Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
Infective endocarditis involving native aortic valve due to Burkholderia cepacia presenting as refractory heart failure in immunocompetent host: A case report
Khin Phyu Pyar1*; Sai Aik Hla2; Soe Win Hlaing2; Soe Min2; Di Wunn2; Zar Ni Htet Aung3; Nyan Lin Maung3; Arkar Moe4; Thurein Wynn5; Aung Phyoe Kyaw5; Kyaw Zay Ya5; Myo Thant Kyaw6; Zay Phyo Aung6; Zaw Lin Oo6; Aung Kyaw Thu6
1 Professor and Head/Senior Consultant Physician, Department of Medicine/ Department of Nephrology, Defence Services Medical Academy, No. (1) Defence Services General Hospital (1000-Bedded), Myanmar.
2 Department of Medicine, No. (1) Defence Services General Hospital, 1000-Bedded, Myanmar
3 Senior Consultant Physician, Department of Medicine, No. (1) Defence Services General Hospital, 1000-Bedded, Myanmar.
4 Senior Consultant Cardiologist, Department of Cardiology, No. (1) Defence Services General Hospital, 1000-Bedded, Myanmar
5 Lecturer, Department of Medicine, Defence Services Medical Academy, Myanmar.
6 Assistant Lecturer, Department of Medicine, Defence Services Medical Academy, Myanmar
*Corresponding Author: Khin Phyu Pyar
Professor and Head/Senior Consultant Physician,
Department of Medicine/ Department of Nephrology,
Defence Services Medical Academy, No. (1) Defence
Services General Hospital, 1000-Bedded, Myanmar.
Email: khinphyupyar@gmail.com
Received : Jul 13, 2021
Accepted : Oct 01, 2021
Published : Oct 08, 2021
Archived : www.jcimcr.org
Copyright : © Mahamud B (2021).
Abstract
A 44-year-old previously healthy gentle man presented with dyspnoea for three weeks which was more severe over 7 days. He had anaemia, sinus tachycardia, wide pulse pressure of 100 mmHg, heaving displaced apex beat, and features of aortic regurgitation with occasional crackles over both lung base. Echocardiogram revealed vegetations at aortic valve. He was initially treated as a case of infective endocarditis and left ventricular failure with amoxicillin, gentamycin and anti-failure treatment. However, heart failure was very refractory and even worsening; he expired five days after arrival to our hospital. Blood culture obtained after his death showed a growth of unusual organism Burkholderia cepacia.
Keywords: infective endocarditis; aortic regurgitation; refractory heart failure; Burkholderia cepacia.
Citation: Pyar KP, Hla SA, Hlaing SW, Min S, Wunn D, et al. Infective endocarditis involving native aortic valve due to Burkholderia cepacia presenting as refractory heart failure in immunocompetent host: A case report. J Clin Images Med Case Rep. 2021; 2(5): 1349.
Background
Infective endocarditis is a rare infectious disease involving the endocardial surface of the heart and vascular endothelium. As it has significant morbidity and mortality, early diagnosis and treatment is extremely important. The diagnosis of infective endocarditis is suspicious if a patient with known congenital heart disease or rheumatic heart disease develops fever; likewise, it is one of the possible diagnosis in a patient with prolonged fever. In reviewing infective endocarditis, native valve involvement was seen in 70% of cases [1]. Generally left sided valves are more commonly involved in infective endocarditis than right sided one; tricuspid valve involvement is seen in intravenous hero in users. The common causal organisms found in native valve endocarditis were Staphylococcus aureus and Streptococcus viridans and Enterococcus species. Burkholderia cepacia rarely causes endocarditis; but, it is known to cause infective endocarditis particularly in intravenous heroin users, immunocompromised host and in patients with prosthetic valve replacement [2]. However, infective endocarditis caused by Burkholderia cepacia in native valve of immunocompetent patient was rarely reported [3,4]. Because of worldwide decreasing antimicrobial sensitivity and its de-novo antibiotic resistance, Burkholderia cepacia is difficult to treat. Mortality rate of infective endocarditis varies from 15% to 40%. There were several predicting factors favoring death like old age, heart failure, requirement for haemodialysis, anaemia and thrombocytopenia [5].
Case presentation
The patient was 44 year old soldier, previously healthy man, transferred from Rakhine State because of shortness of breath for 3 weeks. It was progressive in nature and he had to sleep in sitting position for one week. He also had cough with blood streak sputum. He denied fever, minor dental procedure or intravenous drug use.
On examination, vital signs revealed a temperature of 36.5o C, pulse rate 90/minute with collapsing in character, respiratory rate 22/minute, and blood pressure 130/30 mmHg (wide pulse pressure 100 mmHg). He had anaemia of mild degree; there was no other features of infective endocarditis like clubbing, splinter haemorrhage or splenomegaly. On auscultation, an early diastolic murmur was heard at left sternal border.
His total WBC count was normal 7.1x109 /L; differential count too (neutrophils 70.4%, lymphocytes 24.9%, monocytes 4.7%). Haemoglobin was 11.0 g/dL (MCV 93 µm3 , MCH 27.5 pg, MCHC 29.5 lg/dl) and platelet count was low normal 133x109 /L. ESR was 50 mm at 1st hour. Fasting blood sugar was 5.1mmol/l. His serum creatinine was marginally raised i.e., 1.9 mg%. Chest Xray showed moderate cardiomegaly with pulmonary congestion. Electrocardiography revealed left ventricular hypertrophy with sinus tachycardia.
Mobile vegetation on the aortic valve was seen in echocardiography. Left ventricular ejection fraction was 60%. Both left atrium and ventricles were dilated with mild mitral regurgitation. There was no evidence of pericardial effusion.
He was treated as a case of infective endocarditis with parenteral gentamycin 80 mg 12 hourly and amoxicillin 1 gram 4 hourly. Anti-failure treatment (frusemide, carvedilol, aldectone) was given along with oxygen therapy. Parenteral morphine was added as he had worsening left ventricular failure. Cardiac surgical team planned for aortic valve replacement.
He was afebrile throughout the stay in hospital. Despite treatment, left ventricular failure was uncontrollable; and, he expired 5 days after admission.
The blood culture obtained after death showed growth of Burkholderia cepacia. The isolates were sensitive to Meropenum, levofloxacin and trimethoprim and sulphamethoxazole .The MIC were (4), (2) and (20) respectively.
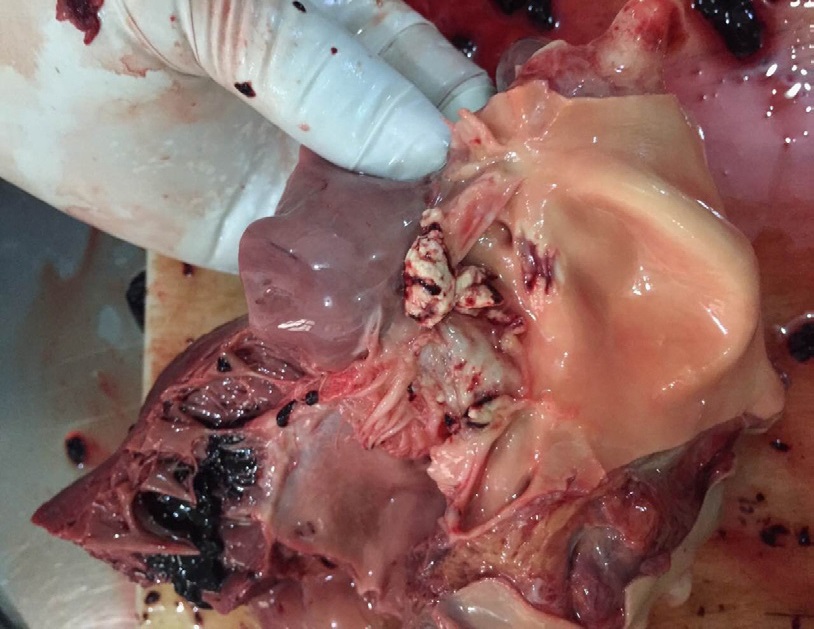
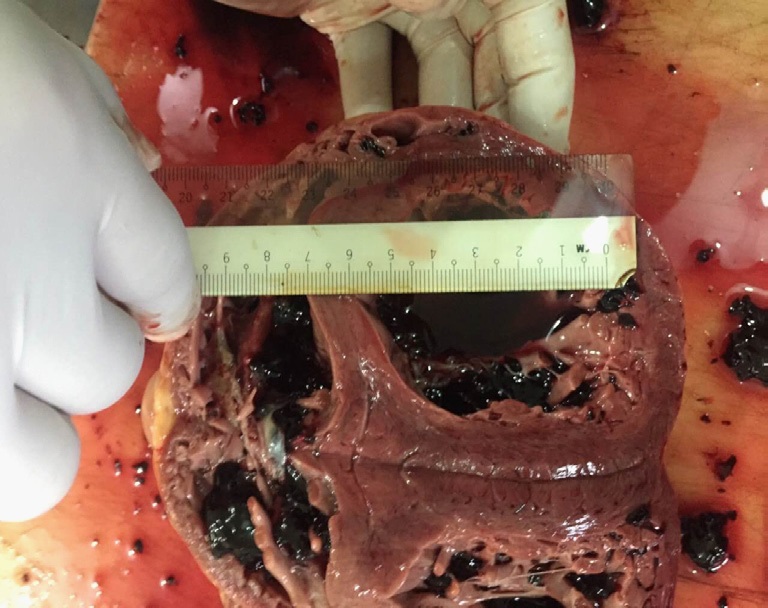
Post-moterm examination revealed vegetation over aortic valve (Figure 1). Heart was enlarged and left ventricle was dilated (Figure 2). The spleen was soft and septic. Both kidneys were normal. The lungs were congested. There was no evidence of embolization or abscess in other organ.
Discussion
Infective endocarditis is one of the possible complications of both congenital heart disease and rheumatic heart disease if they undergo invasive procedure without antibiotic prophylaxis. It is more commonly reported after prosthetic valve replacement [2,6]. Most of the cases with infective endocarditis had minor procedure with underlying known rheumatic heart disease. In this patient, he did not have invasive procedure before and we did not identify the source of infection; this is one reason for reporting.
The most common presentation of infective endocarditis is fever [11]; and, the remaining are unexplained anaemia, undue tachycardia, refractory heart failure, changing cardiac murmur and that of thromboembolic complications like stroke, brain abscess and pyemic abscess in kidney etc. In this patient, left ventricular failure (dyspnoea of varying degree, pink frothy sputum, crackles in lung bases, tachycardia) was the main presentation which was relatively less common than others; therefore, it was another point for reporting rare presentation.
Regarding the valve involvement in endocarditis, aortic valve involvement (64%) was two times commoner than mitral valve was (36%) in some study [7]; however, the reverse was found in other report [1].
In patients with Burkholderia cepacia endocarditis resulting from native valve, the mitral valve is known to be less frequently involved than the tricuspid valve as it is infected in intravenous drug user. Only one study reported aortic valve endocarditis without any predisposing factors. In this case, aortic valve was involved.
In this case, “Whether he had aortic regurgitation before or not” and “What was the underlying aetiology if he had known aortic regurgitation” are interesting. In our country and also in other reports, the aetiology of most of both mitral and aortic valvular lesions are rheumatic in aetiology [1]. In the absence of unprotected sex was against the diagnosis of syphilitic aortic valvulitis or regurgitation.
According to his medical records, done 6 months ago, he did not have valvular lesion. If so, he had infective endocarditis with very virulent organism causing vegetations over previously normal aortic valve with regurgitant effect. In other words, the causal organism must be very virulent to give all the hemodynamic events.
The common causal organisms found in infective endocarditis were gram positive organisms: Staphylococcus aureus, Staphylococcus epidermidis, Streptococcus viridans and Enterococcus species [8]. It is very rarely cause by Burkholderia cepacia in native mitral and aortic valve [3,4] and tricuspid valve of newborn [9], intracardiac foreign body in renal transplant recipient [10]. It is very rare in immunocompetent host [11].
Burkholderia cepacia is one of the soil habitant gram negative bacilli; it has intrinsic resistant to antibiotics and antiseptics. It particularly infects patients with cystic fibrosis and chronic granulomatous diseases. Burkholderia cepacia rarely causes endocarditis; however, it is known to cause infective endocarditis particularly in intravenous heroin users, immunocompromised host and in patients with prosthetic valve replacement.Thus, this is another explanation for presenting the case.
The case expired just 5 days after arrival to our hospital; the blood culture result obtained one week showed the notorious organism- Burkholderia cepacia. In fact, it is difficult to treat because of its de-novo antibiotic resistance and antimicrobial resistance worldwide. It again pointed out the importance of early diagnosis, appropriate treatment and timely referral.
In view of reported complications of infective endocarditis, in order of frequency were heart failure (36%), atrial fibrillation (13%) and thromboembolic complication producing cerebrovascular accident (9%) [7]. In this patient, the initial presentation was more of complication- left ventricular failure.
Mortality rate of infective endocarditis is not low and it may be as high as 40% [8]. The factors favoring high mortality were old age group, drug resistant organism, presence of heart failure, the requirement for haemodialysis, presence of anaemia and thrombocytopenia [5]. In this patient, the presenting manifestation as refractory heart failure was the main contributor for his death.
Conclusion
Refractory heart failure is one of the unusual presentations of infective endocarditis. We should be aware of very virulent micro-organism like Burkholderia cepacia even in native valve in immunocompetent host. Doing mechanical valve replacement with appropriate antibiotics may save the life. We should encourage early referral to tertiary center in cases like infective endocarditis and refractory heart failure. Although we could not save his life, we want to share our learning points.
Like Burkholderia cepacia, the micro-organisms live silently in the soil and they can invade our body silently even in immune-competent host like this patient; finally, they can even kill us silently. If we did not get the blood culture result, we would not know the name of the silent killer. This is the essence of soil microbiology.
Acknowledgements: The authors would like to thank the patient’s family for giving consent to this article. Also, to all doctors and nursing team for making great efforts in caring him. The authors acknowledged the following team; Professor Tin Moe Mya for laboratory support, Dr Htoo Pyae Thar & Dr Swan Htet for microbiological support, and Professor Khin Win Sein, Professor Saw Lwin, Professor Soe Hlaing and Professor Soe Win for administrative support.
Declaration of conflict of interest: The authors declared no potential conflicts of interests with respect to authorship and publication of this article.
Ethical approval: Our institution does not require ethical approval for reporting cases.
Funding: The authors received no financial support for publication of this article.
Informed consent: The informed consent for publication in this article was obtained from patient.
References
- Assiri AS. Clinical and microbiological profiles of infective endocarditis in a tertiary hospital in Aseer region, Saudi Arabia. Journal of the Saudi Heart Association. 2011; 23: 207–211.
- Dellalana LE, Byrge KC, Gandelman JS, Lines T, Aronoff DM, et al. A Unique Case of <i>Burkholderia cepacia</i> Prosthetic Mitral Valve Endocarditis and Literature Review. Infectious Diseases in ClinicalPrac tice (Baltimore, Md.). 2019; 27: 123-125.
- Ki HK, Kim SH, Han SW, Cheong HS. A case of native valve endocarditis caused by Burkholderia cepacia without predisposing factors. BMC Infectious Diseases. 2011; 11: 114–114.
- Sabir N, Ikram A, Gardezi A, Zaman G, Satti L, et al. Native valve dual pathogen endocarditis caused by Burkholderia cepacia and Aspergillus flavus—A case report. JMM Case Reports. 2008; 5: e005143–e005143.
- Şimşek-Yavuz S, Şensoy A, Kaşıkçıoğlu H, Çeken S, Deniz D, et al. Infective endocarditis in Turkey: Aetiology, clinical features, and analysis of risk factors for mortality in 325 cases. International Journal of Infectious Diseases : IJID : Official Publication of the International Society for Infectious Diseases. 2015; 30: 106–114.
- Thuny F, Avierinos JF, Tribouilloy C, Giorgi R, Casalta JP, et al. Impact of cerebrovascular com plications on mortality and neurologic outcome during infective endocarditis: A prospective multicentre study. European Heart Journal. 2007; 28: 1155–1161.
- Al-Tawfiq J, Sufi I. Infective endocarditis at a hospital in Saudi Arabia: Epidemiology, bacterial pathogens and outcome. Annals of Saudi Medicine. 2009; 29: 433–436.
- Khan IA, Mehta NJ. Stenotrophomonas maltophilia Endocarditis: A Systematic Review. Angiology. 2002; 53: 49–55.
- Yonas E, Damay V, Pranata R, Nusarintowati N. Infective endocarditis due to Burkholderia cepacia in a neonate: A case report. Journal of Medical Case Reports. 2018; 12: 120.
- Falcão Pedrosa Costa A, Castelo Branco Cavalcanti F, Modesto dos Santos V. Endocarditis due to Burkholderia cepacia and an intracardiac foreign body in a renal transplant patient. Revista Portuguesa de Cardiologia (English Edition). 2014; 33: 117.e1- 117.e4.
- Khan M, Lalani FK, Ikram A, Zaman G, Ahmed P. Dual Infection by Burkholderia Cepaciaand Pseudomonas Putida in an Infective Endocarditis Case. Journal of the College of Physicians and Surgeons-Pakistan: JCPSP. 2017; 27: 367–369.