death within a few weeks [7,14,15]. The aim of this study was to evaluate the clinical evolution of patients with HDV-3 infection from an endemic region of the Western Brazilian Amazon.
Materials and methods
Study population
A cross-sectional study was carried out with Anti-HDAg reagent patients, seen at an outpatient clinic specialized in viral hepatitis located in Rondônia, Brazil.
Eligible patients were from the Western Brazilian Amazon region (Figure 1), had serological evidence of HDV (Anti-HDAg positive) and HBV infection (HsAg positive), were between 18 and 70 years of age, were not pregnant and/or indigenous and had no coinfection with HCV (Anti-HCV negative) nor HIV (AntiHIV negative). All of them had a history of at least 2 (two) positive tests for RNA-HDV detection, were continuously monitored by the team of professionals, and had laboratory and clinical data available for consultation.
Clinical-epidemiological analysis
All participants underwent a medical consultation, followed by collection of 10 mL of venous blood. Epidemiological data; previous medical history and results of imaging exams (ultrasound of total abdomen and upper digestive endoscopy), liver biopsy and/or elastography; hematological tests (hematocrit level, leukocyte count, platelet count and determination of prothrombin activity time); biochemicals (level of liver transaminases, bilirubin, albumin, alkaline phosphatase and γ-glutamyl transferase) and serological markers for HBV, HDV, HCV and HIV, performed in the 6 months prior to entry into the study were recorded.
Patients with a history of clinical events related to liver decompensation (increased transaminases, thrombocytopenia, fibrosis, cirrhosis, ascites, hepatic encephalopathy, esophageal varices and/or esophageal hemorrhages) were classified as having Chronic Liver Disease (CLD). Information on treatment with Nucleotide Analogs (NTA) and Nucleoside Analogs (NSA) and/ or Interferon-based regimens (IFN) carried out in the previous semester were also recorded.
Laboratory data and age were used to determine the FIB-4 and APRI scores [16, 17], non- invasive methods used to estimate the degree of fibrosis and the presence or absence of liver cirrhosis.
Extraction of viral RNA
The viral RNA was extracted from 200 µL of serum, using the QIAamp® viral RNA Mini Kit (QIAgen® Inc., Germany), following the manufacturer's instructions. The RNA was eluted in 60 µL of elution buffer.
HDV Viral Load
A multiplex one-step RT-qPCR assay, which simultaneously amplifies the HDV ribozyme and a single copy endogenous control from the human host, was used for quantitative and qualitative detection of the viral pathogen and human control.
The reaction was performed on an ABI 7500 real-time PCR platform (Applied Biosystems®, Foster City, CA, USA) under the following conditions: 60ºC for 30 minutes for reverse transcription, 95ºC for 10 minutes, followed by 45 cycles at 95ºC for 15 seconds for initiator annealing and 60ºC for 1 minute, a stage in which new strands are polymerized and, consequently, fluorescence is detected.
Viral genotyping
For genotyping, a protocol including extraction, reverse transcription and nested-PCR [18] were followed. The amplified product was sent off for sequencing using the Sanger method. The software MEGA X20 was used for editing and assembling the consensus strands. Then, the strands were aligned with 223 complete HDV sequences deposited in Genbank through Clustal W2.1.20, to determine the genotype of the samples.
Statistical analysis
Statistical analyses were performed with a 95% confidence interval, using the statistical software GraphPad Prism 8.4.0 ®. Categorical covariates were compared using the chi-square test or Fisher's exact test, when appropriate. Continuous variables were given means, minimum, maximum, and standard deviation and, when necessary, an ANOVA Two-way test was performed for comparison between groups. Results with p-value <0.05 were considered statistically significant.
Ethics
This study was approved by the local Research Ethics Committee (33CEP/2010/CEPEM).
Results
Epidemiological and clinical characterization of the study population
A total of 19 patients met the inclusion criteria, 13 male (68.4%) and 6 (31.6%) female. All were between 23 and 65 years of age (average 47.7 years old and SD 10.9 years old).
According to criteria established in the methodology, 84.2% of the individuals (16/19) were classified as having CLD and 15.8% did not show signs of liver disease and were included in the group of inactive carriers. Of the total, 64.2%/(12/19) had a history of recent treatment with interferon and/or nucleos(t) ide analogs.
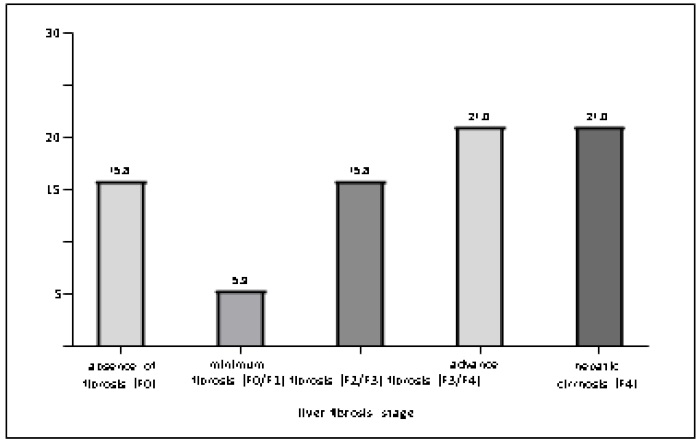
The results reported in elastography and/or liver biopsy tests are described in Figure 2. In the assessment of liver damage through imaging tests, 15.8% (3/19) of patients did not present any apparent liver injury (F0); 5.3% (1/19) had a minimum degree of fibrosis; 15.8% (3/19), moderate fibrosis; 21.0% (4/19), advanced fibrosis; and 21.0% (4/19) had progressed to liver cirrhosis.
HDV viral load
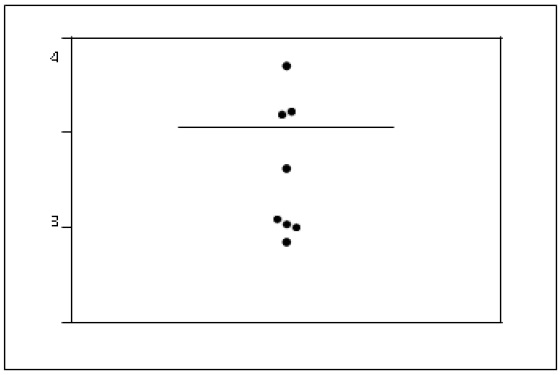
Of the total samples tested, 30.8% (8/19) presented detectable viral RNA (Erro! Fonte de referência não encontrada.) and the viral load varied from 70.5 to 5059.5 copies/mL (mean of 1129.4 copies).
Relationship between viral load and clinical classification
The correlation between clinical stage and viral load is described in Table 1. The results show that HDV viral load did not correlate with liver damage (p> 0.05); but in the group of carriers with detectable viral load, age was associated with the development of liver cirrhosis (p 0.001).
Table 1: Clinical classification of HBV carriers positive for anti-HDV, separated into groups of patients with detectable and non-detectable HDV RNA.
Clinical Characterization |
Detectable viral load (n=8) |
Non-detectable viral load (n=11) |
P-value |
CLD stage |
|
|
|
Active disease n (%) |
7 (36.8) |
9 (47.4) |
> 0.999 |
Inactive disease n (%) |
1 (5.3) |
2 (10.5) |
|
Presence of cirrhosis |
|
|
|
Total cases n (%) |
2 (10.5) |
6 (31.6) |
0.352 |
Average mean age (min. - max.) |
31 (23-39) |
53.5 (46-57) |
0.001 |
Presence of mild fibrosis |
|
|
|
Total cases n (%) |
0 (0.0) |
1 (5.3) |
>0.100 |
Average mean age (min. - max.) |
- |
- |
- |
Presence of moderate fibrosis |
|
|
|
Total cases n (%) |
2 (10.5) |
1 (5.3) |
0.546 |
Average mean age (min. - max.) |
41.5 (38-45) |
- |
- |
Presence of advanced fibrosis |
|
|
|
Total cases n (%) |
3 (15.8) |
1 (5.3) |
0.262 |
Average mean age (min. - max.) |
48.3 (46-52) |
- |
- |
Influence of Laboratory Parameters and Treatment on HDV Viral Load
The presence of thrombocytopenia or elevated levels of liver transaminases were not predictive of HDV active viral replication. Detection of HBV DNA, HBeAg, or the implementation of treatment are also not correlated with viremia (Table 2).
Table 2: Laboratory data of HBV patients who were anti-HDV positive are separated into two groups, those with detectable HDV RNA and those with non-detectable HDV RNA.
Parameters |
Detectable viral load (n=8) |
Non-detectable viral load (n=11) |
P-value |
Platelets |
|
|
|
Thrombocytopenia n (%) |
2 (10.5) |
4 (21.0) |
>0.9999 |
Hepatic Transaminases |
|
|
|
Elevated AST n (%) |
4 (21.0) |
4 (21.0) |
0.6577 |
Elevated ALT n (%) |
3 (15.8) |
4 (21.0) |
>0.9999 |
HBV |
|
|
|
Detectable viral load n (%) |
4 (21.0) |
9 (47.4) |
0.3189 |
HBeAg reagent n (%) |
2 (10.5) |
4 (21.0) |
>0.9999 |
Treatment |
|
|
|
IFN n (%) |
1 (5.3) |
1 (5.3) |
>0.9999 |
NTA/NSA n (%) |
2 (25.0) |
6 (31.6) |
0.3521 |
IFN + NTA/NSA n (%) |
- |
2 (10.5) |
0.4854 |
No treatment n (%) |
5 (26.3) |
2 (10.5) |
0.0698 |
Legend: IFN: Interferon; NSA: Nucleoside Analogs; NTA: Nucleotide Analogs.
Validation of APRI and FIB-4 as scores of anticipation of clinical events associated with Hepatitis Delta progression
The results of liver biopsy and/or elastography were compared to the FIB-4 and APRI scores data described in Table 3. The evaluated indices were not in agreement (p< 0.05) with the results of liver damage obtained through imaging exams.
Table 3: Correlation between liver damage seen in liver biopsy and/or elastography tests and FIB-4 and APRI scores of HDV patients.
Non-Invasive Marker |
Observed Liver Damage |
||||
Inactive CLD (F0) |
Mild fibrosis (F0/F1) |
Moderate fibrosis (F2/F3) |
Advanced fibrosis (F3/F4) |
Cirrhosis (F4) |
|
FIB-4 score |
n (%) |
n (%) |
n (%) |
n (%) |
n (%) |
F0/F1 |
2 (10.5) |
1 (10.5) |
1 (10.5) |
2 (10.5) |
3 (15.8) |
F2 |
1 (10.5) |
- |
1 (10.5) |
1 (10.5) |
1 (10.5) |
F3/F4 |
- |
- |
1 (10.5) |
1 (10.5) |
4 (21.0) |
APRI score |
n (%) |
n (%) |
n (%) |
n (%) |
n (%) |
F0/F1 |
3 (15.8) |
1 (10.5) |
1 (10.5) |
3 (15.8) |
4 (21.0) |
F2 |
- |
- |
2 (10.5) |
- |
1 (10.5) |
F3/F4 |
- |
- |
- |
1 (10.5) |
3 (15.8) |
Degree of liver damage in treated patients
The degree of liver damage seen on imaging tests and treatment administered was correlated. There were 16 patients (84.2%) with varying degrees of liver fibrosis and cirrhosis, 5 (26.3%) untreated. Among the 3 (15.8%) patients with no signs of liver damage evident on imaging studies, 1 (5.3%) was recently treated with interferon and / or nucleus analogue (t) ide. Analysis of these variables did not show a correlation between treatment and clinical evolution (p> 0.05).
Discussion
Based on the profile described for HDV patients living in the Amazon region, the individuals included in the study are young (mean age 47.7 years old) and mostly men (59.1%). Regarding the clinical presentation, there is already a consensus that patients with chronic Hepatitis Delta can remain stable, but that the majority present frequent hepatic decompensation events and quick progress to cirrhosis and HCC [6–12]. The reported results precisely show the pathogen's ability to cause severe liver infections, by demonstrating that 84.2% (n = 16) of the patients had the active disease and 42.1% (n = 8) had already evolved to liver cirrhosis. Levels of viral RNA have been previously described as predictive of cirrhosis and mortality [8,10,19,20], but there was no correlation between viral load and clinical progression of the patients included in this study. Possibly, the two parameters were not associated due to the introduction of treatments based on nucleos(t)ide analogs and interferon, which inhibit viral replication. Studies carried out to evaluate the effectiveness of this combination of drugs show that between 40% and 90% of patients have non-detectable viral load at the end of treatment 173 [21–25].
The difficulty in predicting events associated with clinical progression in HDV infection was demonstrated in the evaluation of noninvasive scores, which anticipate the occurrence of events in liver diseases. The FIB-4 and APRI indices are used to predict progression to fibrosis and liver cirrhosis in HCV and hepatic steatosis, but they did not present satisfactory results for the group of HDV patients evaluated.
The results demonstrate that it is extremely difficult to predict the behavior of HDV infection. This may be associated with genetic variability or with mechanisms involved in viral persistence and replication, which have not yet been fully elucidated. To date, the only tangible information is that HDV infection is more aggressive and the natural course of the disease is less severe in terms of contagion and the evolution of complications, when compared to other 184 hepatitises [5,8,10,20,26].
The implementation of therapeutic regimens improves the quality of life of chronic patients and can inhibit viral replication, but the drugs available are not specific for HDV and are not effective in preventing the development of CLD [6–9]. In this study, the patient who had the highest viral load in number of copies, which was 5059.5 copies/mL, evolved to death even after 3 years of treatment.
Conclusions
The study demonstrated that although infection by genotype 3 can lead to stable clinical conditions, the highest proportion of chronic carriers had frequent events of liver decompensation and progression to cirrhosis. The clinical status was in accordance with descriptions in the literature, but statistical analyses did not show a relationship between levels of viral RNA and pathogenesis, possibly due to the introduction of therapeutic regimens to inhibit viral replication.
The results show the difficulty in establishing noninvasive markers of liver damage but reinforce the consensus that HDV infection is more aggressive than other hepatitises. It was also possible to observe that the implementation of therapeutic regimens may reduce the viral load, but they are not enough to prevent the evolution of the disease.
Data availability: All data used to support the findings of this study are available in the text and can be solicited from the corresponding author.
Conflict of interest: The authors declare no potential Conflict of interest.
Funding statement: Coordenação de Aperfeiçoamento de Pessoal de Nível Superior-Capes, Brazil, and Instituto de Biologia Molecular do Paraná-IBMP, Brazil.
Acknowledgements: We thank group of virology molecular of Fiocruz in Rondônia, Brazil; Molecular Biology Institute of Paraná-IBMP, Brazil; and Research Center for Tropical Medicine – CEPEM, Porto Velho (RO), Brazil.
References
- Mentha N, Clément S, Negro F, Alfaiate D. A review on hepatitis D: From virology to new therapies. 2019.
- Fu TB, Taylor J. The RNAs of hepatitis delta virus are copied by RNA polymerase II in nuclear homogenates. J. Virol. 1993; 6: 6965–72, 1993.
- Lai MMC. RNA Replication without RNA-Dependent RNA Polymerase: Surprises from Hepatitis Delta Virus. J. Virol. 2005; 79: 7951–7958.
- Wedemeyer H. Hepatitis D revival. Liver Int. 2011; 31: 140–144.
- Romeo R. Hepatitis delta virus: Making the point from virus isolation up to 2014. World J. Hepatol. 2015;7: 2389.
- Alvarado-Mora MV, Romano CM, Gomes-Gouvêa MS, Gutierrez MF, Carrilho FJ, et al. Dynamics of Hepatitis D (delta) virus genotype 3 in the Amazon region of South America. Infect. Genet. Evol. 2011.
- Bensabath G, Hadler SC, Soares MCP, Fields H, Dias LB, Popper H, Maynard JE. Hepatitis Delta Virus Infection and Labrea Hepatitis: Prevalence and Role in Fulminant Hepatitis in the Amazon Basin.” JAMA J. Am. Med. Assoc. 1987.
- Romeo R, Foglieni B, Casazza G, Spreafico M, Colombo M, Prati D. “High serum levels of HDV RNA are predictors of cirrhosis and liver cancer in patients with chronic hepatitis delta.” PLoS One. 2014.
- Smedile A, Lavarini C, Farci P, Arico S, Marinucci G, et al. Epidemiologic Patterns Of Infection With The Hepatitis B Virus-Associated Delta Agent In 236 Italy. Am. J. Epidemiol. 1983; 117: 223–229.
- Romeo R, Del Ninno E, Rumi M, Russo A, Sangiovanni A, et al. A 28-Year Study of the Course of Hepatitis Δ Infection: A Risk Factor for Cirrhosis and Hepatocellular Carcinoma. Gastroenterology. 2009.
- Liao B, Zhang F, Lin S, He H, Liu Y, Zhang J, et al. Epidemiological, Clinical and Histological Characteristics of HBV/HDV Co-Infection: A Retrospective Cross-Sectional Study in Guangdong, 243 China.” PLoS One. 2014; 12.
- Fattovich G. Influence of hepatitis delta virus infection on morbidity and mortality in compensated cirrhosis type B. Gut. 2000; 46: 420–426.
- Farci P, Niro G. Clinical features of hepatitis D. Semin. Liver Dis. 2012.
- Casey JL, Brown TL, Colan EJ, Wignall FS, Gerin JL. A genotype of hepatitis D virus that occurs in northern South America. Proc. Natl. Acad. Sci. 2006.
- Gomes-Gouvêa MS, Soares MCP, Bensabath G, de CarvalhoMello IMVG, Brito EMF, et al. Hepatitis B virus and hepatitis delta virus genotypes in outbreaks of fulminant hepatitis (Labrea black fever) in the western Brazilian Amazon region.” J. Gen. Virol. 2009.
- Sterling RK, Lissen E, Clumeck N, Sola R, Correa MC, et al. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology. 2006; 43: 1317–1325.
- Wai C. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C.” Hepatology. 2003; 38: 518–526, 2003.
- Botelho-Souza L. Análise molecular do vírus da hepatite Delta: desenvolvimento de transcrição reversa-PCR em tempo real e Nested PCR-RFLP para quantificação egenotipagem viral. 2014.
- Alvarado-Mora MV, Locarnini S, Rizzetto M, Rebello Pinho JR. An update on HDV: Virology, pathogenesis and treatment. 2013.
- Sureau C, Negro F. The hepatitis delta virus: Replication and pathogenesis. J. Hepatol. 2016; 64: S102–S116, 2016.
- Wedemeyer H, Yurdaydìn C, Dalekos GN, Erhardt A, Çakaloğlu Y, et al. Peginterferon plus Adefovir versus Either Drug Alone for Hepatitis Delta. N. Engl. J. Med. 2011.
- Kabaçam G, Onder FO, Yakut M, Seven G, Karatayli SC, et al. Entecavir treatment of chronic hepatitis. D. Clin. Infect. Dis. 2012; 55: 645-50.
- Wedemeyer H, Yurdaydin C, Hardtke S, Caruntu FA, Curescu MG, et al. Peginterferon alfa-2a plus tenofovir disoproxil fumarate for hepatitis D (HIDIT-II): A randomised, placebo controlled, phase 2 trial. Lancet Infect. Dis. vol. 2019; 28119: 275-286.
- Borzacov LMP, de Figueiredo Nicolete LD, Souza LFB, dos Santos AO, Vieira DS, et al. Treatment of hepatitis delta virus genotype 3 infection with peg-interferon and entecavir.” Int. J. Infect. Dis. 2016.
- Chen GY, Su TH, Kao JH. Successful treatment of chronic hepatitis B and D with pegylated-interferon plus entecavir.” J. Formos. Med. Assoc. 2015.
- Niro GA, Smedile A, Ippolito AM, Ciancio A, Fontana R, et al. Outcome of chronic delta hepatitis in Italy: A long term cohort study.” J. Hepatol. 2010.