Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
“Tineariasis” (or plaque-psoriasis induced by Terbinafine)
Ramirez-Bellver JL1*; Segurado-Miravalles G1; Bagazgoitia L1; Moreno C3; Ruiz-Rodriguez R1
1 Dermatology Department, Clinica Dermatologica Internacional, Madrid, Spain.
2 Dermatology Department, Hospital Universitario Ramon y Cajal, Madrid, Spain.
3 Pathology Department, Hospital Universitario Ramon y Cajal, Madrid, Spain
*Corresponding Author: Jose Luis Ramirez-Bellver
Dermatology Department, Clinica Dermatologica
Internacional, C/ Marques de Villamagna, 8 Madrid,
Spain.
Email: jluisrbellver@gmail.com
Received : Sep 21, 2021
Accepted : Nov 09, 2021
Published : Nov 16, 2021
Archived : www.jcimcr.org
Copyright : © Ramirez-Bellver JL (2021).
Abstract
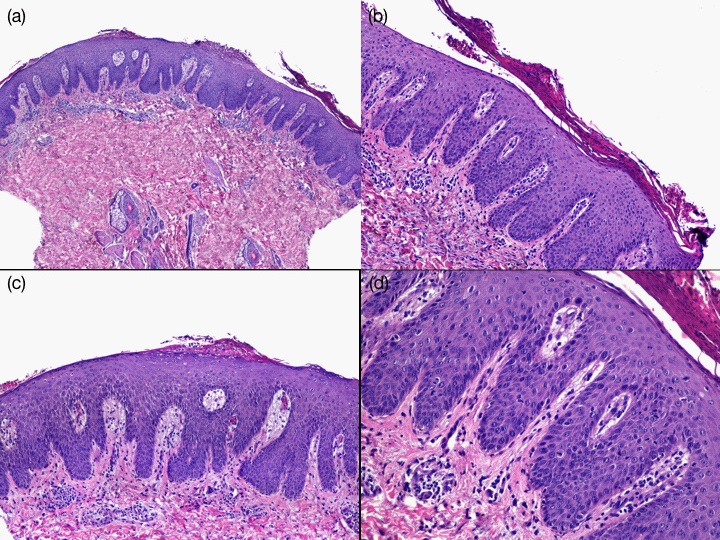
Terbinafine is an anti fungal drug used worldwide to treat dermatophytosis. Although generally is well tolerated, several cutaneous side effects have been described. One of them is the induction or exacerbation of psoriasis, especially the pustular type. We describe a case of plaque-psoriasis induced by terbinafine in a young patient. Skin biopsy was performed to confirm the diagnosis and the suspected drug was discontinued. Biopsy showed regular epidermal hyperplasia with parakeratoses and neutrophils in the corneal layer. No fungal elements were observed. Improvement was observed after discontinuation of terbinafine. We present a new case of the induction of plaque-psoriasis after the use of oral terbinafine and conclude that this drug should be used with caution in predisposed patients.
Keywords: psoriasis; pustular posriasis; plaque-psoriasis; terbinafine
Citation: Ramirez-Bellver JL, Segurado-Miravalles G, Bagazgoitia L, Moreno C, Ruiz-Rodriguez R. Tineariasis”(or plaquepsoriasis induced by Terbinafine). J Clin Images Med Case Rep. 2021; 2(6): 1407.
Introduction
Several drugs have been reported to exacerbate a preexisting psoriasis, to induct lesions on uninvolved skin in patients with psoriasis or to precipitate the disease in people with or without family history. Frequent implied drugs are beta-blockers, lithium salts, synthetic antimalarials, NSAIDS and tetracyclines. However, other substances are considered possible triggers: ACE- inhibitors, interferons and terbinafine [1]. We report the case of a patient who developed a flare up of psoriasis after initiating oral terbinafine.
Case presentation
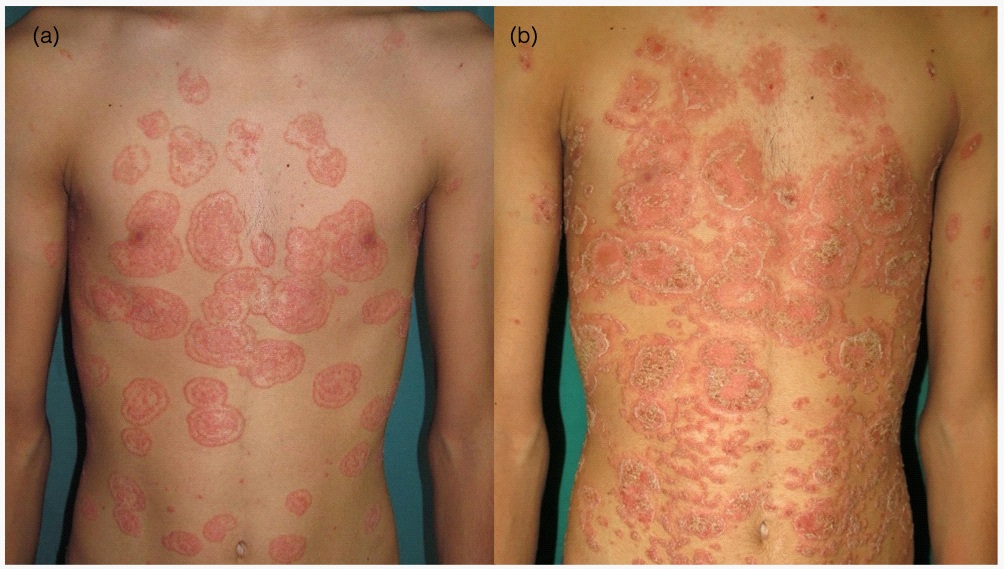
A 16- year- old male consulted for skin lesions affecting his trunk and proximal aspects of lower limbs. Medical history was unremarkable, but his father had been diagnosed of psoriasis. The lesions were well-defined, erythematous, round or oval plaques with an elevated border (Figure 1A). The clinical suspect of tinea corporis was confirmed by a positive culture for T. rubrum, and oral terbinafine (250 mg/day) was started. Eight days later the patient was admitted to the Emergency Room because of clinical worsening and pruritus. At this time, erythematous plaques had appeared under the previous lesions, which presented now desquamation and scales (Figure 1B). A biopsy was taken but terbinafine was continued. Two weeks later the lesions changed their aspect, being now confluent, erythematous-desquamating plaques in the sites described previously (Figure 2A). Because of the psoriasiform aspect of the lesions, calcipotriol/ betametasone cream was prescribed; although terbinafine was not discontinued (biopsy report was not available yet). A few days later, desquamation had disappeared and only erythematous, coalescent plaques were observed (Figure 2B). Histopathological examination showed regular epidermal hyperplasia, parakeratoses with neutrophils in the corneal layer and mild perivascular and superficial infiltrate. No fungi were observed on the stratum corneum (Figure 3). This was compatible with psoriasis and terbinafine was discontinued. Blood tests were prescribed in case systemic therapy was necessary, but a week later a dramatic clinical improvement could be observed and no oral treatment was prescribed (Figure 2C).
Case discussion
Terbinafine is a widely prescribed antifungal drug with high selective activity against fungal squalene epoxidase, which explains its relatively benign side-effects and good tolerability [2]. However, 1 in every 10 patients develops a complication, generally abdominal discomfort, but cases of liver toxicity or central nervous system affection have been reported. Approximately 3% are cutaneous reactions [3]: Exanthema, erythema and pruritus, fixed drug eruption, alopecia and lupus. Life-threatening conditions such as Steven Johnson´s syndrome or erythroderma may also occur. The induction of psoriasis, especially the pustular type, has been described, being sometimes difficult to differentiate from acute generalized exanthematous pustulosis (AGEP) [4,5].A flare-up of inverse psoriasis may also occur [6]. Although most cases refer to the use of oral terbinafine, a plaque of pustular psoriasis may develop as a result of topical application of this drug [7]. The literature data indicate that terbinafine may exacerbate pre-existing psoriasis or be responsible for the development of a psoriasis de novo, especially in predisposed patients. Although rare, generalized pustular psoriasis with alteration of liver function tests and leukocytosis may also occur [8], so physicians should monitor hepatic enzymes when serious cutaneous side effects take place during the use of terbinafine. These clinical reports have made some authors propose that oral terbinafine should not be the first antifungal drug in patients with personal or family history of psoriasis [4]. For these patients itraconazole should be considered. Nevertheless, although AGEP may occur with this drug [9], no psoriasis development has been reported with its use. Besides, no systemic antifungal therapy should be started without microbiological confirmation of fungal infection, as long as ungueal psoriasis may resemble onychomycosis and so terbinafine might be prescribed. Once pustular or other types of psoriasis have developed, treatment includes discontinuation of the drug and, according to the severity of the symptoms and the extension of the disease, systemic therapies may be required.
Conclusion
We present a case of severe plaque-psoriasis induced by terbinafine. These case report adds evidence to the recommendation that oral terbinafine should be used with caution, especially in predisposed patients. Moreover, a skin biopsy is advisable in case of lesions that change their aspect or if the patient refers symptoms different from the initial ones.
References
- Dika E, Varotti C, Bardazzi F, Maibach HI. Drug-induced psoriasis: an evidence-based overview and the introduction of psoriatic drug eruption probability score. Cutan Ocul Toxicol. 2006; 25: 1-11.
- Szepietowski JC. Terbinafine exacerbates psoriasis: case report with a literature review. Acta Dermatovenerol Croat 2003; 11: 17-21.
- Roujeau JC, Bioulac-Sage P, Bourseau C, et al. Acute generalized exanthematous pustulosis. Analysis of 63 cases. Arch Dermatol 1991; 127: 1333–8.
- Ozturk G, Turk BG, Karaca N, Karaarslan IK, Ertekin B, Ertam I, Kazandi A, Kandiloglu G. Generalized pustular eruptions due to terbinafine. Cutan Ocul Toxicol. 2012; 31: 81-4.
- Duckworth L, Maheshwari MB, Thomson MA. A diagnostic challenge: acute generalized exanthematous pustulosis or pustular psoriasis due to terbinafine. Clin Exp Dermatol. 2012; 37: 24-7.
- Pauluzzi P, Boccucci N. Inverse psoriasis induced by terbinafine. Acta Derm Venereol. 1999; 79: 389.
- Verros CD, Rallis E. The role of terbinafine in induction and/or exacerbation of psoriasis. Int J Dermatol. 2013; 52: 1155-6
- Kim BS, Jang HS, Jwa SW, Jang BS, Kim MB, Oh CK, Kwon YW, Kwon KS. Generalized pustular psoriasis and hepatic dysfunction associated with oral terbinafine therapy. J Korean Med Sci. 2007; 22: 167-9.
- Cançado GG, Fujiwara RT, Freitas PA, Correa-Oliveira R, Bethony JM. Acute generalized exanthematous pustulosis induced by itraconazole: an immunological approach. Clin Exp Dermatol. 2009; 34: e709-11.