Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
Bilateral parotid gland enlargement as a presenting manifestation of relapsed pediatric acute myeloid leukemia
Akanksha Garg1; Priyanka Chauhan2; Anshul Gupta2; Soniya Nityanand2*
1 Department of Hematology, GCRI, Ahmedabad, Gujarat, India.
2 Department of Hematology, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, India.
*Corresponding Author: Soniya Nityanand
Professor, Department of Hematology, Sanjay Gandhi
Post Graduate Institute of Medical Sciences, Raebareli
Road, Lucknow - 226014, UP, India.
Email: nsoniya186@gmail.com
Received : Aug 24, 2021
Accepted : Sep 22, 2021
Published : Sep 29, 2021
Archived : www.jcimcr.org
Copyright : © Nityanand S (2021).
Abstract
Parotid gland involvement is a rare presentation of Acute Myeloid Leukemia (AML). We report a 10-year-old girl of acute myelomonocytic leukemia with normal cytogenetics and positivity for inversion 16, who after completion of first consolidation of the BFM 2004 AML protocol, presented with bilateral parotid gland enlargement. Bone marrow examination was suggestive of a relapse. Fine needle aspiration of the parotid gland showed presence of myeloblasts. Patient was given FLAG-IDA chemotherapy, with which the parotid swellings rapidly regressed and she achieved a remission and was planned for allogenic bone marrow transplantation. Acute myelomonocytic and monoblastic leukemias are known to be associated with tissue infiltration. However, exocrine gland involvement such as parotid enlargement is rare and is associated with a poor prognosis as was seen in our patient who despite having inversion 16 positivity had poor disease outcome.
Keywords: acute myeloid leukemia; parotid gland enlargement; granulocytic sarcoma.
Citation: Garg A, Chauhan P, Gupta A, Nityanand S. Bilateral parotid gland enlargement as a presenting manifestation of relapsed pediatric acute myeloid leukemia. J Clin Images Med Case Rep. 2021; 2(5): 1330.
Introduction
Acute Myeloid Leukemia (AML) in children accounts for a very small number of cases, incidence being 2-3 per 100,000 per annum [1]. The prevalence of relapsed AML in children is 24-40% [2]. Acute myelomonocytic (AML-M4) and monoblastic leukemia (AML-M5) are known causes for tissue infiltration. Moreover, exocrine gland involvement such as parotid enlargement is very rare. Parotid gland enlargement presenting as a Granulocytic Sarcoma (GS) / Myeloid Sarcoma (MS) in relapsed pediatric AML is rarely reported. We report a case of a relapsed pediatric AML with bilateral parotid enlargement.
Case report
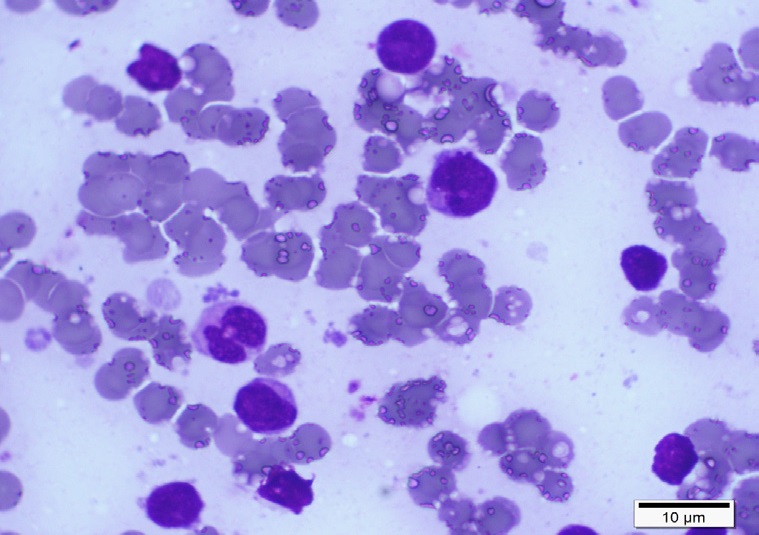
A 10-year old girl of AML-M4 with normal cytogenetics and positivity for inversion 16 (inv (16)) presented with isolated bilateral, painless parotid gland enlargement (Figure 1a) 26 days after completion of the 1st consolidation of the BFM 2004 AML protocol. There was no fever, organomegaly, evidence of any cranial nerve palsy including facial nerve palsy or CNS involvement. Her haemoglobin was 11.6 g/dL, Total Leucocyte Count was 11.7 x 106/L, and platelet count was 63 x 109/L. Though our first differential diagnosis was mumps, but the absence of fever, pain, and tenderness of the parotid glands, prompted us to investigate for any relapse of the disease. Bone marrow examination confirmed a relapse with presence of 80-90% myeloblasts. Fine needle aspiration of the parotids showed presence of myeloblasts (Figure 1b). CSF examination did not reveal presence of any malignant cells. KIT mutation analysis was done and found to be negative. Patient was given 1st cycle of FLAGIDA chemotherapy, with which the parotid swellings rapidly regressed in size and a remission was achieved. An HLA typing of the family was performed and a 10/10 match was identified in her brother. While the family was arranging finances for the transplant, a second course of FLAG-IDA chemotherapy was administered. However, within a month following the second course she relapsed, this time with complaints of decreased vision in the left eye with diplopia. Physical examination revealed recurrence of the bilateral parotid enlargement and left lateral rectus palsy. CSF cytology was positive for malignant cells. The patient’s family opted for no further therapy and thereafter were lost to follow up.
Discussion
Both AML- M4 and M5 are known to be associated with tissue infiltration in the form of swollen gums, myeloid sarcomas, and skin nodules [8]. However, parotid enlargement is very rare. Myeloid Sarcoma (MS) is composed of myeloblasts, occurring in extramedullary sites in AML. It is more common in the pediatric age group with an incidence of up to 30% in some studies of pediatric AML patients versus 2–5% in adults [3]. It can be present both at the time of initial diagnosis of AML as well as at the time of disease recurrence [4]. Common sites are bone, periosteum, soft tissues, lymph nodes, and skin, but have also been reported in the gastrointestinal tract, testes, breast, cervix, vagina, salivary glands, mediastinum, pleura, and peritoneum. Neiman et al reviewed 61 biopsies of MS and only 1 patient had salivary gland involvement [5]. In a case series of 131 patients with MS, most common site was lymph node followed by skin. The rare sites were bladder, breast, thyroid, and pancreas, but none of the patients had parotid involvement [6]. Majority of patients in these studies were adults. In a case series by Claerhout et al, one case each of CNS and orbital MS have been described in pediatric patients [7]. However, no case of parotid MS as seen in our patient was described.
In adults, parotid gland involvement as a presenting manifestation has been reported in newly diagnosed AML [12], newly diagnosed T-cell leukemia [13], and lymphoma [14]. Parotid gland enlargement as the presenting manifestation of pediatric AML is even rarer, with only a few case reports. Geetha et al reported a case of a 14-year-old girl with bilateral parotid gland enlargement as initial manifestation of AML [9]. Naithani et al reported a case of left side parotid gland enlargement in a newly diagnosed pediatric AML [8]. Both these cases expired during their treatment.
The parotid gland has been described as a site of extramedullary relapse in adults with Acute Lymphoblastic Leukemia (ALL) and AML [10,11]. Parotid gland has been a sanctuary site for relapsed acute leukemia either in isolation or in association with central nervous system [9,15]. Factors predisposing extramedullary relapse in AML include an abnormal karyotype (e.g., t (8; 21), inv (16) and t(11q23)), FAB type M4, M5 morphologies, and strong male predominance [16,17].
KIT gene mutations in adult and pediatric AML patients with t (8;21) and in adult AML patients with inv (16) have been associated with a poorer prognosis than in those without KIT gene mutations. However, the frequency and clinical impact of KIT gene mutations in pediatric AML patients with inv (16) remain unknown. Pediatric AML patients with inv (16) have been reported to represent 3.4% to 6% of the total number of pediatric AML patients [18]. Thus, the number of pediatric AML patients with KIT mutations is likely to be very small. Although our patient had favorable inv (16) mutation and did not demonstrate KIT mutations, her disease relapsed, and she demonstrated parotid enlargement as extramedullary disease. Further, she became refractory to chemotherapy and developed CNS involvement also.
Recently, Caraffini et al, described RAF Kinase Inhibitor Protein (RKIP) as a negative regulator of RAS-MAPK/ERK signaling. A somatic loss of RKIP has recently been described as a frequent event in AML [19]. It has been shown to be associated with monocytic AML phenotypes and proven to be of functional relevance for leukemogenesis. They demonstrated that RKIP is indeed involved in the tissue infiltration of leukemic blasts and, consequently, in the formation of MS. However, this testing was not done in our patient at that time. It is likely that in the future, further such molecular markers would be discovered which could explain poor clinical outcomes in pediatric patients with inv (16) AML.
Conclusion
To conclude, bilateral parotid enlargement as a presenting manifestation of relapsed childhood AML has not been reported, but our case demonstrates that if present should prompt investigations for relapse of AML. Such patients have a poor prognosis as also highlighted by our case who despite having inv (16) and absence of KIT mutations had a chemotherapy resistant disease. Newer molecular mutations could be unveiled soon explaining the poor prognosis in pediatric patients of AML with inv (16) mutation.
Conflict of interest: The authors of this manuscript have no conflicts of interest to declare.
Author contribution: All authors had full access to the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Conceptualization, A.G., and P.C.; Methodology, A.G, S.N.; Investigation, P.C, S.Y; Formal Analysis, A.G, P.C.; Resources, S.Y.; Writing - Original Draft, A.G, P.C.; Writing - Review & Editing, A.G, S.N.; Visualization, A.G.; Supervision, A.G.
Data availability statement: Data sharing is not applicable to this article as no new data were created or analyzed in this study.
References
- Hoffbrand VA, Catovsky D, Tuddenham E. Post graduate Hematology, 7th edition, 2016.
- Rubnitz JE.How I treat pediatric acute myeloid leukemia, Blood. 2012; 119: 5980-5988.
- Byrd JC, Edenfield WJ, Shields DJ, Dawson NA. Extramedullarymyeloid cell tumors in acute nonlymphocytic leukemia: a clinical review. Journal of Clinical Oncology. 1995; 13: 1800–1816.
- Koc Y, Miller KB, Schenkein DP, Daoust P, Sprague K, Berkman E. Extramedullary tumors of myeloid blasts in adults as a pattern of relapse following allogeneic bone marrow transplantation. Cancer. 1999; 85: 608–615.
- Neiman RS, Barcos M, Berard C, Bonner H, Mann R, Rydell RE, Bennett JM. Granulocytic sarcoma: a clinicopathologic study of 61 biopsied cases. Cancer. 1981; 48: 1426–1437.
- Keisuke Kawamoto, Hiroaki Miyoshi, Noriaki Yoshida, Jun Takizawa, Hirohito Sone and Koichi Ohshima. Clinicopathological, Cytogenetic, and Prognostic Analysis of 131 Myeloid Sarcoma Patients Am J SurgPathol. 2016; 40: 1473–1483.
- Helena Claerhout, Sophie Van Aelst, Celine Melis, Thomas Tousseyn, Olivier Gheysens, Peter Vandenberghe, DaanDierickx, and Nancy Boeckx. Clinicopathological characteristics of de novo and secondary myeloid sarcoma: A monocentric retrospective study. doi: 10.1111/ejh.13056.
- Naithani R, Mahapatra M; Parotid involvement in Acute Myelomonocytic Leukemia, Ind J Paed. 2007: 965.
- Geetha N, Kusumakumary P, Abraham E, et al. An uncommon presentation of acute nonlymphocytic leukemia: a case report. Pediatr Hematol Oncol. 1998; 15: 75–79.
- Rhee D, Myssiorek D, Zahtz G, et al. Recurrent attacks of facial nerve palsy as the presenting sign of leukemic relapse. Laryngoscope. 2002; 112: 235–237.
- Mesa JR, Espinosa E, Losada R, et al. Parotid and central nervous system relapse during complete hematologic remission in acute promyelocytic leukemia. Haematologica. 1999; 84: 565–566.
- Sood BR, Sharma B, Kumar S, et al. Facial palsy as first presentation of acute myeloid leukemia. Am J Hematol. 2003; 74: 200– 201.
- Obama K, Saito M, Higuchi I, et al. Adult T-cell leukemia predominantly involving exocrine glands. Eur J Haematol. 2004; 73: 332–339.
- Stritzky M, Wereldsma JC, Pegels JG. Parotid mass as first symptom of a malignant lymphoma. J SurgOncol. 1998; 67: 25–27.
- Ito T, Ishikawa Y, Noda M, Hattori T, Okano S. Isolated parotid relapse following bone marrow transplantation for acute myeloblastic leukemia; a case report. Nippon Ketsueki Gakkai Zasshi 1998; 21: 1031-36.
- Clark WB, Strickland SA, Barrett AJ, Savani BN. Extramedullary relapses after allogeneic stem cell transplantation for acute myeloid leukemia and myelodysplastic syndrome. Haematologica. 2010; 95: 860–3.
- Vega-Ruiz A, Faderl S, Estrov Z, Pierce S, Cortes J, Kantarjian H, et al. Incidence of extramedullary disease in patients with acute promyelocytic leukemia: a single-institution experience. Int J Hema- tol. 2009; 89: 489–96.
- Shimada A, Taki T, Tabuchi K, et al. KIT mutations, and not FLT3 internal tandem duplication, are strongly associated with a poor prognosis in pediatric acute myeloid leukemia with t(8;21): A study of the Japanese Childhood AML Cooperative Study Group. Blood. 2006; 107: 1806-1809.
- Caraffini V, Perfler B, Berg J, Uhl B, Schauer S, et al. Loss of RKIP is a frequent event in myeloid sarcoma and promotes leukemic tissue infiltration. Blood. 2018; 13: 826-830.