Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
A rare case of plasmacytoma of mandible revealing plasma cell myeloma
Hari Ram1; Sneha Gupta2*; Praveen Kumar Singh2 ; Shivani Sharma2
1 Professor, Department of Oral and Maxillofacial Surgery, King George’s Medical University, Lucknow, India.
2 Junior Resident, Department of Oral and Maxillofacial Surgery, King George’s Medical University, Lucknow, India.
*Corresponding Author: Sneha Gupta
Department of Oral and Maxillofacial Surgery, King
George’s Medical University, Lucknow, India.
Email: gahens@gmail.com
Received : Aug 17, 2021
Accepted : Sep 13, 2021
Published : Sep 20, 2021
Archived : www.jcimcr.org
Copyright : © Gupta S (2021).
Abstract
Multiple myeloma (MM) is a malignant proliferation of plasma cells with multiple foci. Plasmacytoma is a solitary plasma cell neoplasm involving a single bone. The most commonly involved bone is vertebra. Jaw bones are rarely involved as a first bone as they have lesser hematopoietic marrow. A solitary plasmacytoma may progress to multiple myeloma within few months to year.
We present a case of a swelling of mandible that on further investigations confirmed the diagnosis of multiple myeloma. We have discussed the course of treatment given and its prognosis.
Keywords: multiple myeloma; plasmacytoma of jaw; bence jones Protein; abnormal plasma cells; CD138.
Citation: Ram H, Gupta S, Singh PK, Sharma S. A rare case of plasmacytoma of mandible revealing plasma cell myeloma. J Clin Images Med Case Rep. 2021; 2(5): 1319.
Introduction
Multiple myeloma also known as Kahler’s disease usually has a multifocal derivation within the bone. It contributes to about 15% of all hematologic malignancies and 1% of all malignancies [1,2]. There is a monoclonal multiplication of aberrant plasma cells in this disease that sequel from a single malignant predecessor that has undergone an uncontrolled mitotic division. Afterwards, either kappa or lambda type of immunoglobulin light chain is generated by these cells [3]. The most common site of involvement is the spine, vertebrae, femur, and pelvis and often occurs centrally within a bone [4,5]. A single bone when involved is termed as plasmacytoma and occasionally when a soft tissue is involved, it is termed as extamedullary plasmacytoma. A solitary plasmacytoma or extramedullary plasmacytoma has a better prognosis. On the other hand, a plasmacytoma when gets converted into myeloma, it has a poorer prognosis. About 12% to 15% of solitary plasmacytomas of the bone arise in the jaw and they frequently involve the posterior body, angle and ramus region of the mandible. The male to female ratio of solitary plasmacytoma 2: 1 and an average age of 55 years [6-8].
Case report
A 58 years old female visited our department of oral and maxillofacial surgery, complaining of a pain and swelling on the right side of the lower jaw for the past 4 months with on and off fever malaise and fatigue as well. The extraoral examination revealed facial asymmetry due to swelling over the right side of the face which was well defined extending supero-inferiorly below the ala tagus line to 1 cm below the lower border of mandible (Figure 1). Approximate dimension was 8 cm supero-inferiorly. Swelling extends antero-posteriorly from corner of commisure of lip to 1 cm anterior to posterior border of mandible. Overlying skin was normal in colour. Approximate dimension is 8.5 cm antero-posteriorly. On palpation it was hard, tender and fixed. Raised temperature was appreciated. Right Submandibular and submental lymph nodes were palpable, tender, mobile, and had an approximate dimension of 2 cm. The right mental nerve proved hypoesthetic with subjective intermittent ‘tingling’ reported. A step could be appreciated at the right lower boder of mandibular body region. Intraorally, swelling encompassing the left mandibular buccal & lingual vestibule and alveolar ridge was identified which was not crossing the midline (Figure 2). Swelling was approximately 5*2.5 cm in dimension, extending from 42 region to right retromolar pad region of mandible obliterating buccal and lingual vestibule region. Swelling was sessile. Overlying mucosa was friable, gelatinous and soft. Pain was elicited on palpation. Mobility of the mandibular jaw can be appreciated in two halves in relation to 44 region. Also, 44 was mobile.
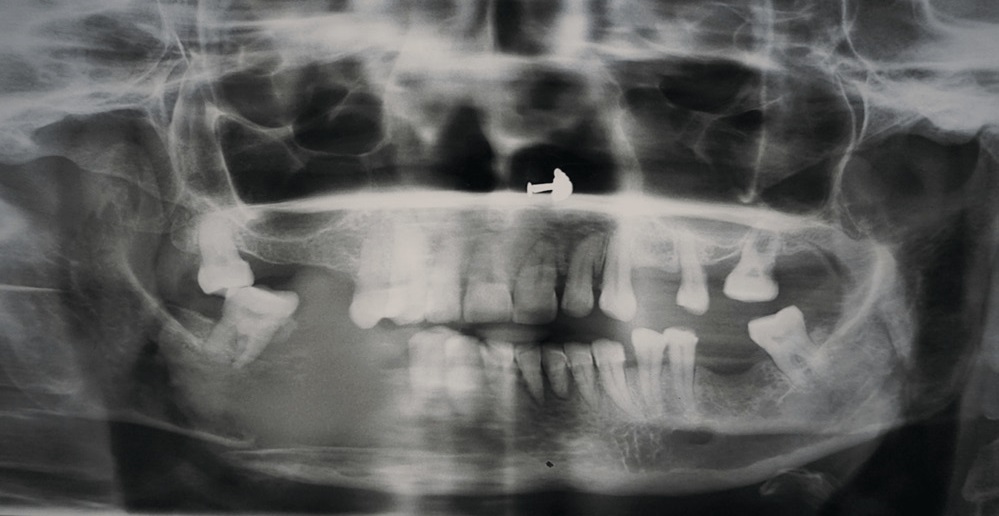
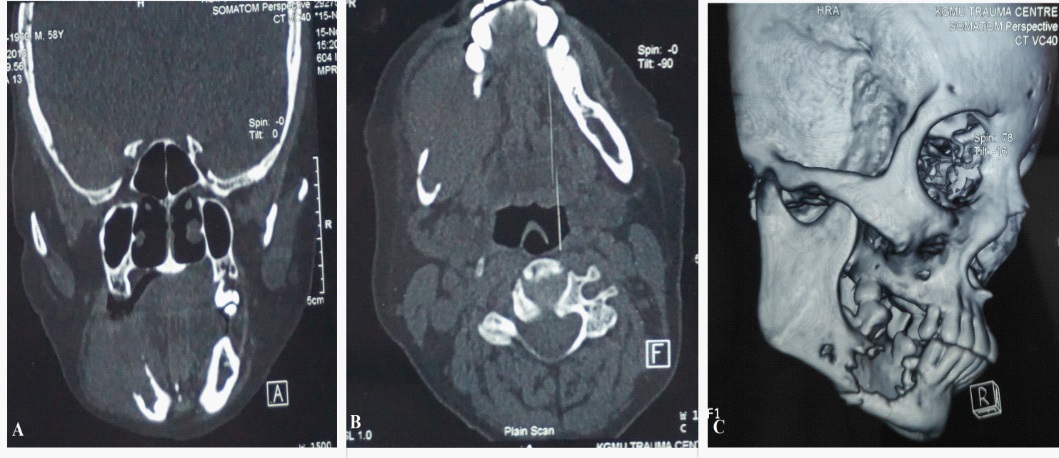
A panoramic radiograph revealed an ill-defined osteolytic radiolucent bony lesion involving the left mandibular body that is 46, 47 region with discontinuity in the lower border of mandible indicative of a pathological fracture (Figure 3). The computed tomography revealed an intense destruction of buccal and lingual cortical plates in the same region (Figure 4).
An incisional biopsy of the left mandibular body region was performed under local anaesthesia and specimen was sent for histopathological examination. The section showed that the biopsy tissue was lined by stratified squamous epithelium with dense diffuse infiltration of the underlying subepidermal zone by atypical Plasma cells disposed in form of sheets. Individual atypical cell had round nuclei with variably clumped chromatin, prominent nucleoli and moderate amount of cytoplasm. Many binucleted and multinucleated plasma cells and plasmablasts were also seen. On immunohistochemical analysis EMA, LCA and CD138 markers were positive. Weak focal cytoplasmic positivity for EMA marker, strong intensity, diffuse cytoplasmic positivity in for LCA marker and moderate intensity focal cytoplasmic positivity for CD138 markers in tumour cells was seen. CD20, CD99, CD19, CD3, Cytokeratin, Myeloperoxidase and Synaptophysin were not seen.
The patient was referred to clinical haematology department and a systemic work-up for the final diagnosis was performed to differentiate the solitary plasmacytoma of bone and multiple myeloma. In the hemogram we observed a decrease in concentration of haemoglobin, slight raise in urea, creatinine levels, an increased serum ionic calcium and positive C reactive protein.
A bone marrow examination, serum protein electrophoresis and whole body PET scan was advised to the patient. The bone marrow smear was particulate and mildly hypercellular for age. Megakaryocytes were adequate. Majority of the bone marrow nucleated cells were 62% abnormal plasma cells with eccentric nuclei with abundant amount of deep basophilic cytoplasm. Few binucleate form and few with prominent nucleoli (plasmablasts) were also seen. Granulocytic precursors (25%) showed normal maturation and morphology. Erythroid precursors (8%) were chiefly late normoblasts. Lymphocytes were mature in appearance. Bone marrow aspirate gave an impression of plasma cell myeloma. In serum protein electrophoresis no M band was seen.
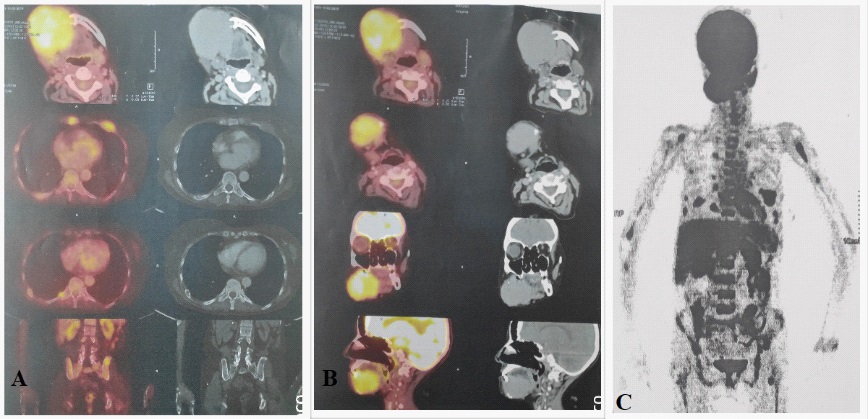
Whole body images were acquired in 3D mode 60 min after intravenous injection of 370MBq of 18 F-FDG using a dedicated LSO PET CT Scanner (Figure 4). Lytic destructive changes were noted in right hemimandible with large well defined homogeneously enhancing soft tissue mass (6.5*5.6*4.5 mm). The mass was abutting right hyoglossus with maintained fat plane. Anteriorly the lesion reaches up to skin. Multiple centimetric sized multiple bilateral cervical level IA, IB, II, III lymph nodes noted. Lytic changes were also noted in right scapula, right humerous (marrow), sternum, bilateral ribs with multiple soft tissue component in left 4th rib anteriorly, bilateral pelvic bone and bilateral femora, C6, S1 vertebra and multiple punched out lesions noted in entire calvaria. Diffuse marrow uptake was noted in visualized axial and appendicular skeleton. Diffuse osteoporosis was also noted. PET Scan gave an impression of an active stage of disease.
The patient was recommended for multiagent chemotherapy with Bortezomib, Thalidomide, Nandrolone, Aspirin, Zoledronate and weekly assessment of hemogram, kidney function test and serum ionic calcium level was done. There was an increment in the level of haemoglobin, improvement in kidney function test. The patient had accepted the chemotherapy well and is in good health until now (Figure 5).
Discussion
Multiple Myeloma is a malignant proliferation of abnormal plasma cells at multiple foci. Uncontrolled antibodies are secreted by these abnormal cells due to the chromosomal mutation. These antibodies are non functional and termed M protein. Most often they are of the IgG variety (50% of cases), with IgA being the 2nd most common at 25%. If untreated, symptoms may progress due to the high levels of circulating M protein. The body attempts to secrete the excess protein in the urine, with time causing renal failure. M protein is additionally deposited throughout the body as amyloid. Deposition of this protein in the bilateral tongue presents as firm nodules or swellings. They don’t require biopsy and can recur if excised. Hypercalcemia, hyperuricemia are an ominous sign. This is often a sign of advanced lytic bone lesions. Because the tumor cells proliferate within the bone marrow, they disrupt the normal hematopoiesis leading to a normocytic normochromic anemia. In end stage disease, it is kidney failure and infection that contribute most to a patient’s demise. The 5 year survival rate is stage dependent. In stage I beta 2 microglobin is 82% <3.5 mg/L, stage II 62%, stage III 40% (< 5.5 mg/dl). Prognostic factors include large tumor masses, anemia, rising beta 2 microglobin, and elevated creatinine [3].
In all the patients with a solitary plasmacytoma, a systemic examination should be done before the final diagnosis to rule out the presence of any systemic disease that may go undiagnosed. In the present case after the histopathological diagnosis of a solitary plasmacytoma, a thorough systemic examination, bone trephination, immunohistochemical analysis and a PET Scan was done to divulge the diagnosis as ‘plasma cell myeloma’
According to the criteria agreed on by the International Myeloma Working Group (IMWG) [9] our patient had symptomatic active myeloma as the patient had 68% plasma cells in the bone marrow, anemia, slightly raised urea, creatinine, uric acid, serum ionic calcium, multiple skeletal osteolytic destruction, generalized bone pain and a pathological fracture. Also, based on the Durie-Salmon [10] staging system of multiple myeloma our patient is in stage II of the disease with the above mentioned signs and symptoms.
After the initial diagnosis of multiple myeloma symptomatic type of chemotherapy was given with Bortezomib/thalidomide/ dexamethasone (category 1: NCCN guidelines for myeloma [11]) which is one of the preferred regimens. All patients receiving primary myeloma therapy should be given bisphosphonates (category 1: NCCN guidelines [11]) as an adjunct therapy. Bony manifestations of myeloma occur as disseminated osteopenia, osteolytic lesions. These complications lower the patients’ quality of life so by using bisphosphonates as an adjuct these complications are lowered [11]. Zoledronic acid is a potent bisphosphonate which was used by the haematologist in our patient but it has a risk of development of osteonecrosis of the jaw so our patient was surveyed weekly for renal function and monitored for osteonecrosis of the jaw as well.
NCCN guidelines [11] also says that an exposure to myelotoxic agents (including alkylating agents and nitrosoureas) can compromise the stem cell reserve before stem cell procurement in patients who possibly will be candidates for transplants. Stem cell therapy can be given as supportive therapy with high dose chemotherapy. Low-dose radiation therapy can be given as a palliative treatment for uncontrolled pain, imminent pathologic fracture, compression of spinal cord or vertebral instability. Radiation therapy should not preclude stem cell collection in potential candidates for stem cell therapy. Hypercalcemia should be treated with hydration and calcitonin. Plasmapheresis should be used as adjunctive therapy for treatment for renal dysfunction. Erythropoietin therapy should be considered for anemic patients particularly with renal failure. NSAIDs and IV contrast media should be avoided to decrease the chances of renal dysfunction.
A plasmacytoma when gets converted into myeloma, it’s a poorer prognosis so an early diagnosis is indispensable for the patient’s survival. A solitary bone plasmacytoma may advance to plasma cell myeloma at a rate of 65-84% in 10 years and 65- 100% in 15 years. The average time of beginning of transformation to myeloma is 2-5 years with a 10-year disease-free survival rate of 15-46% [12].
So putting in a nutshell, we have reported a case of a plasma cell myeloma who presented as a case of plasmacytoma of right side of mandible. Patient was thoroughly investigated and diagnosed as stage II multiple myeloma according to Durie-Salmon staging [10]. Patient was recommended multiagent chemotherapy with Bortezomib, Thalidomide, Nandrolone, Aspirin, Zoledronate and patient has responded well to the chemotherapy.
References
- Rajkumar SV, Dimopoulos MA, Palumbo A, et al. International Myeloma Working Group Updated Criteria for the Diagnosis of Multiple Myeloma. Lancet Oncol. 2014; 15: e538–e548.
- Rajkumar SV. Multiple myeloma: Update on diagnosis, risk-stratification, and management. Am J Hematol. 2014; 89: 998–1009.
- Mohan H. Essentials of Pathology 7th ed. New Delhi: Jaypee Brothers Medical Publishers (P) Ltd. 2015: 361-364
- Kilciksiz Sevil, Karakoyun-Celik Omur, Agaoglu Fulya Yaman, Haydaroglu Ayfer. A Review for Solitary Plasmacytoma of Bone and Extramedullary Plasmacytoma. The Scientific World Journal. 2012; 2012: 1–6.
- Purkayastha A, Sharma N, Suhag V, Lohia N. Extramedullary plasmacytoma of oral cavity: series of three unusual cases at unusual locations. Int J Oral Health Sc. 2017; 6: 26–29.
- Rodríguez-Caballero B, Sanchez-Santolino S, García-MontesinosPerea B, Garcia-Reija MF, Gómez-Román J, et al. Mandibular solitary plasmocytoma of the jaw: A case report. Medicina Oral, Patologia Oral y Cirugia Bucal. 2011; 16: e647–e650.
- Souza LN, Farias LC, Santos LAN, Mesquita RA, Martelli H, Jr., De-Paula AMB. Asymptomatic expansile lesion of the posterior mandible. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology. 2007; 103: 4–7.
- Bachar G, Goldstein D, Brown D, et al. Solitary extramedullary plasmacytoma of the head and neck-Long-term outcome analysis of 68 cases. Head and Neck. 2008; 30: 1012–1019.
- The International Myeloma Working G. Criteria for the classification of monoclonal gammopathies, multiple myeloma and related disorders: a report of the International Myeloma Working Group. Br J Haematol 2003; 121: 749–757.
- Durie BG, Salmon SE. A clinical staging system for multiple myeloma. Cancer 1975; 36: 842-854. Copyright © (1975) American Cancer Society. Reproduced with permission of John Wiley & Sons, Inc.
- Anderson KC, Alsina M, Bensinger W, Biermann JS, Khan AC, Cohen AD, et al. © JNCCN–Journal of the National Comprehensive Cancer Network. 2011; 9: 10.
- Caers J, Paiva B, Zamagni E, Leleu X, Bladé J, et al. Diagnosis, treatment, and response assessment in solitary plasmacytoma: updated recommendations from a European Expert Panel. J Hematol Oncol. 2018; 11: 10.