Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
Chiari I malformation and Noonan’s syndrome: Shared manifestations of RASopathy
Megan Still; Patricia Miller; William Dodd; Rachel Moor; Brandon Lucke-Wold; Ken Porche; Kelly Foote*
Department of Neurosurgery, University of Florida, Gainesville, USA.
*Corresponding Author: Kelly Foote
Professor, Department of Neurosurgery, University of
Florida, Gainesville.
Email: Kelly.Foote@neurosurgery.ufl.edu
Received : Aug 27, 2021
Accepted : Sep 23, 2021
Published : Sep 30, 2021
Archived : www.jcimcr.org
Copyright : © Foote K (2021).
Abstract
Neurologic sequalae of Noonan syndrome have been postulated in the literature. A topic of significance is the role of RASopathy in the shared pathophysiology of Noonan Syndrome and Chiari I malformation. In this unique case report, we present a patient with concomitant Noonan Syndrome and Chiari I with 4th ventricular outflow obstruction. The case highlights the importance of close clinical suspicion in this patient population. We utilize the case to delve into intricacies of the known pathophysiology and encourage ongoing investigation.
Keywords: Noonan syndrome; Chiari I malformation; RASopathy.
Citation: Foote K, Still M, Miller P, Dodd W, Moor R, et al. Chiari I malformation and Noonan’s syndrome: Shared manifestations of RASopathy. J Clin Images Med Case Rep. 2021; 2(5): 1334.
Introduction
Noonan syndrome (NS) is a clinically diagnosed disorder of development affecting approximately 1 in 2000 live births [1,2]. Congenital abnormalities associated with NS have been reported in multiple organ systems, the most common of which include craniofacial and skeletal malformations, cardiopulmonary anomalies, and various coagulopathies [3]. Neurologic symptoms are relatively uncommon [1]. Noonan syndrome is classified as a RASopathy as all known etiologic mutations affect the RAS/MAPK signaling pathway, which regulates cell growth, differentiation, migration, and repair [4]. Though NS is generally not life-threatening, especially in the absence of cardiac defects, investigation into clinical signs and various associated pathologies is important for early detection and optimal management.
The phenotypic spectrum of reported NS-associated abnormalities is ever-growing due to the wide-ranging effects of RAS/ MAPK disturbances. One of the most common genetic abnormalities in NS is a mutation in the PTPN gene, a part of the RAS/ MAPK pathway, which has also been linked to Chiari I malformation (CIM) [5,6]. Here we describe a patient presenting with both NS and Chiari I Malformation (CIM). CIM, defined as herniation of the cerebellar tonsils through the foramen magnum, has become more readily diagnosed due to increasing accessibility of MRI studies [7]. At the University of Florida, out of the 467 patients treated for Chiari malformation and 162 for Noonan syndrome (and other congenital disorders of short stature) since 2015, this is the only patient evaluated who had concurrent diagnoses of both. Reports of concurrent NS and CIM are also rare in the literature. The first case was reported in 1982 [8], and only six additional cases have been reported since 2001 [9-14]. While an exact pathogenic link between the two syndromes remains to be fully understood, a retrospective cohort study found that approximately one-quarter of children with CIM harbor a RAS/MAPK-related mutation [15]. Establishing a link between RASopathies like NS and CIM may help facilitate early recognition and diagnostic workup of associated genetic syndromes for clinicians treating patients with Chiari malformations. Similarly, such a link may encourage physicians treating those with NS to begin incorporating surveillance neuroimaging into their standard of practice, especially in patients with confirmed RASopathies, or neurologic symptoms that could be consistent with CIM. In this report, we describe the characteristics, clinical evaluation, and surgical intervention of a patient with NS and CIM, discuss how this case fits into the existing literature, and consider how CIM as a feature of NS might be empirically validated.
Case report
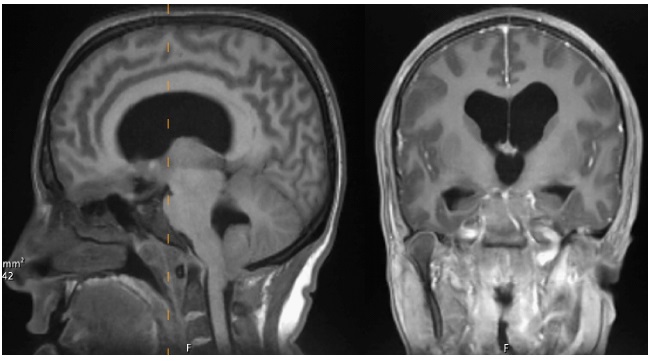
A 22-year-old woman with known NS presented to an outside hospital with unrelenting headaches. The headaches became intractable, and she was transferred to our institution for further management. Other reported symptoms included balance disturbance, intermittent numbness in her hands, and neck stiffness that had been ongoing for 3 weeks. She denied toxic habits and her only other past surgical history was correction of strabismus. Head computed tomography (CT) was obtained showing CIM and ventriculomegaly. Follow-up magnetic resonance imaging (MRI) was subsequently obtained (Figure 1).
After discussion with the patient and family, the patient elected to proceed with suboccipital craniectomy and expansion duraplasty for Chiari decompression with placement of an external ventricular drain (EVD). In the operating suite, a right frontal EVD was placed and the patient was then rotated into prone position. The case proceeded in the usual fashion with a midline suboccipital craniectomy, C1 laminectomy, and a Y-shaped dural opening. The cerebellar tonsils were carefully elevated to reveal a membrane occluding the 4th ventricular outflow at the foramen of Magendie. A generous fenestration of this membrane resulted in high flow egress of cerebrospinal fluid. An expansion duroplasty was then completed by sewing in a watertight, shield-shaped bovine pericardial graft covered with a thin layer of polyethylene glycol hydrogel and a single layer of dry gelatin sponge. The wound was closed in layers, and the patient was transferred to the intensive care unit (ICU).
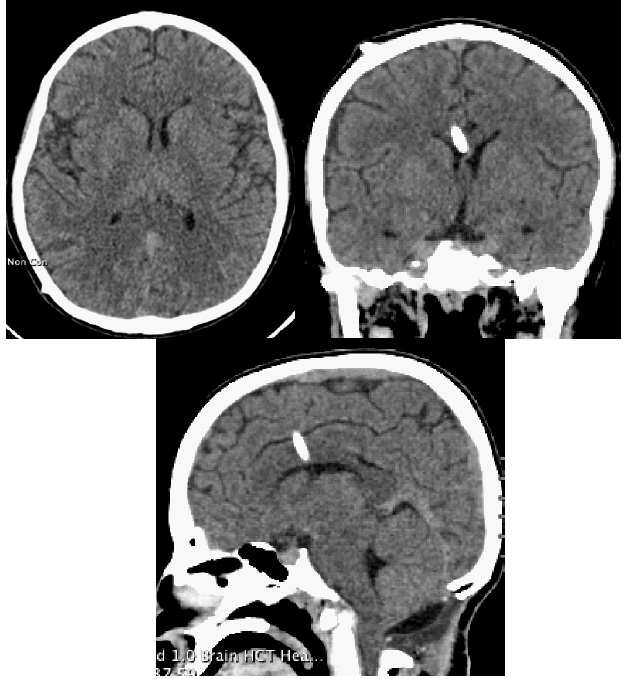
On post-op day one, her mental status declined and the EVD flow was noted to be sluggish. Head CT revealed an EVD tract hemorrhage with intraventricular hematoma (IVH). The Clear trial protocol was initiated with intraventricular tissue plasminogen activator (tPA) and a left-sided EVD was placed at bedside [16]. Clearance of the IVH was ultimately successful, but she failed a trial of EVD weaning and eventually required placement of a Ventriculoperitoneal Shunt (VPS). She was discharged to a rehabilitation center and has since made an excellent neurologic recovery. At her 2-month follow-up appointment, her headaches had significantly improved, the numbness in her hands had completely resolved, and she has had no further problems with balance, memory, or concentration. Surveillance head CT at that time showed resolution of ventriculomegaly, successful Chiari decompression, and interval right VPS placement (Figure 2).
Discussion
NS is a common disorder that presents with varying phenotypes and ranging severity. Multiple conditions unrelated to the diagnostic findings of NS appear to have a much higher incidence in this population. These include depression, scoliosis, chronic back pain, and lymphedema, in addition to CIM [5]. Additionally, there are reports of CIM in other disorders of the RAS/MAPK pathway, including LEOPARD syndrome, CFC syndrome, Costello syndrome, and neurofibromatosis type 1 [14,17-20]. In each of these reports, the incidence of CIM was less than 50%, but higher than the estimated prevalence in the general population (less than 1% or approximately 3.5% on radiographic findings) [21]. Due to the relative rarity of concomitant findings, it is challenging to determine if the relationship is incidental or causal. Thus, it is imperative to continue to report instances of these syndromes occurring simultaneously in order to support investigation, as well as to determine if there are common features among patients with both these findings. As genetic testing develops for RASopathy, the role in early diagnosis will become more important.
The pathophysiology of CIM is not well understood, but possible etiologies include genetic mutations and downward pressure from cranial constriction. These features are commonly found in patients with NS, especially those with significant craniofacial abnormalities [12]. One of the most common genetic mutations found in NS is a mutation of the PTPN gene, which tends to affect the face and jaw preferentially [12]. Mutations of this gene have been found in two patients with diagnoses of concurrent NS and CIM reported in the literature [13]. The proposed pathophysiology is alteration in the RAS/MAPK pathway [13]. There is also a very high incidence of Chiari malformations found in patients with craniosynostosis, lending possible support to the supposition that craniofacial abnormalities can cause progressive elevations in intracranial pressure and subsequent downward pressure [22].
Though there is not currently enough data to describe Chiari I malformation as a common phenotype of Noonan syndrome, this potential connection is important because patients with RASopathies as the source of NS may be more susceptible to CIM. Based on these observations, we suggest that a thorough neurologic evaluation of persons with NS be performed on a regular basis and if any suggestive neurologic symptoms or signs develop, early brain imaging should be obtained in order to detect CIM prior to the development of significant neurologic deficits or hydrocephalus. Furthermore, surgical intervention with suboccipital craniectomy, C1 laminectomy, and duroplasty has been demonstrated to be a successful treatment for symptoms caused by brainstem compression due to Chiari malformation in patients with Noonan syndrome.
References
- Roberts AE, Allanson JE, Tartaglia M, Gelb BD. Noonan syndrome. Lancet. 2013; 381: 333-342.
- Allen MJ, Sharma S. Noonan Syndrome. In: StatPearls. Treasure Island. 2021.
- Myers A, Bernstein JA, Brennan ML, et al. Perinatal features of the RASopathies: Noonan syndrome, cardiofaciocutaneous syndrome and Costello syndrome. Am J Med Genet A. 2014; 164A: 2814-2821.
- Tidyman WE, Rauen KA. The RASopathies: developmental syndromes of Ras/MAPK pathway dysregulation. Curr Opin Genet Dev. 2009; 19: 230-236.
- Smpokou P, Tworog-Dube E, Kucherlapati RS, Roberts AE. Medical complications, clinical findings, and educational outcomes in adults with Noonan syndrome. Am J Med Genet A. 2012; 158A: 3106-3111.
- Mitsuhara T, Yamaguchi S, Takeda M, Kurisu K. Gowers’ intrasyringeal hemorrhage associated with Chiari type I malformation in Noonan syndrome. Surg Neurol Int. 2014; 5: 6.
- McClugage SG, Oakes WJ. The Chiari I malformation. J Neurosurg Pediatr. 2019; 24: 217-226.
- Peiris A, Ball MJ. Chiari (type 1) malformation and syringomyelia in a patient with Noonan’s syndrome. J Neurol Neurosurg Psychiatry. 1982; 45: 753-754.
- Han Y, Chen M, Wang H. Chiari I malformation in patients with RASopathies. Childs Nerv Syst. 2021; 37: 1831-1836.
- Holder-Espinasse M, Winter RM. Type 1 Arnold-Chiari malformation and Noonan syndrome. A new diagnostic feature? Clin Dysmorphol. 2003; 12: 275.
- Colli R, Colombo P, Russo F, Sterpa A. [Type 1 Arnold Chiari malformation in a subject with Noonan syndrome]. Pediatr Med Chir. 2001; 23: 61-64.
- Keh YS, Abernethy L, Pettorini B. Association between Noonan syndrome and Chiari I malformation: a case-based update. Childs Nerv Syst. 2013; 29: 749-752.
- Ejarque I, Millan-Salvador JM, Oltra S, Pesudo-Martinez JV, Beneyto M, Perez-Aytes A. [Arnold-Chiari malformation in Noonan syndrome and other syndromes of the RAS/MAPK pathway]. Rev Neurol. 2015; 60: 408-412.
- Reinker KA, Stevenson DA, Tsung A. Orthopaedic conditions in Ras/MAPK related disorders. J Pediatr Orthop. 2011; 31: 599- 605.
- Saletti V, Vigano I, Melloni G, Pantaleoni C, Vetrano IG, Valentini LG. Chiari I malformation in defined genetic syndromes in children: are there common pathways? Childs Nerv Syst. 2019; 35: 1727-1739.
- Hanley DF, Lane K, McBee N, et al. Thrombolytic removal of intraventricular haemorrhage in treatment of severe stroke: Results of the randomised, multicentre, multiregion, placebocontrolled CLEAR III trial. Lancet. 2017; 389: 603-611.
- Beier AD, Barrett RJ, Burke K, Kole B, Soo TM. Leopard syndrome and Chiari type I malformation: a case report and review of the literature. Neurologist. 2009; 15: 37-39.
- Santoro C, Pacileo G, Limongelli G, et al. LEOPARD syndrome: clinical dilemmas in differential diagnosis of RASopathies. BMC Med Genet. 2014; 15: 44.
- Gripp KW, Hopkins E, Doyle D, Dobyns WB. High incidence of progressive postnatal cerebellar enlargement in Costello syndrome: brain overgrowth associated with HRAS mutations as the likely cause of structural brain and spinal cord abnormalities. Am J Med Genet A. 2010; 152A: 1161-1168.
- Miraglia E, Fabbrini G, Di Biasi C, et al. Chiari type 1 malformation in Neurofibromatosis type 1: experience of a center and review of the literature. Clin Ter. 2016; 167: e6-10.
- Langridge B, Phillips E, Choi D. Chiari Malformation Type 1: A Systematic Review of Natural History and Conservative Management. World Neurosurg. 2017; 104: 213-219.
- Cinalli G, Spennato P, Sainte-Rose C, et al. Chiari malformation in craniosynostosis. Childs Nerv Syst. 2005; 21: 889-901.