Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
Silent hypoxaemia in COVID-19: Journey through ICU
Ashani Ratnayake1; Prabhashini Kumarihamy2*; Sujeewa Gunaratne2; Hiranya Abeysinghe2; Sahan Perera2; Shirley Ekanayake3
1 Consultant Anaesthetist, Specialised COVID-19 Treatment Unit, Base Hospital, Teldeniya, Sri Lanka.
2 Consultant Physician, Specialised COVID-19 Treatment Unit, Base Hospital, Teldeniya, Sri Lanka.
3 Consultant Radiologist, Specialised COVID-19 Treatment Unit, Base Hospital, Teldeniya, Sri Lanka.
*Corresponding Author: Prabhashini Kumarihamy
Consultant Physician, Specialised COVID-19 Treatment
Unit, Base Hospital, Teldeniya, Sri Lanka.
Email: Prabhashinikumarihamy@yahoo.com
Received : Aug 05, 2021
Accepted : Sep 13, 2021
Published : Sep 20, 2021
Archived : www.jcimcr.org
Copyright : © Kumarihamy P (2021).
Citation: Ratnayake A, Kumarihamy P, Gunaratne S, Abeysinghe H, Perera S, et al. Silent hypoxaemia in COVID-19: Journey through ICU. J Clin Images Med Case Rep. 2021; 2(5): 1317.
Clinical image description
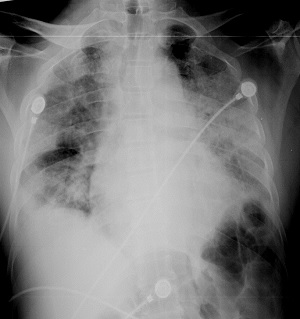
Silent hypoxia is a well-known entity associated with SARSCoV-2 [1,2]. It is a condition where despite the patient being hypoxic, they do not show any signs and symptoms of respiratory distress [2]. Hypoxia can only be detected either by pulse oximetry reading or through blood gas analysis. These patients may have variable radiological appearances on presentation. Many studies have shown silent hypoxia has a high incidence of 20-40% with patients with SARS-CoV-2 pneumonia [2,3]. Some patients need intensive care support and some recover without any supports. Here we present a series of chest radiographs of a patient presented with silent hypoxia. A previously well 53 year old male presented to a COVID-19 treatment facility with a positive antigen testing. At the time of admission, the patient was well with a respiratory rate of 16/min and stable haemodynamics. There were no other signs and symptoms of respiratory distress. His routine pulse oximetry reading was 66% with an arterial oxygen partial pressure of 56 mmHg. The first chest radiograph showed an extensive air space opacification (Figure 1). The appearance was so severe and did not match with his clinical picture. An entity of silent hypoxia was diagnosed, and he was admitted to the Intensive care unit and started on face mask oxygen through 60% venturi.
With an oxygen requirement as high as FiO2 of 80% with pressure support of 10 mmHg and PEEP of 7 mmHg, he remained comfortable and therefore Invasive ventilation was not considered. Weaning of oxygen therapy commenced after 6 days.
Figure 3 shows a Chest radiograph done on the 10th day in ICU showing improvement of air space opacification and commencement of the development of chronic lung changes. He had a total ICU stay of 16 days and was transferred to a respiratory unit for pulmonary rehabilitation. During the period of weaning, he had several episodes of silent hypoxia.
References
- Rahman A, Tabassum T, Araf Y, Al Nahid A, Ullah MA, et al. Silent hypoxia in COVID-19: pathomechanism and possible management strategy. Mol Biol Rep. 2021; 48: 3863-3869.
- Gopal AB, Chakraborty S, Padhan PK, Barik A, Dixit P, et al. Silent hypoxia in COVID-19: A gut microbiota connection,Current Opinion in Physiology. 2021.
- Busana M, Gasperetti A, Giosa L, Forleo GB, Schiavone M, et al. Prevalence and outcome of silent hypoxemia in COVID-19. Minerva Anestesiol. 2021; 87: 325-333.