Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
Extramedullary plasmacytoma of the tongue: A case report
Leart Berdica1,2; Teona Bushati1,2; Alfred Aga2; Emirjona Vajushi2; Erion Sukaj2; Albina Ndoja1; Agron Dogjani1*
1 Faculty of Medicine, University of Medicine of Tirana, Albania.
2 American Hospital of Tirana, Albania.
*Corresponding Author: Asc. Prof. Dr. Agron Dogjani, MD, Ph.D. FACS, FISS, FICS
Faculty of Medicine, University of Medicine of Tirana,
Albania.
Email: agron.dogjani@umed.edu.al
Received : Oct 10, 2021
Accepted : Nov 10, 2021
Published : Nov 17, 2021
Archived : www.jcimcr.org
Copyright : © Berdica L (2021).
Abstract
Background: Tongue extramedullary plasmacytoma is a very rare pathology. Despite rare cases, extramedullary plasmacytoma should be considered as a differential diagnosis in case of a mass in the tongue. A total of 19 cases were reported with EMP in English literature along with the case we will address. It is characterized by a monoclonal neoplastic proliferation of plasma cells in the absence of multiple myeloma (MM). Histopathology and immunohistochemistry are very important for the diagnosis and differential diagnosis.
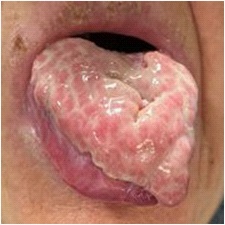
Case presentation: The case we will describe is an 80-year-old lady from Albania who presents with a vegetative lesion in the form of a thick plate on the dorsal part of the tongue with dimensions 6 X 5 X 1.5 cm. A material of 0.5 cm diameter was taken from the lesion for the biopsy. After histopathological examination, immunohistochemical examinations, and after correlations with laboratory, clinical and imaging data, the diagnosis of extramedullary plasmacytoma of the tongue was reached. The patient underwent radiotherapy treatment.
Conclusions: EMP is a rare tumor, accounting for 3% of plasma cell neoplasms and <1% of all head and neck tumors. The diagnosis of EMP, in this case, was reached with biopsy, immunohistochemistry, and the correlation with laboratory and imaging data. We will show the importance of biopsy along with immunohistochemistry in the diagnosis and differential diagnosis of extramedullary plasmocytoma of the tongue.
Keywords: plasmacytoma; immunohistochemistry; biopsy; plasma cell.
Abbreviations: EMP: Extramedullary plasmacytoma; MM: Multiple myeloma; Cm: centimeter
Citation: Berdica L, Bushati T, Aga A, Vajushi E, Dogjani A. Extramedullary plasmacytoma of the tongue: A case report. J Clin Images Med Case Rep. 2021; 2(6): 1409.
Introduction
Plasmacytoma is a rare plasma cell neoplasm that accounts for 1-2% of all tumors. EMP should be differentiated from other plasma cell lesions such as MM, plasma cell granuloma,reactive plasma cell hyperplasia together with amelanotic melanoma. MM is similar histologically but clinically has a multicentric origin in bone and in serum.
Protein immuno-electrophoresis the presence of myeloma proteins is observed.
In plasma cell granuloma lymphocytes, eosinophiles, neutrophils and histiocytes are found surrounded by septa of connective tissue. Plasma cell tumor involving lymph nodes is reactive plasmacytic hyperplasia. Immunohistochemical markers such as: MART – 1, S100, Melan A, HMB45 help to differentiate EMP from amelanotic melanoma [13-16].
Clinically these tumors are classified into Multiple Myeloma (MM), Solitary Bone Plasmocytoma and Extramedullary Plasmocytoma (EMP) [1].
Extramedullary plasmocytoma accounts 5-10 % of all plasma cells neoplasms [17]. It has a head-neck predilection with 80% of cases localized in the superior part of aerodigestive tract [19]. The regions most commonly involved include the nasal cavity, nasopharynx, paranasal sinuses, and tonsils [20]. Tongue involvement is extremely rare for this gammapathy [17]. EMP may present as a single or multiple lesion outside the skeleton. In the presence of skeletal deposits the diagnosis is Multiple Myeloma [21]. However as a primary manifestation multiple myeloma may have a solitary mass imitating extramedullary plasmacytoma. Multiple myeloma is the most common plasma cell neoplasm accounting for about 90% of cases, the rest consisting of extramedullary plasmacytoma or solitary bone plasmacytoma. The prognosis of multiple myeloma is poor with an average survival rate of 2-3 years. Extramedullary plasmacytoma has the best prognosis of all plasma cell neoplasms with a 10-year survival of 70% [2]. However, there is a risk of progression to multiple myeloma in a significant percentage of about 40% of patients. In these conditions a careful follow-up following treatment of extramedullary plasmacytoma is highly recommended.
Clinical case
An 80-year-old lady presents with a lesion on the tongue. The patient complains of pain, difficulty in chewing and difficulty in speaking. In the macroscopy the tumoral lesion consists in a thick placque in the dorsal part of the tongue approximately 6 X 5 X 1,5 cm. The surface is totally eroded. Pink color with gray stretch marks on the surface and solid-elastic consistency.
In this situation two incisional biopsies were performed consequently to be sure about the representation of the bioptic sample and conventional staining for HE as well as an extensive immunohistochemical panel for differential diagnosis. The material taken for the biopsy has a diameter of 0.5 cm
Microscopy: The surface of the lesion is composed of an admixture of granulation tissue and inflammatory cells. In the deepest portion there are several dense plasmacytic groups that dissect the tissue. The cells are CD38 and CD138 positive and have a high expression of Kappa and Lambda in the cytoplasm.
Several other antibodies were used for the differential diagnosis such as CKAE1/AE3, CD45, CD20, CD79a, CD3, CD5, ki67, CD34, HHV8, CD68, S100, LangherinA, CD15, CD21, CD23.
The differential diagnosis was made with carcinoma, lymphoma, Kapposi Sarcoma, Langherhans cell hystiocitosis, Inflammatory Pseudotumor.
The population of plasma cells is noticeable. In immunohistochemical examination the cells results: CKAE1/AE3 (---), CD45 (+++), CD20 (+--), CD79a (+++), CD3 (---), CD5 (+--), Ki67 = 40 %, CD34 (+--), HHV8 (---), CD68 (+--), CD38 (+++), CD138 (+++), kappa (+++), Lamda (+++), S100 (+--), Langherine A (---), CD15 (+--), CD21 (---), CD23 (---).
Following these results in histopathological and immunohistochemical examination the patient is recommended CT of the head, thorax, abdomen and pelvis. Tomography of the head, thorax, abdomen, and pelvis didn’t show the evidence of metastasis.
Also all lymph nodes of the examined regions result in no obvious neoplastic lesions. Serum Beta-2 microglobulin levels are elevated, Myelogram appears normal.
Renal funcional test results normal, also the Albumine level, uric acid and total protein levels are normal. LDH is also normal. Seric levels of IgA, IgG, IgM, Lamda, Kappa, kappa/Lamda ratio are in the norm. Protein electrophoresis shows a decrease in Albumin level and an increase in Alpha-2-globulin, while Alpha1-globulin, Beta globulin, Gamma globulin and A/G ratio arepresent at normal levels.
Erythrocyte sedimentation rate is normal. In the urine analysis proteinuria is observed. Based on all the results mentioned above as well as clinical correlations, the diagnosis of extramedullary plasmacytoma of the tongue was made. The patient underwent radiotherapy treatment.
Discussion
EMP of the tongue is extremely rare with only a few cases reported in the literature [8,9-12]. EMP is one of the three types of plasma cell neoplasms. The other two are multiple myeloma and solitary bone plasmocytoma (also called medullary plasmacytoma) [18]. Extramedullary plasmocytoma accounts about 5-10% of all plasma cell neoplasms [17]. It shows a head-neck region preference with 80% of cases localized in the upper part of the aerodigestive tract [19]. Areas most commonly involved include the nasal cavity, nasopharynx, paranasal sinuses, and tonsils [20]. Clinically the oral cavity plasmacytoma manifests as swelling, jaw pain, toothache, paresthesia, tooth movement, tooth migration, hemorrhage, and pathological bone fractures [7,9,16]. Extramedullary plasmacytoma affects men more often than women with a male ratio: Female 3:1. The average age is 55 years old [20]. It is very important to get in-depth biopsy as 80% of extramedullary plasmacytomas originate from the submucosa and taking the biopsy to the surface can lead to a false negative result with fatal consequences for the patient [18]. In these conditions the threshold for biopsy recurrence should be small, especially when there is strong clinical suspicion.
Histopathological diagnosis of plasma cell neoplasms requires the presence of malignant monoclonal proliferation of the plasma cell line. Plasma cells produce CD138 and a light monoclonal cytoplasmic chain, kappa or lambda [21]. Plasma cells are immature and present the malignancy characteristics of immature cells with atypical hyperchromatic nuclei and no visible nucleoli. Prominent histological features of extramedullary plasmacytoma include infiltration of affected areas of soft tissue with plasma cells [17]. Moreover, amyloid deposition is common in plasmocytoma and this can be detected as a deposit that appears apple green under polarized light and red when the tumor is stained with Congo red stain [21]. When the diagnosis of plasma cell tumor is established by immunohistochemistry, the next step is to distinguish whether it constitutes a solitary lesion consistent with plasmacytoma or is part of several multiple lesions indicating the presence of multiple myeloma [20,22]. Further hematological, biochemical and radiological examinations should be used to look for other extra skeletal or skeletal lesions [20]. Hematological and biochemical examinations include whole blood analysis with white matter differentiation, uremia, creatinine and electrolytes, CRP, ESR, and concentrations of beta-2 microglobulin and immunoglobulins. Skeletal examination includes serum calcium, albumin, and alkaline phosphates. Ongoing serum and urine protein electrophoresis including Bence-Jones proteins should be considered. Finally, a bone marrow biopsy is often necessary and constitutes an important component in the diagnostic process [17,21]. The prognosis of the early stages of EMP is relatively good, especially if the tumor is in the head-neck region [3]. The prognosis becomes poor when EMP progresses to MM [2]. In this way it is important that EMP is diagnosed early to have a good result [1,4]. However, the overall 5 - year survival drops from 83.7% to 30% when these patients progress to MM [2]. Progression from EMP to MM was the only negative prognostic factor identified for laryngeal EMP [2]. Plasmacytomas are very radiosensitive tumors: the recommended treatment for extramedullary plasmocytomas is surgery or radiotherapy. These treatments are more or less the same effectiveness and with similar recurrence rates. Various authors recommend combining both as the optimal treatment for extramedullary plasmacytoma [23]. The decision on which treatment to choose depends on many factors and should be made by a multidisciplinary staff of head and neck oncology, taking into account the patient’s wishes.
Conclusion
EMP is a rare tumor, accounting for 3% of plasma cell neoplasms and <1% of all head and neck tumors. The diagnosis of EMP in this case was reached with biopsy, immunohistochemistry and the correlation with laboratory and immaging data. It is very important that EMP should be differentiated from other plasma cell lesions such as MM, plasma cell granuloma, reactive plasma cell hyperplasia together with amelanotic melanoma. This differential diagnosis as described during the presentation of the case was made with immunohistochemistry and in the case of MM with serum electroforesis and CT of total body. The biopsy and the immunohistochemistry has a key role in the diagnosis and consequently in the treatment of the EMP.
The patient underwent radioterapy and the result was satisfactory as shown in the figure number 2.
It is very important the follow- up of the patient because in some cases the EMP can progress to MM and this is related to a poorer prognosis.
Declarations
Ethical Approval and Consent to participate: Not applicable.
Consent for publication: Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Availability of supporting data: Not applicable.
Competing interests: Not applicable.
Funding: Not applicable.
Authors’ contributions: LB carried out the histopathological and immunohistochemistry diagnosis, participated in the sequence alignment and drafted the manuscript. TB carried out the immunoassays. AA participated in the sequence alignment. EV participated in the design of the study and performed the statistical analysis. ES participated in its design and coordination and helped to draft the manuscript. AD conceived of the study, and helped in assuming data for this case report. All authors read and approved the final manuscript.
Acknowledgements: Not applicable.
References
- Alwan H, Moor JW, Wright D, Kanatas AN and Cruickshank HE. Extramedullary plasmacyto¬ma of the tongue base: a case report and clini¬cal review of head and neck plasmacytoma. Ear Nose Throat J 2010; 89: 369-373.
- Xing Y, Qiu J, Zhou ML, Zhou SH, Bao YY, Wang QY and Zheng ZJ. Prognostic factors of laryn¬geal solitary extramedullary plasmacytoma: a case report and review of literature. Int J Clin Exp Pathol 2015; 8: 2415-2435.
- Liu HY, Luo XM, Zhou SH and Zheng ZJ. Progno¬sis and expression of lambda light chains in solitary extramedullary plasmacytoma of the head and neck: two case reports and a litera¬ture review. J Int Med Res 2010; 38: 282-288.
- Onal C, Oymak E, Uguz A and Ergin M. Primary solitary extramedullary plasmacytoma of the tongue. Ear Nose Throat J 2012; 91: 292-295.
- Tournier-Rangeard L, Lapeyre M, Graff-Caillaud P, Mege A, Dolivet G, Toussaint B, Charra-Brun¬aud C, Hoffstetter S, Marchal C and Peiffert D. Radiotherapy for solitary extramedullary plas¬macytoma in the head-and-neck region: a dose greater than 45 Gy to the target volume im¬proves the local control. Int J Radiat Oncol Biol Phys 2006; 64: 1013-1017.
- Chao MW, Gibbs P, Wirth A, Quong G, Guiney MJ and Liew KH. Radiotherapy in the manage¬ment of solitary extramedullary plasmacyto¬ma. Intern Med J 2005; 35: 211-215.
- Martinelli C, Rulli MA. Primary plasmacytoma of soft tissue (gingiva). Report of a case. Oral Surg Oral Med Oral Pathol. 1968; 25: 607 – 609.
- Webb CJ, Makura ZG, Jackson SR, Helliwell T. Primary extramedullary plasmacytoma of the tongue base. Case report and review of the literature. ORL J OtorhinolaryngolRelat Spec. 2002; 64: 278 – 280.
- Pisano JJ, Coupland R, Chen SY, Miller AS. Plasmacytoma of the oral cavity and jaws: a clinicopathologic study of 13 cases. Oral Surg Oral Med Oral Pathol Oral RadiolEndod. 1997; 83: 265 – 271
- Alwan H, Moor JW, Wright D, Kanatas AN, Cruickshank HE. Extramedullary plasmacytoma of the tongue base: a case report and clinical review of head and neck plasmacytoma. Ear Nose Throat J 2010; 89(8): 369-373.
- Hama Y, Uematsu M, Kusano S. Solitary extramedullary plasmacytoma of the tongue. Ulster Med J. 2004; 73(2): 132- 134.
- Montero C, Alvarez J, Torrico P, Pando-Pinto J, Blasco A. Primaryextramedullaryplasmocytoma of the tongue base. Acta Otorrinolaringol Esp. 1999; 50(8): 657-659.
- Ozdemir R, Kayiran O, Oruc M, Karaaslan O, Kocer U, Ogun D. Plasmacytoma of the hard palate. J Craniofac Surg. 2005; 16: 164 – 169.
- Epstein JB, Voss NJ, Stevenson-Moore P. Maxillofacial manifestations of multiple myeloma. An unusual case and review of the literature. Oral Surg Oral Med Oral Pathol. 1984; 57: 267 – 271.
- Wood NK, Goaz PW. Differential Diagnosis of Oral and Maxillofacial Lesions. St. Louis: The CV Mosby Co.; 1996: 385.
- Lust J. Solitary plasmacytoma of bone and extramedullary plasmacytoma. In: Gertz M, Greipp P, editors. Hematologic malignancies: Multiple myeloma and related plasmacell disorders. New York: Springer-Verlag; 2004. p. 111-118.
- Hama Y, Uematsu M, Kusano S. Solitary extramedullary plasmacytoma of the tongue. Ulster Med J. 2004; 73: 132–4.
- Iseri M, Ozturk M, Ulubil SA. Synchronous presentation of extramedullary plasmacytoma in the nasopharynx and the larynx. Ear Nose Throat J. 2009; 88: E9 – 12.
- Galieni P, Cavo M, Pulsoni A, et al. Clinical outcome of extramedullary plasmacytoma. Haematologica. 2000; 85: 47–514..
- Straetmans J, Stokroos R. Extramedullary plasmacytomas in the head and neck region. Eur Arch Otorhinolaryngol. 2008; 265: 1417–234.
- Webb CJ, Makura ZG, Jackson SR, Helliwell T. Primary extramedullary plasmacytoma of the tongue base. Case report and revieë of the literature. ORL J Otorhinolaryngol Relat Spec. 2002; 64: 278 –80
- Marom T, Goldfarb A, Vaknine H, Kravtsov V, Roth Y. Clinicalphotograph. Sinonasal extramedullary plasmacytoma. Otolaryngol Head Neck Surg. 2009; 141: 533–4
- Tsang RW, Gospodarowicz MK, Pintilie M, et al. Solitary plasmacytoma treated with radiotherapy: impact of tumor size on outcome. Int J Radiat Oncol Biol Phys 2001; 50: 113 –20