Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
Atypical cellular blue nevus: A case report and review of literature
Shi H1#; Fidelis C2#, Zou Y3 ; Liang J1 ; Huang B1 ; Zhou B1 ; Liang Z1 *
1Department of Thoracic Oncology, The Cancer Center of the Fifth Affiliated Hospital of Sun Yat-sen University, China
2 Department of Anatomy, Midlands State University, Gweru, Zimbabwe
3 Department of Oncology and Hematology, Huizhou Sixth People's Hospital, China.
$ Equal Contribution.
*Corresponding Author: Zibin Liang
Department of Thoracic Oncology, The Cancer Center
of The Fifth Affiliated Hospital of Sun Yat-sen
University, Zhuhai 519020, China
Email: liangzb@mail.sysu.edu.cn
Received : Sep 10, 2021
Accepted : Nov 19, 2021
Published : Nov 26, 2021
Archived : www.jcimcr.org
Copyright : © Liang Z (2021).
Abstract
Blue nevi are benign neoplasms of many variants which have several similar histological, clinical and immunochemical features. The two most frequent types are dendritic/common blue nevus and cellular blue nevus. Atypical blue nevus is a rare variant of cellular blue nevus whose characteristics are usually confused with malignant blue nevus/malignant melanoma which arise in a cellular blue nevus. Our paper describes a case of a 59-year-old woman who presented with a pigmented lesion in her right gluteal region which started itching and slowly grew in the last 20 years. After surgical resection, histopathological examination showed a nodule which had features that were consistent with atypical cellular blue nevus.
Keywords: atypical; cellular; blue nevus.
Citation: Sackey AD, Sackey AD, John B, Lee-Duah RO. A look into “Outlining the challenges of Covid-19 health crises in Africa’s maritime industry: The case of maritime operations in marine warranty surveying practice”: Discussing ‘three pillar challenge’. J Clin Images Med Case Rep. 2021; 2(6): 1429.
Background
Blue nevus and its related lesions are a group of heterogenous melanocytic proliferations first described by Max Tie`che in [1], which share several morphological and clinical characteristics [2,3]. Some of the features reported include the blue tinctorial property, proliferation of oval/spindle melanocytes, presence of heavily pigmented dendritic cells, variable fibrosis of the stroma and the presence of macrophages [4,5]. Immunohistochemically, blue nevi tumours express melanoma associated antigen HMB45, S100 and Melan A/Mart-1 [2]. In literature, the clinocopathologic features of the two frequent types of blue nevi have been described. These include Dendritic or Common Blue Nevus (DBN) and Cellular Blue Nevus (CBN) which has been further subdivided into Atypical Cellular Blue Nevus (ACBN) and Malignant Blue Nevus (MBN). Atypical Cellular Blue Nevus (ACBN) refers to a rare form of the typical Cellular Blue Nevus (CBN) which shows atypical histological characteristics between Cellular Blue Nevus (CBN) and Malignant Blue Nevus (MBN) [6]. According to literature published on the subject, the distinction between Cellular Blue Nevus (CBN) and Atypical Cellular Blue Nevus (ACBN) remains difficult, and currently there is no consensus among pathologists with regards to the biological descriptions of these atypical neoplasms [7].
A few number of case reports published have reported on the histopathological appearance of Atypical Cellular Blue Nevus (ACBN). Some of the histological characteristics include features similar to Cellular Blue Nevus (CBN), such as a superficial lesions in the dermis or subcutaneous adipose tissue composed of oval to spindle cells, dendritic melanocytic cells and a number melanophages [2]. In many cases, sclerosis has been reported to be a characteristic feature of cellular CBN [8,9]. However, any additional feature to the CBN histological pattern in the absence of malignancy is referred to as ACBN. Due to the rarity nature of ACBN, we hereby report a case with histological features and characteristics similar to ACBN and a review of literature.
Case presentation
A 59-year-old immunocompetent woman, with a nevoid lump in her right buttock area for over 50 years without symptoms was studied. She got know to about it from her family when she was a child. She often felt itching there for the previous 20 years while the growth increased slowly in size. The lesion was dome-shaped, black in color and measured 1.5 cm in diameter. The patient’s Karnofsky score was 90. Ultrasound assessment showed an elliptic low echo inside the skin of buttock with the size of about 17 X 8 mm. The internal echo was uniform without obvious changes after pressure and had a slight posterior acoustic enhancement.
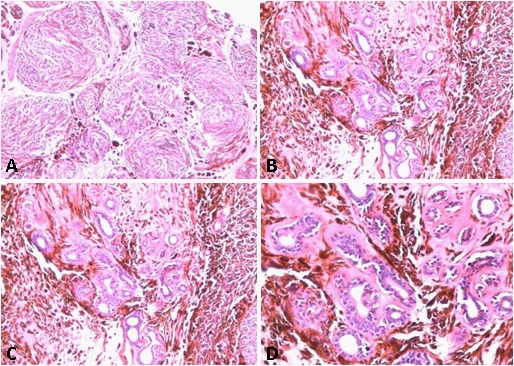
The histological examination showed an obscure boundary, wedge nodule in subcutaneous fat (Figure 1A and B), with the involvement of skin accessory organs and nerve bundles (Figure 1C and D). The tumor was composed of heavily pigmented, sphaerocysts of various sizes and polygonal cells which contained a small amount of pigment. Some of the cells present were small, with vesicular ovoid nuclei and eosinophilic nucleoli. Others cells had large and round vesicular nuclei with clearly eosinophilic nucleoli. In addition there were pigmented macrophages, few polykaryocytes and the presence of interstitial fibrosis and hardening.
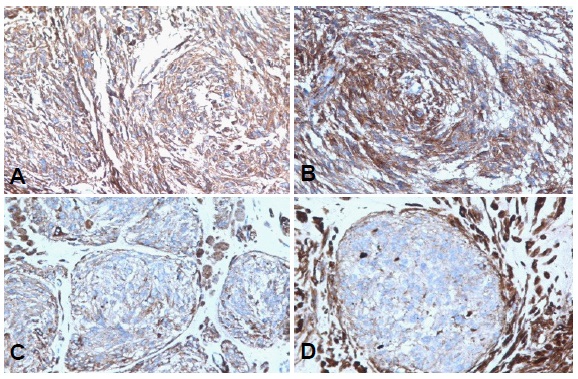
Immunohistochemical findings included Melan-A and HMB45 (Figure 2A and B), while only a few cells were reactive for S-100 (Figure 2C). These results indicate that all pigmented cells were epithelioid melanocytes. Nevocytes were negative for CD68 and CD34. Ki-67-labeled nuclei were present although very low (<2 mm2 ). All of these findings were consistent with atypical cellular blue nevus.
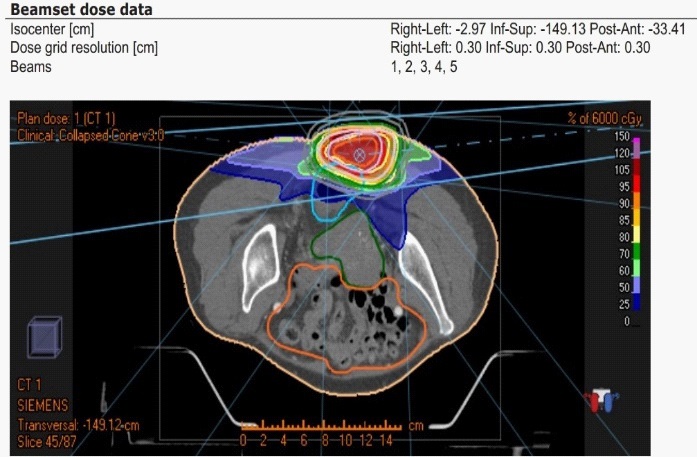
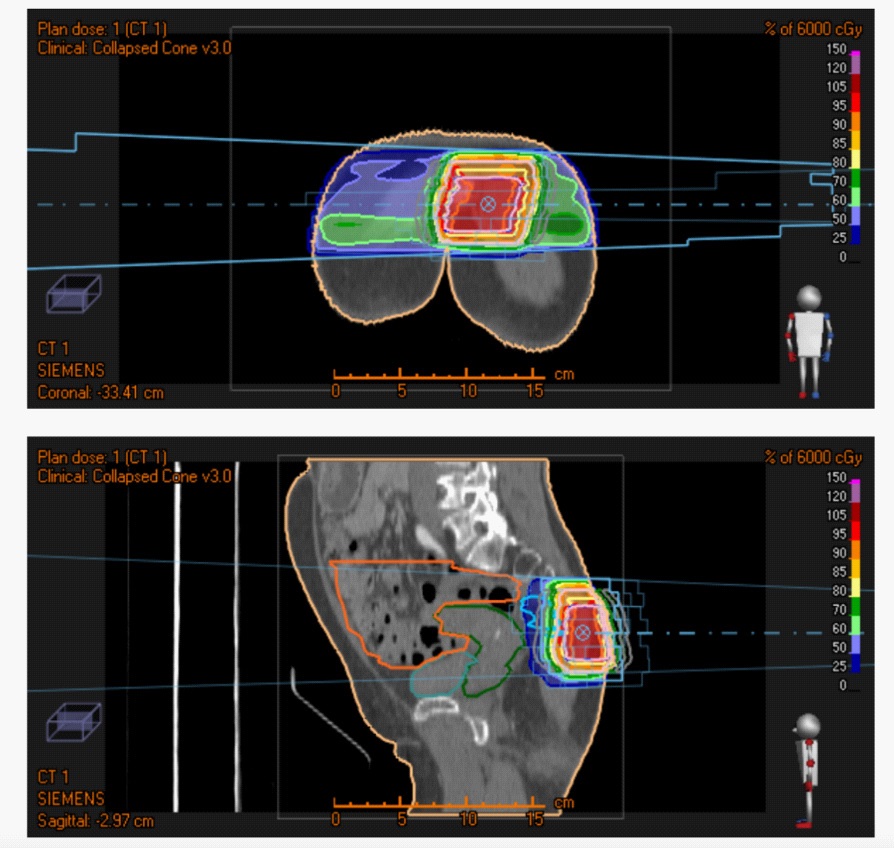
On imaging, contrast-enhanced Computed Tomography (CT) simulation before radiotherapy showed a little opacity in the interspace of sacrococcygeal subcutaneous fat with reticular high density shadow, which was considered the possibility of postoperative changes. Local skin and soft tissue were negative. The right gluteal region did not swell. The patient received intensity modulated radiation therapy (IMRT) radiotherapy to her right gluteal area with a dose of 60Gy/30F after surgery (Figure 3).
In radiotherapy implementation, PTV1 of the patient’s right gluteal area max dose ranges from 6050 cGy to 6300 cGy, uniform 6150 cGy, min DVH 6100 cGy to 99% volume. At the same time, organs at risk are well protected. Radiation dose distribution in the Intensity Modulated Radiation Therapy (IMRT) radiotherapy to the patient’s right gluteal area and organ at risk (Figure 4).
# |
Beam name |
Number of segments |
X1 |
Maximum jaw [cm] X2 |
aperture Y1 |
Y2 |
Gantry angle [deg] |
Coll. angle [deg] |
Couch angle [deg] |
MU per fraction |
Bolus [Y/N] |
Block [Y/N] |
1 |
1 |
11 |
-3.00 |
3.40 |
-3.50 |
4.00 |
85.0 |
0.0 |
0.0 |
354.97 |
N |
N |
2 |
2 |
9 |
-3.53 |
3.54 |
-4.00 |
4.00 |
42.0 |
0.0 |
0.0 |
81.38 |
N |
N |
3 |
3 |
7 |
-4.35 |
4.07 |
-4.00 |
4.00 |
0.0 |
0.0 |
0.0 |
61.76 |
N |
N |
4 |
4 |
11 |
-3.39 |
3.82 |
-4.00 |
4.00 |
318.0 |
0.0 |
0.0 |
82.73 |
N |
N |
5 |
5 |
9 |
-3.42 |
3.49 |
-4.00 |
4.00 |
275.0 |
0.0 |
0.0 |
212.57 |
N |
N |
Dose |
Function |
ROI |
Description |
Robust |
Weight |
Value |
|
Physical Composite Objective |
|
|
No |
|
0.2890 |
Plan |
Max Dose |
External |
Max Dose 6300 cGy |
No |
60 |
1.1702E-7 |
Plan |
Min Dose |
PTV1 |
Min Dose 6050 cGy |
No |
120 |
0.0110 |
Plan |
Min DVH |
PTV1 |
Min DVH 6100 cGy to 99% volume |
No |
150 |
0.0143 |
Plan |
Uniform Dose |
PTV1 |
Uniform Dose 6150 cGy |
No |
80 |
0.0250 |
Plan |
Max Dose |
PTV1 |
Max Dose 6300 cGy |
No |
60 |
2.9169E-5 |
Plan |
Min Dose |
PTV2-PTV1 |
Min Dose 5400 cGy |
No |
100 |
0.0146 |
Plan |
Min DVH |
PTV2-PTV1 |
Min DVH 5450 cGy to 99% volume |
No |
120 |
0.0160 |
Plan |
Uniform Dose |
PTV2-PTV1 |
Uniform Dose 5500 cGy |
No |
60 |
0.1143 |
Plan |
Max Dose |
PTV2-PTV1 |
Max Dose 6000 cGy |
No |
40 |
2.0016E-4 |
Plan |
Max Dose |
ring1 |
Max Dose 5100 cGy |
No |
20 |
1.5437E-4 |
Plan |
Max Dose |
ring2 |
Max Dose 4500 cGy |
No |
20 |
0.0010 |
Plan |
Max DVH |
rectum |
Max DVH 4000 cGy to 10% volume |
No |
30 |
0.0027 |
Plan |
Max DVH |
femoral head R |
Max DVH 200 cGy to 10% volume |
No |
10 |
0.0020 |
Plan |
Max DVH |
femorol head L |
Max DVH 200 cGy to 10% volume |
No |
10 |
0.0034 |
Plan |
Max DVH |
uterus |
Max DVH 1000 cGy to 10% volume |
No |
30 |
0.0118 |
Plan |
Max DVH |
bladder |
Max DVH 1000 cGy to 10% volume |
No |
20 |
0.0000 |
Plan |
Max DVH |
instestine |
Max DVH 500 cGy to 10% volume |
No |
40 |
0.0000 |
Plan |
Max Dose |
DOSE |
Max Dose 3500 cGy |
No |
30 |
0.0725 |
Discussion
Blue nevi lesions similar to the case described in this paper are usually acquired conditions that frequently appear in adolescents and young adults although they can be congenital in very few cases [7,3]. They mostly appear in females and the common anatomical location include the buttocks and the scalp but previous reports have observed them in extracutaneous sites such as the oral mucosa, lymph nodes and the female genital tract [2,10-13]. To date, the distinction of ACBN from both cellular blue nevus and malignant bleus nevus still remains difficult.
Malignant Blue Nevus (MBN) is a rare, highly aggressive and lethal melanoctytic type of cancer, with a high rate of recurrence and metastatis to the lymph nodes [14,7]. Most of the cases of MBN are occur in older patients and they are in most cases associated with cellular blue nevus or other types of blue nevi but rarely with DBN [14]. Anatomically, the scalp is the most common site of MBN involvement and the average diameter of the lesions ranges from 3 to 15 cm which was different from the 1,5 cm diameter lesion located in the right gluteal region in our case [15,16]. Histopathologically, MBN is a blue black multinodular lesion characterized by fascicular dense collections of pigmented, pleomorphic spindle cells with prominent atypical nuclei, high mitotic rate (>3/mm2 ), prominent nucleoli and necrosis [15,14].
Cellular Blue Nevus (CBN), commonly affects females and adult patients under the age of 40 years [17,6]. Common sites for CBN include the buttocks, the lower back and the scalp although it can be found in many other locations [6,3]. Microsopically, CBN shows considerable histological heterogeneity of various patterns. According to [18], the multinodular cellular infiltrate of CBN is composed of oval to spindle-shaped melanocytes with pale cytoplasm alternating with bundles of spindle-shaped pigmented melanocytes. In other cases, rare mitotic activity (<1/mm2 ), focal necrosis, sclerosis and nuclear pleomorphism is usually observed in CBN [17,3]. Similiar to our case, the characteristics of CBN described in literature were also observed in our patient. Although the patient was now 59 years old, the lesion first presented itself when she was a child and started itching when she was around 39 years old. Histological features further used to distinguish between CBN and atypical CBN included the obscure boundary of the tumour, presence of numerous pigmented pleomorphic cells with various nuclear shapes and prominent nucleoli. In addition, there was necrosis, interstitial fibrosis and occasional mitotic activity, features which are usually rare to find in a typical CBN. After surgical resection and radiotherapy we did not observe any recurrence or any metastasis during the follow-up.
Immunohistochemical findings confirmed the usual findings of cellular blue nevus but it did not help to distinguish between typical and atypical CBN in this case. Based on this, it still remains that other methods to distinguish ACBN from CBN and MBN are needed. While other researchers have reported on a genetic diagnosis based on chromosomal aberrations and a tendency to recur of ACBN versus CBN it still remains that more studies supported with molecular research and long-term follow-up are required to clearly determine the morphological criteria and progression behavior of cellular blue nevi [19,20]. In conclusion, while ACBN and CBN have been described as distinct categories, it is our view that ACBN will continue to present problems to less experienced dermatopathologists since ACBN is biologically closer to CBN.
Declarations
Funding: This study was supported by 1) Guangdong Basic and Applied Basic Research Foundation (2019A1515011986) &. 2) Grant of Guangdong Medical Science and Technology Research (A2019420).
References
- Tieche M. Uber benigne Melanome (‘‘Chromatophorome’’) der Haut- ‘‘blaue Naevi’’. Virchows Arch Pathol Anat. 1906; 186: 212-229.
- Murali R, McCarthy SW, Scolyer RA. Blue nevi and related lesions: a review highlighting atypical and newly described variants, distinguishing features and diagnostic pitfalls. Adv Anat Pathol. 2009; 16: 365-382.
- Zembowicz A, Phadke PA. Blue nevi and variants: an update. Arch Pathol Lab Med. 2011; 135: 327-336.
- Ferrara G, Argenziano G. Blue nevus in Color Atlas of Melanocytic Lesions of the Skin. Springer Berlin Heidelberg. 2007; 78-86. https://doi.org/10.1007/978-3-540-35106-1_12
- Sakamoto Sachiko, Oiso Naoki, Narita Tomohiko, Kawada, Akira. Blue Nevus with a Dermoscopic Appearance of Peripheral Streaks with Branches. Case Reports in Dermatology. 2014; 6: 66-68. 10.1159/000360215.
- Tran TA, Carlson JA, Basaca PC, Mihm MC. Cellular blue nevus with atypia (atypical cellular blue nevus): a clinicopathologic study of nine cases. Journal of Cutaneous Pathology. 1998; 25: 252-258. doi:10.1111/j.1600-0560.1998.tb01729.x
- Barnhill RL, Argenyi Z, Berwick M, Duray PH, Erickson L, Guitart J, et al. Atypical cellular blue nevi (cellular blue nevi with atypical features): lack of consensus for diagnosis and distinction from cellular blue nevi and malignant melanoma (“malignant blue nevus”). Am J Surg Pathol. 2008; 32: 36-44.
- Aydingoz IE, Dikicioglu-Cetin E. Sclerosing cellular blue nevus simulating melanoma. Dermatol Online J. 2012; 18: 11.
- Cabral ES, Chen FW, Egbert BM, Swetter SM. Acquired Blue Nevi in Older Individuals. JAMA Dermatology. 2014; 150: 873
- Bautista NC, Cohen S, Anders KH. Benign melanocytic nevus cells in axillary lymph nodes. A prospective incidence and immunohistochemical study with literature review. Am J Clin Pathol. 1994; 102: 102.
- Dohse L, Ferringer T. Nodal blue nevus: a pitfall in lymph node biopsies. Journal of Cutaneous Pathology. 2010; 37: 102-104.
- Fitzhugh VA, Houck K, Heller DS. Vaginal Blue Nevus: Report of a Case and Review of the Literature. Journal of Lower Genital Tract Disease. 2011; 15: 325-327.
- Kauzman A, Rei N, Avon SL. The blue nevus: a rare lesion of the oral cavity. Gen Dent. 2014; 62: e22-26.
- Granter SR, McKee PH, Calonje E, et al. Melanoma associated with blue nevus and melanoma mimicking cellular blue nevus: a clinicopathologic study of 10 cases on the spectrum of so-called ‘‘malignant blue nevus’’. Am J Surg Pathol. 2001; 25: 316-323.
- Goldenhersh MA, Savin RC, Barnhill RL, Stenn KS. Malignant blue nevus. Case report and literature review. J Am Acad Dermatol. 1988; 19: 712-722.
- Calista D, Schianchi S, Landi C. Malignant blue nevus of the scalp. Int J. Dermatol. 1998; 37: 126-127.
- Rodriguez HA, Ackerman LV. Cellular blue nevus. Clinicopathologic study of forty-five cases. Cancer. 1968; 21: 393-405.
- International Classification of Diseases for Oncology, Sep 2011. Approved by the IARC/WHO Committee for ICD-0-3. http:// codes.iarc.fr/code/977. Accessed December 28, 2018.
- Elder DE, Murphy GF. Malignant tumors (melanomas and related lesions). In: Rosai J, ed. Atlas of Tumor Pathology: Melanocytic Tumors of the Skin. Washington, DC: Armed Forces Institute of Pathology. 1991: 177-185.
- Maize JCJr, McCalmont TH, Carlson JA, et al. Genomic analysis of blue nevi and related dermal melanocytic proliferations. Am J Surg Pathol. 2005; 29: 1214-1220.