Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
Deteriorating cardiac function in patients with chronic total occlusion after successful percutaneous coronary intervention: A case series
Xueyao Yang1#; Jinfan Tian1#; Mohammad Sharif Popal2; Lijun Zhang3; Yi He4; Xiantao Song1*
1 Department of Cardiology, Beijing Anzhen Hospital, Capital Medical University, Beijing, China, 100029.
2 Department of Cardiac Surgery, Beijing Anzhen Hospital, Capital Medical University, Beijing, China, 100029.
3 Department of Radiology, Beijing Anzhen Hospital, Capital Medical University, Beijing, China, 100029.
4 Department of Radiology, Beijing Friendship Hospital, Capital Medical University, Beijing, China, 100050.
*Corresponding Author: Xiantao Song
Department of Cardiology, Beijing Anzhen Hospital,
Capital Medical University, Anzhen Road, Chaoyang
District, Beijing, 100029, China.
Email: songxiantao0929@qq.com
Received : Aug 05, 2021
Accepted : Sep 24, 2021
Published : Oct 01, 2021
Archived : www.jcimcr.org
Copyright : © Song X (2021).
Abstract
Background: Current trials show conflicting results about the effect of successful Percutaneous Coronary Intervention (PCI) on cardiac function in patients with chronic total occlusion (CTO). Various factors contribute to a lack of functional changes after CTO revascularization.
Case summary: Here, we present three patients who underwent PCI to treat CTO of the single main branch, all of whom demonstrated a decline in cardiac function detected by Cardiovascular Magnetic Resonance (CMR). Case 1 is a patient with a history of smoking, and transmural myocardial necrosis in the territory of the CTO at baseline. Case 2 exhibites hyperglycemia and persistent ischemia in a non-CTO-supplied territory. Case 3 has a long history of alcohol abuse, likely causing adverse ventricle remodeling after PCI.
Discussion: The deterioration observed in these cases does not appear to be associated with the PCI itself. It should be considered that postoperative risk factors attenuate the true benefits of CTO revascularization. This case series also highlights the prudent selection of patients eligible for revascularization by comprehensive assessments and recommends continuous strict management during follow-up to improve the long-term prognosis of patients and the application value of CTO revascularization.
Keywords: chronic total occlusion; percutaneous coronary intervention; cardiac function; adverse ventricle remodeling; cardiovascular magnetic resonance imaging
Citation: Song X, Yang X, Tian J, Popal MS, Zhang L, et al. Deteriorating cardiac function in patients with chronic total occlusion after successful percutaneous coronary intervention: A case series. J Clin Images Med Case Rep. 2021; 2(5): 1337.
Introduction
Current guidelines recommend percutaneous revascularization of Chronic Total Occlusion (CTO) when symptoms are persistent or ischemia is evident in the territory of the occluded vessel [1]. However, optimal CTO treatment is still controversial considering the difficulty of the procedure and the ambiguous benefits it provides. Observational studies suggest that successful revascularization of CTO is associated with improved cardiac function and lower cardiac mortality [2-4]. However, recent trials do not demonstrate any superior effect of Percutaneous Coronary Intervention (PCI) over Optimal Medical Therapy (OMT) on cardiac function in patients with CTO [5-7].
Indeed, in our clinical practice, we observed improvement of Left Ventricular (LV) systolic function and remodeling after successful CTO PCI in many patients. However, a few patients had deteriorative cardiac function. We speculate that deteriorating cardiac function in these patients could attenuate the beneficial effect of CTO revascularization observed in the overall population. Here, we present three cases of patients with deteriorating functional changes one year after successful CTO PCI and discuss the possible reasons for their decline in functionality. Accordingly, we aim to uncover important factors previously neglected in the treatment and management of CTO.
Patients included in this case series were derived from a prospective, registered study that investigated the effects of successful PCI on CTO (supported by Capital Health Development Research Project No. 2018-2-2063). The protocol was approved by the ethics committee of Beijing Anzhen Hospital, Capital Medical University. All patients with CTO lesions eligible for PCI underwent CMR examination both before and one year after the interventional procedure.
Case presentation
Case 1
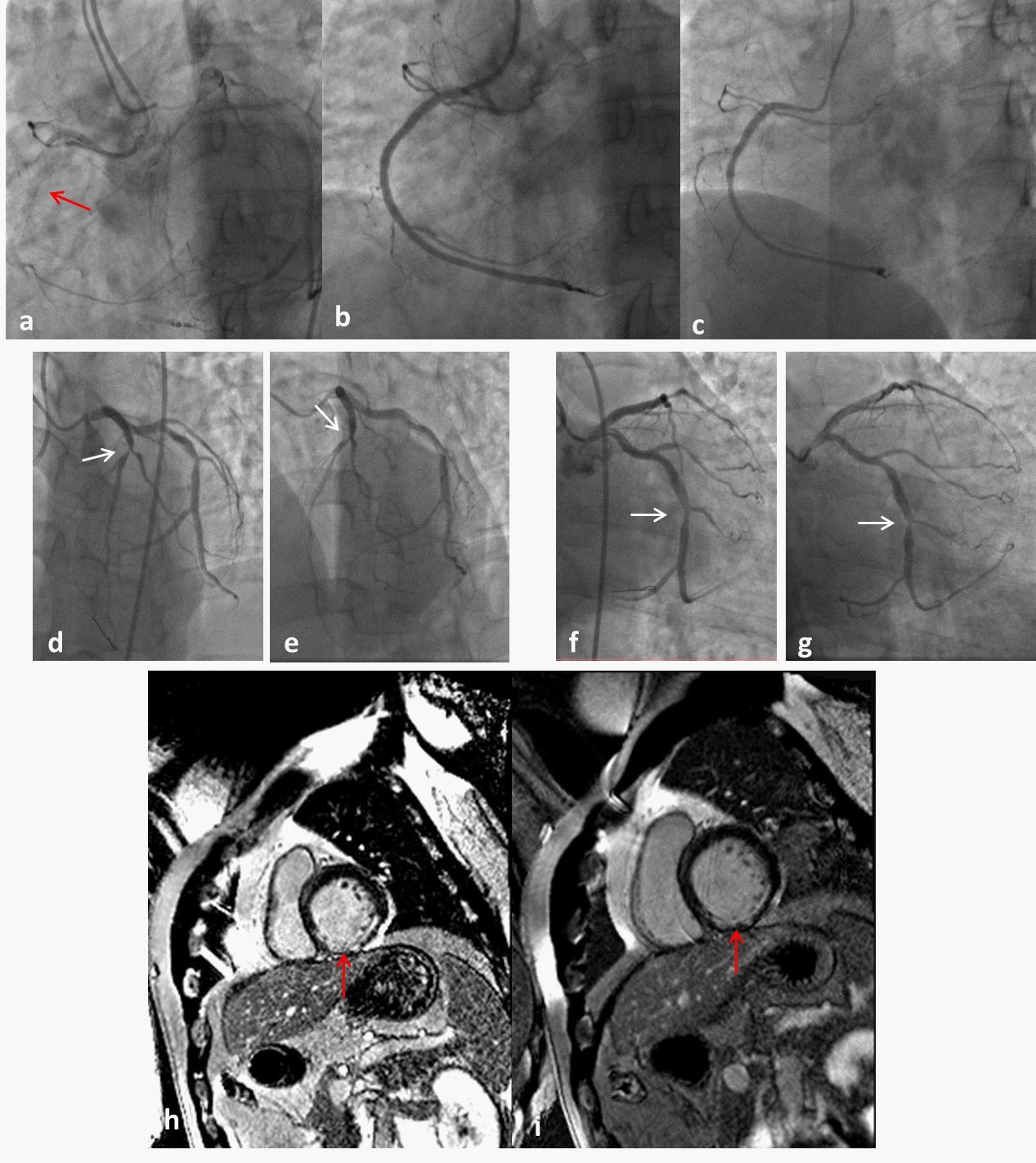
A 49-year-old man presented with recurrent effort angina for one year. He suffered an acute inferior myocardial infarction ten years ago and was treated with thrombolytic therapy within one hour of the event, followed by a left circumflex (LCX)-PCI eight days later. He then adhered to OMT. However, he did not quit smoking and his blood glucose levels remained uncontrolled. Angiography revealed right coronary artery (RCA)-CTO with Rentrop 3 grade collaterals from the left anterior descending (LAD) artery (Figure 1a), and 50-60% stenosis in both the proximal LAD and the middle LCX (Figure 1d, 1f). Using an antegrade approach, a PILOT 150 guidewire successfully passed through the CTO lesion without difficulty. Then, we performed a balloon dilation with a 2.5 X 20 mm B. Braun balloon and deployed one 3.5 X 28 mm Boston Promus Element stent, followed by a postdilatation Boston Quantum Maverick balloon measuring 3.75 X 10 mm. A Thrombolysis In Myocardial Infarction (TIMI) with grade 3 blood flow was observed in the RCA after the PCI procedure (Figure 1b).
Follow-up
During follow-up, the patient maintained satisfactory blood glucose levels by using oral antidiabetic agents. However, he failed to quit smoking. During his one year follow-up appointment, coronary angiography showed advanced stenosis in the LAD and LCX arteries (Figure 1e, 1g) with no obvious de novo stenosis in the RCA (Figure 1c). Both the LAD and LCX lesions were treated by PCI. According to CMR results, LVEF declined from 61.87% to 55.92%, accompanied by an increased level of LVEDV (from 128.31 ml to 134.1 ml) and an elevated level of LVESV (from 48.92 ml to 59.11 ml). A contrast enhancement scan showed that the extent of late gadolinium enhancement of the inferior wall was about 50%-75% both at baseline and follow-up, which could be considered transmural myocardial necrosis (Figure 1h, 1i).
Case 2
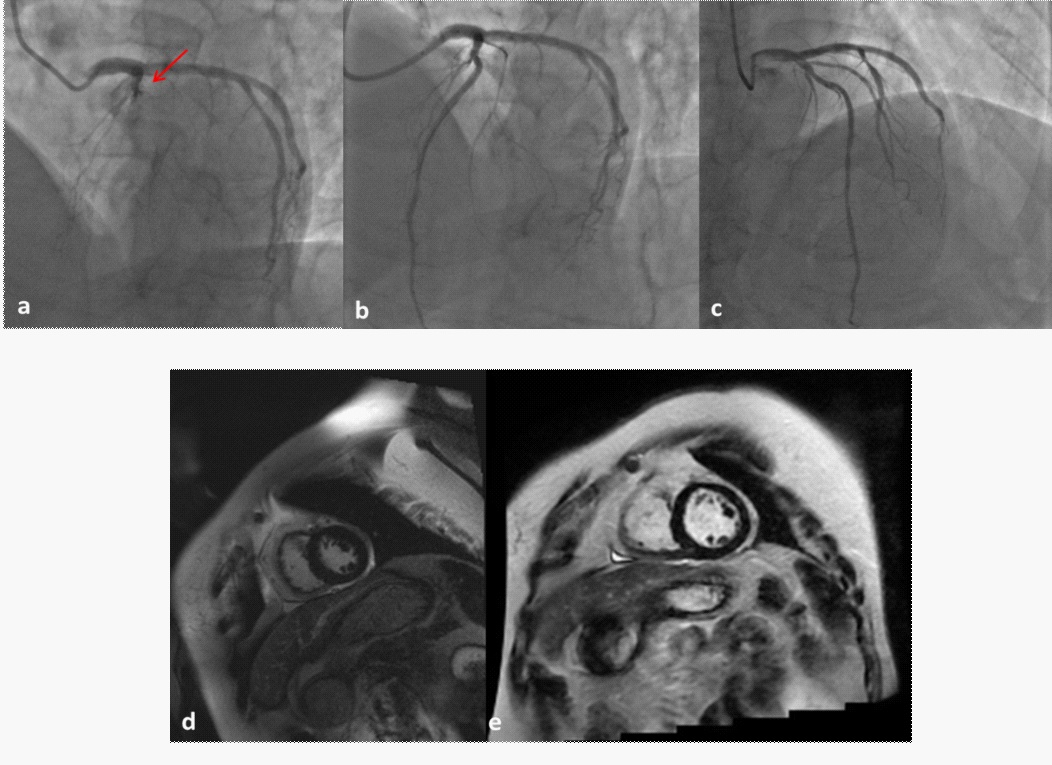
A 57-year-old woman was admitted to our hospital with discontinuous chest pain lasting more than a month. Cardiovascular risk factors included diabetes mellitus, hyperlipidemia, and obesity (Body Mass Index (BMI) = 28.23 kg/m2 ). Coronary angiography showed a completely occluded LAD, D1 (Fig 2a) with Rentrop 3 grade collaterals from the LCX, and 40-50% stenosis in the middle LCX. We employed an antegrade approach to stent a PILOT 50 guidewire through the occlusion lesion. After repeated balloon dilation using a 1.25 X 10 mm Terumo Tazuna balloon, a 1.25 X 6 mm Medtronic Springer Legend balloon, and a 2.5 X 15 mm B.Braun balloon, one 3.0 X 28 mm Abbott Xience Xpedition stent was deployed at the occluded lesion. D1 was then revascularized by balloon dilation using a 1.25 X 6 mm Medtronic Springer Legend balloon and a 1.5 X 15 mm Cordis EMPIRA balloon. The angiographic result was excellent (Figure 2b).
Follow-up
After the successful CTO PCI procedure, the patient successfully lost weight, with her BMI declining to 26.50 kg/m2 after one year. However, her blood glucose levels remained poorly controlled (glycosylated hemoglobin ranged from 6.9% to 7.4%). Repeated coronary angiography showed almost no changes in the LAD compared with that after the PCI procedure (Figure 2c). Nevertheless, CMR detected that LVEF decreased from 75.18% to 66.53%, while LVEDV increased from 82.48 ml to 124.54 ml, and LVESV increased from 20.47 ml to 41.69 ml. Furthermore, the quantitative total enhanced volume measured by CMR increased from 0.62 ml to 4.94 ml, however this was not observed visually (Figure 2d, 2e).
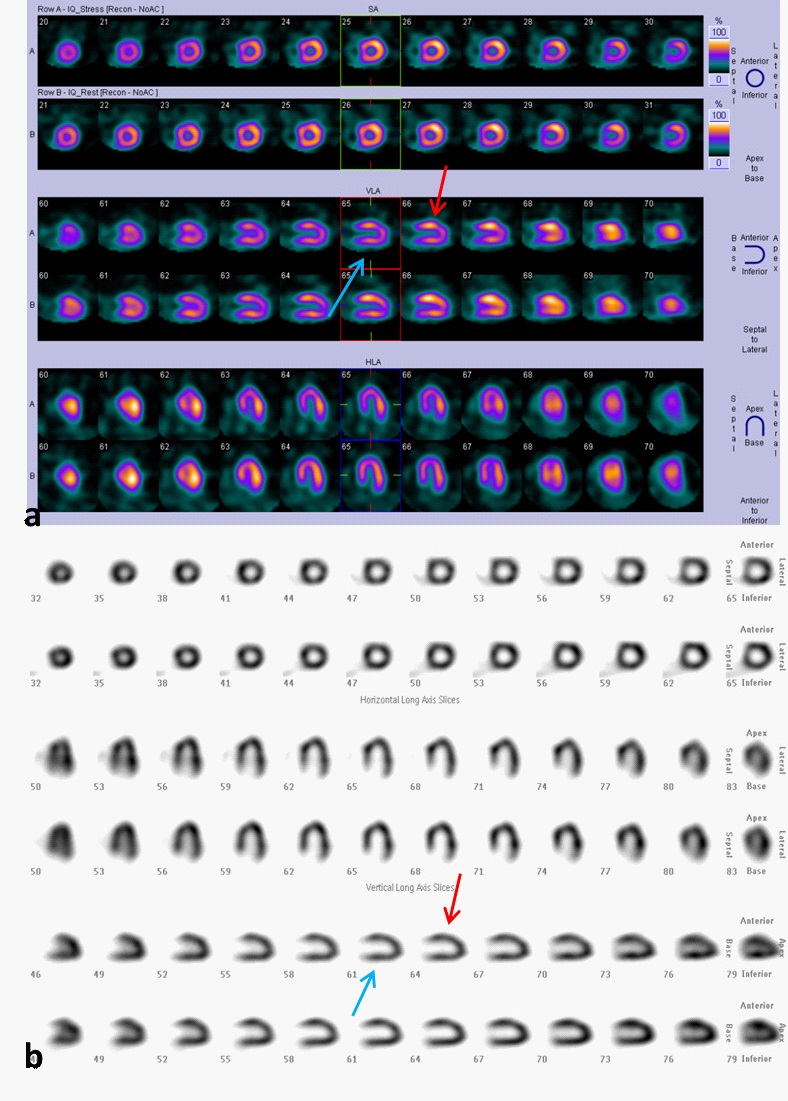
This patient also underwent SPECT both before and one year after the revascularization of the CTO artery. Obvious ischemia in the anterior wall and slight ischemia in the inferior wall was noted before PCI procedure (Figure 3a). The ischemia in the anterior wall was reduced one year after reopening the LAD, however the ischemia in the inferior walls persisted (Figure 3b).
Case 3
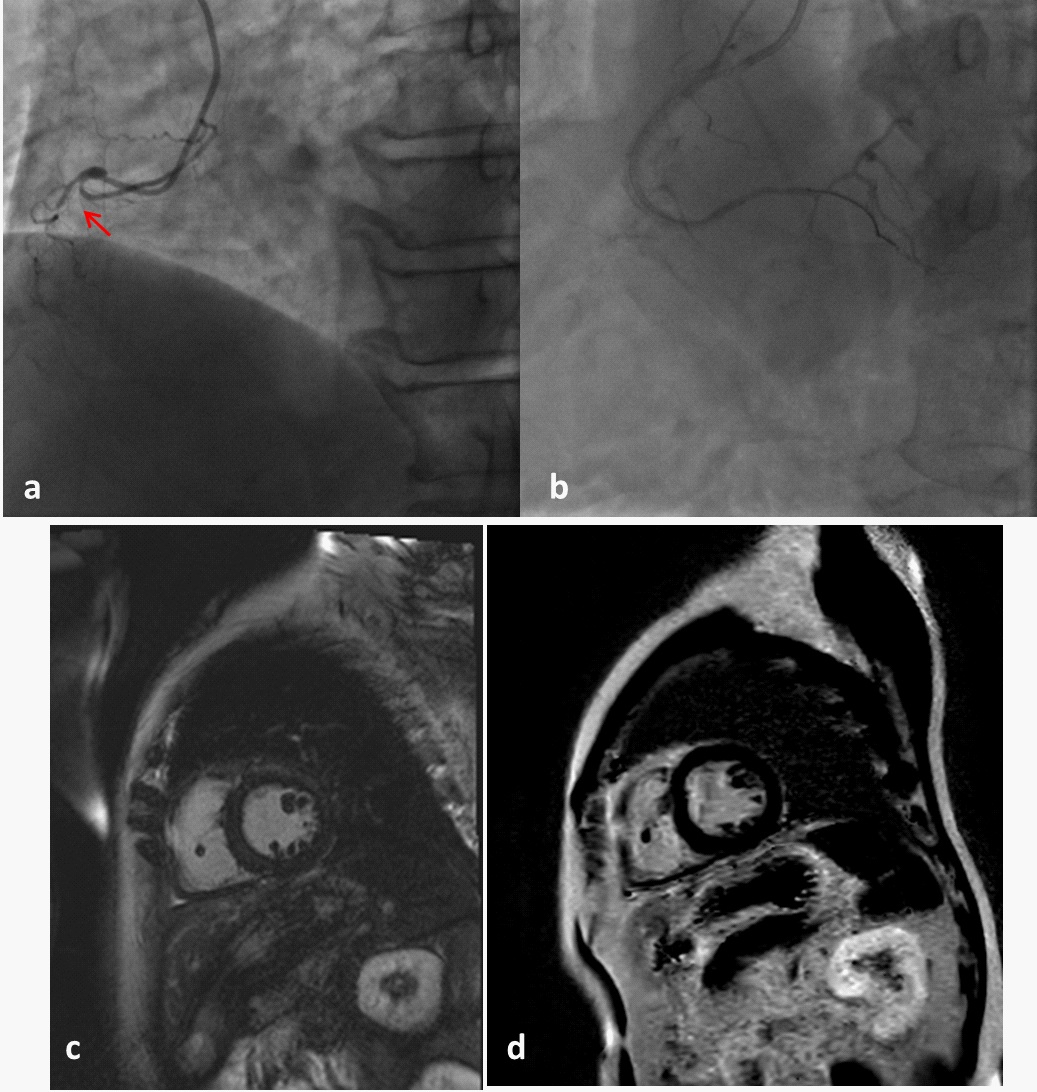
A 67-year-old man presented for evaluation at our outpatient cardiology clinic with a 6-year history of effort angina. Cardiac risk factors of this patient included alcohol consumption (approximately 70-100 g/d for over 20 years) and hypertension. Coronary angiography revealed proximal RCA-CTO (Figure 4a) with Rentrop 3 grade collaterals in the LAD and LCX. An ASAHI Conquest Pro 12 guidewire finally succeed with an antegrade approach after Fielder XT and Gaia First guidewires failed to pass through the occluded lesion. We used a 1.2 X 15 mm Boston Scientific balloon, a 2.0 X 15 mm B.Braun balloon and a 2.5 X 15 mm MACH2 balloon to dilate the lesion, and two stents (2.5 X 35 mm and 3.0 X 35 mm BUMA stents) were successfully implanted with good angiographic results (Figure 4b).
Follow-up
Upon follow-up, the patient’s blood pressure and plasma lipid levels were controlled, and alcohol consumption was sustained. However, CMR showed significantly worse cardiac function one year after CTO PCI, as indicated by a decreased LVEF from 70.77% to 59.48%, an increased LVEDV from 113.7 ml to 135.43 ml, and an elevated LVESV from 33.23 ml to 84.83 ml. No evident late gadolinium enhancement was observed on CMR images (Figure 4c,4d). The patient refused angiography at follow-up, so we advised coronary CT Angiography (CTA) instead. The CTA showed no evident lumen restenosis.
Discussion
All three patients in this case series had CTO lesions in the single main epicardial branch, and the PCI procedure was successful during the first attempt in all cases.
Here, we presented cases with deteriorating cardiac function one year after a successful CTO PCI procedure. However, the deterioration observed in these cases does not appear to be associated with the PCI itself. Thus, it should be considered that postoperative risk factors attenuate the true benefits of CTO revascularization. Additionally, the patients’ selection for CTO revascularization is crucial.
These cases present two important points: First, successful revascularization of the CTO artery is not enough to improve the long-term prognosis, pointing to the importance of postoperative risk factor control. Second, eligible patients for revascularization should be selected prudently. Interventional cardiologists should weigh the potential benefits and additional injuries of each treatment option before determining the appropriate therapy.
Risk factor control is necessary following CTO revascularization
The common cause of worsening cardiac function appears to be poorly controlled risk factors. The first patient presented here did not quit smoking after the procedure and presented with aggravated stenosis in the non-CTO vessels at his one-year follow-up appointment. The second patient had slim ischemia in a remote area not supplied by the CTO vessel (the inferior wall), as shown by SPECT images. This existed both before and after the CTO PCI. This patient was at risk of microvascular dysfunction because she had a long history of hyperglycemia with poorly controlled blood glucose levels. Ischemia in the inferior wall likely resulted from microvascular dysfunction because no obvious RCA stenosis was observed. This microvascular dysfunction likely contributed to worsening cardiac function in this patient [8].
The third patient exhibited decreased levels of LVEF and increased levels of LVEDV and LVESV. Considering his blood pressure and plasma lipid levels were well controlled, we suspected that alcohol abuse was his most serious risk factor, as alcohol-induced cardiotoxicity is often associated with cardiac remodeling [9]. Moreover, alcohol consumption damages endothelial function by inducing inflammation, platelet aggregation, plasma viscosity, and increasing fibrinogen concentration [10], which are all common factors for intramyocardial vessels. Furthermore, endothelium-dependent coronary microvascular remodeling may have adverse effects on cardiac function due to myocardial fibrosis and increased stiffness of the myocardial wall [11]. Although there is limited understanding of the precise mechanisms by which alcohol consumption affects systolic cardiac function, alcohol consumption should be constricted nonetheless.
Patient selection for CTO revascularization is necessary
In the first patient we observed, a transmural extent of infarction (TEI) >50% in the region of the CTO detected by baseline CMR may play a role in cardiac deterioration. According to previous studies [12,13], recovery of regional systolic function is partially dependent on the baseline extent of the myocardial scar. There was a consensus that successful CTO PCI was less likely to bring evident benefit in patients with non-viable myocardium in the CTO territory. Therefore, we wonder that for patients with non-viable myocardium, CTO PCI dose not have to be very aggressive.
Conclusion
The cases we presented here show that preoperative assessment and postoperative management are both important in CTO treatment. Strictly selecting eligible patients and controlling risk factors may improve the beneficial value of CTO revascularization.
Statements
Acknowledgements: The authors thank Min Zhang and Yuan Zhou who performed the catheterization procedure as well as Huijuan Zuo for assisting in the preparation of this manuscript.
Funding: This study was supported by Capital Health Development Research Project (No. 2018-2-2063), National Natural Science Foundation of China (NO. 81971569 and NO.81670324), Beijing Excellent Talent Fund (NO. 2018000021469G241), and Beijing Municipal Education Commission Science and Technology Plan (NO. KM202010025016).
Declaration of conflicting interests: The authors have no conflicts of interest to declare.
Author contribution: Xueyao Yang and Jinfan Tian wrote the manuscript. Lijun Zhang contributed to the data collection. YiHe and Xiantao Song helped to conceive the topic. Mohammad Sharif Popal revised the manuscript.
References
- Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019; 40: 87-165.
- Stuijfzand W, Biesbroek PS, Raijmakers PG, Driessen RS, Schumacher SP, van Diemen P, et al. Effects of successful percutaneous coronary intervention of chronic total occlusions on myocardial perfusion and left ventricular function. Eurointervention. 2017; 13: 345-354.
- Chadid P, Markovic S, Bernhardt P, Hombach V , Rottbauer W, Whrle J. Improvement of regional and global left ventricular function in magnetic resonance imaging after recanalization of true coronary chronic total occlusions. Cardiovascular Revascularization Medicine. 2015; 16: 228-232.
- Ladwiniec A, Allgar V, Thackray S, Alamgir F, Hoye A. Medical therapy, percutaneous coronary intervention and prognosis in patients with chronic total occlusions. Heart. 2015; 101: 1907- 1914.
- Elias J, van Dongen IM, Råmunddal T, Laanmets P, Eriksen E, Meuwissen M, et al. Long-term impact of chronic total occlusion recanalisation in patients with ST-elevation myocardial infarction. Heart. 2018; 104: 1432-1438.
- Roifman I, Paul GA, Zia MI, Williams LK, Watkins S, Wijeysundera HC, et al. The effect of percutaneous coronary intervention of chronically totally occluded coronary arteries on left ventricular global and regional systolic function. Can J Cardiol. 2013; 29: 1436-42.
- Mashayekhi K, Nuhrenberg TG, Toma A, Gick M, Ferenc M, Hochholzer W, et al. A Randomized Trial to Assess Regional Left Ventricular Function After Stent Implantation in Chronic Total Occlusion: The REVASC Trial. JACC Cardiovasc Interv. 2018; 11: 1982-1991.
- Camici PG, D’Amati G, Rimoldi O. Coronary microvascular dysfunction: mechanisms and functional assessment. Nat Rev Cardiol. 2015; 12: 48-62.
- Rodrigues P, Santos-Ribeiro S, Teodoro T, Gomes FV, Leal I, Reis JP, et al. Association Between Alcohol Intake and Cardiac Remodeling. J Am Coll Cardiol. 2018; 72: 1452-1462.
- Brien SE, Ronksley PE, Turner BJ, Mukamal KJ, Ghali WA. Effect of alcohol consumption on biological markers associated with risk of coronary heart disease: systematic review and meta-analysis of interventional studies. BMJ. 2011; 342: 480-480.
- Yang JH, Obokata M, Reddy YNV, Redfield MM, Lerman A, Borlaug BA. Endothelium-dependent and independent coronary microvascular dysfunction in patients with heart failure with preserved ejection fraction. Eur J Heart Fail. 2020; 22: 432-441.
- Nakachi T, Kato S, Kirigaya H, Iinuma N, Fukui K, Saito N, et al. Prediction of functional recovery after percutaneous coronary revascularization for chronic total occlusion using late gadolinium enhanced magnetic resonance imaging. J Cardiol. 2017; 69: 836-842.
- Bucciarelli-Ducci C, Auger D, Di Mario C, Locca D, Petryka J, O’Hanlon R, et al. CMR Guidance for Recanalization of Coronary Chronic Total Occlusion. JACC Cardiovasc Imaging. 2016; 9: 547- 56.