Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
Revealing innumerable occult lesions with T1-weighted 3Dblack-blood-imaging in the detection of intracranial metastatic melanoma under BRAF therapy
Walter M Wallner1 *; Peter Koelblinger2 ; Klaus Hergan1
1Department of Radiology, Paracelsus Medical University Salzburg, Salzburg, Austria.
2 Department of Dermatology and Allergology, Paracelsus Medical University Salzburg, Salzburg, Austria.
*Corresponding Author: Walter M Wallner
Department of Radiology, Paracelsus Medical University Salzburg, Salzburg, Austria.
Tel: +43-5-7255 56107; Email: w.wallner@salk.at
Received : Oct 05, 2021
Accepted : Nov 23, 2021
Published : Nov 30, 2021
Archived : www.jcimcr.org
Copyright : © Wallner WM (2021).
Abstract
In the setting of melanoma, brain metastases are very common and contribute to a large number of different neurological deficits as well as death. In recent years, the general prognosis for patients with intracranial metastatic melanoma has improved due to progress in imaging and therapeutic management. The addition of a contrastenhanced T1-weighted MSDE sequence, a so-called Black-Blood - sequence, to the initial and follow up-scans is an excellent method to display intracranial metastatic melanoma. With this case report we want to demonstrate the possible big discrepancy in the number of metastases displayed by the Black-Blood-sequence compared to contrast enhanced T1-weighted imaging in the setting of BRAF-mutated intracranial metastatic melanoma.
Keywords: melanoma; intracranial metastatic melanoma; CNS metastasis; black-blood-imaging; MRI.
Abbreviations: 3DBB: 3D-Black Blood; ADC: Apparent Diffusion Coefficient; AJCC: American Joint Committee On Cancer; BRAF: Serin/Threonin Kinase B-RAF; Cet1bb: Contrast Enhanced T1-Weighted Black Blood Imaging; Cet1w: Contrast-Enhanced T1-Weighted Imaging; CNS: Central Nervous System; CT: Computertomography; DWI: Diffusion Weighted Imaging; FDG-PET-CT: Fluorodeoxyglucose-Positron Emission-Computer Tomography; FLAIR: Fluid-Attenuated-Inversion Recovery; MEK: Mitogen-Activated - Protein-Kinase; MRI: Magnetic Resonance Imaging; MSDE: Motion-Sensitized Driven-Equilibrium; T1- TFE: T1-Weighted Turbo Field Echo.
Citation: Wallner WM, Koelblinger P, Hergan K. Revealing innumerable occult lesions with T1-weighted 3D-black-blood-imaging in the detection of intracranial metastatic melanoma under BRAF therapy. J Clin Images Med Case Rep. 2021; 2(6): 1437.
Introduction
Intracranial metastatic melanoma is a very common entity that can increasingly be controlled as a result of improved therapeutic possibilities (immunotherapy, targeted therapy) in recent years. Management for initial and follow up imaging of the central nervous system is mostly comprised of contrast and non-contrast enhanced MRI [1]. Here, the Black Blood sequence (3DBB), which is mostly used for cardiac MRI, has led to increased attention. Research as well as routine clinical imaging for brain tumours, metastases, multiple sclerosis, aneurysms or vasculitis are the main fields for this imaging sequence [2-7].
At our institution, the 3DBB is broadly used for pediatric and adult imaging, in the course of which we are frequently encountering interesting results. One of these is demonstrated by the following case report.
Case report
We report the case of a 52 year old female patient who presented to our department for follow-up imaging of the brain in the setting of BRAF-mutated (Serin/Threonin Kinase B-RAF) AJCC stage IV melanoma. The primary melanoma was located subumbilical and first treatment consisted of in-sano excision with sentinel-lymph-node biopsy. Additional systemic therapy included adjuvant treatment with the checkpoint inhibitor nivolumab over the course of 8 months as well as combined BRAF- and mitogen-activated –protein-kinase (MEK)-inhibitor treatment for about 8 months after metastatic disease had developed.
The initial intracranial staging-MRI was unremarkable but a subsequent staging FDG-PET-CT scan revealed a suspicioussplenic and lymph nodelesion, which showed tracer-activity as well as a pulmonary metastasis, which was resected subsequently via video-assisted-thoracoscopy and histologically confirmed afterwards.
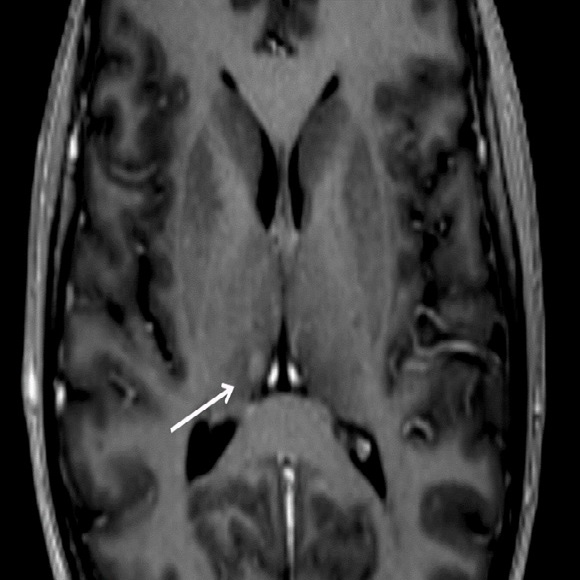
The first follow-up MRI at our department showed a cerebral progression with a metastatic lesion in the right thalamus and therefore monoclonal antibody-treatment was discontinued. (Figure 1).
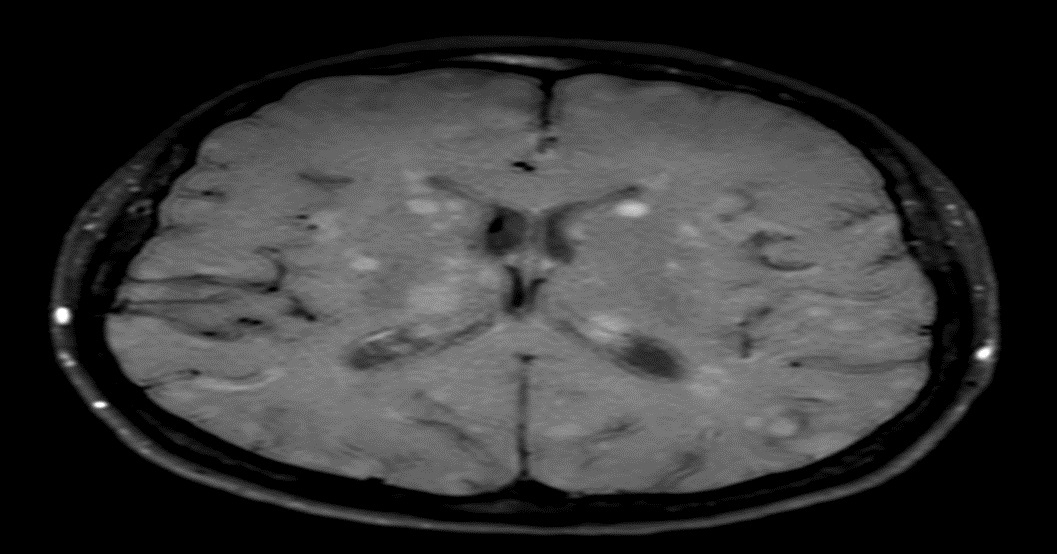
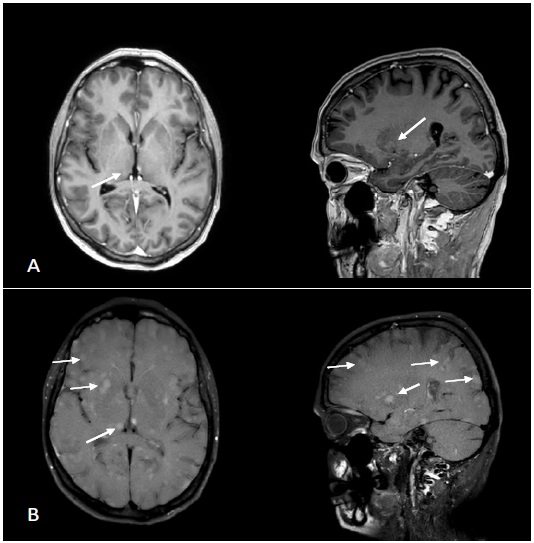
For the diagnostic work-up a 1.5 Tesla MR scanner (Philips Ingenia, Eindhoven, Netherlands) was used and the following examination was performed: Diffusion-weighted imaging (DWI) and apparent diffusion coefficient (ADC), T1-weighted fluid-attenuated inversion recovery (FLAIR), T2-weighted turbo-spin– echo (T2-TSE) unenhanced and contrast-enhanced T1-weighted TFE with multiplanar-reconstruction and a contrast-enhanced T1-weighted 3D-Black Blood sequence. The second follow-up MRI verified the lesion in the right thalamus once more and beyond that various other supra-and infratentoriallesions. To our astonishment, the contrast-enhanced-3DBB displayed the numerous additional lesions very accurately compared to the contrast-enhanced T1w-images where they remained hidden (Figure 2,3). The fact that intracranial melanoma metastases can have a miliary pattern in patients with progressive disease under BRAF-therapy could be observed earlier but the miliary pattern remains a rare manifestation [8-10]. However, to our knowledge, the discrepancy between ceT1w and ceT1BB images in the number of lesions displayed has previously not been described in the literature
Discussion
The "black blood" technique called MSDE (Motion-Sensitized Driven-Equilibrium) consists of a combination of RF pulses and gradients, acting as a black blood prepulse. MSDE has been introduced to suppress blood signal in the complete volume of interest (3D acquisitions).
The gradient strengths in three directions are the key parameter to define the degree of blood suppression. The gradient strength needed to suppress the flowing blood is also related to the blood flow velocity. Slow flowing blood requires stronger gradients to destroy the blood signal. This is achieved by either increasing the gradient amplitude or its duration or by a combination of amplitude and duration, depending on the system performance and SAR limitations. Fast flowing blood experiences larger phase shifts, and thus the blood signal can be suppressed using smaller gradient amplitude and/or shorter gradient duration. In MSDE-imaging the gradient strength relative to the flow velocity of the blood is adjusted by adapting the velocity encoding (in three directions).
The blood-flow-suppression-efficiency is linked to the gradient direction and blood flow direction. Blood flows orthogonal to the net gradient will hardly experience any phase shift and thus will not be suppressed. However, blood flowing along the gradient experiences a large phase shift and will be suppressed. In MSDE, flowing blood is suppressed prior to the imaging sequence (T1-TSE).
Therefore, this sequence consists of arterial and venous signal suppression, fat suppression and higher spatial resolution. This features show advantages after contrast-enhancement because solely those lesions avid for contrast agent are hyperintense and insignificant structures like arteries, cortical veins or fat are suppressed.
The Black-Blood-sequence for intracranial imaging differs from regular T1-weighted imaging in terms of fat suppression, the aforementioned blood-flow suppression, a slice thickness of 0,8mm ( compared to T1-TFE 1,0mm) and a voxel size of 0,8mm (compared to T1-TFE 1,0mm) which results in higher resolution of structures and soft tissue. This is an outstanding advantage compared to other sequences or imaging modalities.The limiting factor concerning the acquisition of ceT1BB-images is the acquisition time or in general the availability at the institution.
In the setting of a melanoma, the diagnostic algorithm for initial and follow-up imaging of the CNS includes non-contrast and contrast-enhanced CTorMRI respectively. However, CT has a lower diagnostic value due to its limited spatial resolution and soft-tissue contrast. In contrast, MRI is an excellent reproducible and non-invasive tool that adds valuable information regarding affected areas, which we consider essential for the early and correct diagnosis of intracranial metastases. Usually contrastenhanced T1-weighted sequences are used to display intracranial metastasis or leptomeningeal disease with excellent results [11]. However, this sequence has disadvantages regarding very small or thin leptomeningeal lesions. Gaviani et al. could show that a T2*-weighted sequence could aid some benefit but only in case of parenchymal lesions [12].
In our case, compared to regular contrast-enhanced T1w images, the ceT1BB revealed numerous additional lesions which where occult on ceT1w and displayed these countless supraand infratentoriel lesions very precisely
Conclusion
As this case demonstrates, we believe that the addition of a contrast enhanced-T1BB improves the diagnostic accuracy for the detection of otherwise occult intracranial metastatic lesions on ceT1w in the setting of melanoma under treatment. This appears to pertain in particular to melanoma treated with BRAF-/ MEK-inhibitor combinations, since a miliary pattern of cerebral metastases has been described repeatedly in this context.
Further research in this field will certainly be required, but we believe that adding a contrast enhanced-T1-Black Blood sequence in the diagnostic imaging work-up of intracranial metastatic melanoma with BRAF-mutation could improve diagnostic outcome.
Declarations
Conflict of interest: W. Wallner, P. Koelblinger and K. Hergan declare that they have no competing interests.
Funding: The authors received no financial support for the research, authorship and/or publication of this article.
Ethical standards: Informed consent was obtained from the patient for the publication of this case report and any accompanying data.
Availability of data and material: All data generated or analyzed during this study are included in this published article.
Author contributions: All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by W. Wallner, P. Koelblinger and K. Hergan. The first draft of the manuscript was written by W. Wallner and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
References
- Pope WB. Brain metastases: Neuroimaging. HandbClin Neurol. 2018; 149: 89-112.
- Oh J, Choi SH, Lee E, Shin DJ, Jo SW, Yoo RE, Kang KM, Yun TJ, Kim JH, Sohn CH. Application of 3D Fast Spin-Echo T1 Black-Blood Imaging in the Diagnosis and Prognostic Prediction of Patients with Leptomeningeal Carcinomatosis. AJNR Am J Neuroradiol. 2018; 39: 1453-1459.
- Nagao E, Yoshiura T, Hiwatashi A, Obara M, Yamashita K, Kamano H, Takayama Y, Kobayashi K, Honda H. 3D turbo spin-echo sequence with motion-sensitized driven-equilibrium preparation for detection of brain metastases on 3T MR imaging. AJNR Am J Neuroradiol. 2011; 32: 664-70.
- Younger DS. Vasculitis of the nervous system. In: Current opinion in neurology. 2004.
- Saam T, Habs M, Pollatos O, Cyran C, Pfefferkorn T, Dichgans M et al. High-resolution black-blood contrast-enhanced T1 weighted images for the diagnosis and follow-up of intracranial arteritis. Br J Radiol. 2010; 83: e182-4.
- Takano K, Hida K, Kuwabara Y, Yoshimitsu K. Intracranial arterial wall enhancement using gadolinium-enhanced 3D black-blood T1-weighted imaging. Eur J Radiol. 2017; 86: 13-9.
- Edjlali M, Roca P, Rabrait C, Naggara O, Oppenheim C. 3D fast spin-echo T1 black-blood imaging for the diagnosis of cervical artery dissection. AJNR Am J Neuroradiol. 2013; 34: E103-6.
- Haueis SA, Kränzlin P, Mangana J, Cheng PF, Urosevic-Maiwald M, Braun RP, Levesque MP, Dummer R, Goldinger SM. Does the distribution pattern of brain metastases during BRAF inhibitor therapy reflect phenotype switching? Melanoma Res. 2017; 27: 231-237.
- Hassel JC, Buder-Bakhaya K, Bender C, Zimmer L, Weide B, et al. German Dermatooncology Group (DeCOG/ADO). Progression patterns under BRAF inhibitor treatment and treatment beyond progression in patients with metastatic melanoma. Cancer Med. 2018; 7: 95-104.
- Escott EJ. A variety of appearances of malignant melanoma in the head: A review. Radiographics. 2001; 21: 625-39.
- Deike-Hofmann K, Thünemann D, Breckwoldt MO, Schwarz D, Radbruch A, Enk A, Bendszus M, Hassel J, Schlemmer HP, Bäumer P. Sensitivityof different MRI sequences in theearly detection of melanoma brainmetastases. PLoS One. 2018; 13: e0193946.
- Gaviani P, Mullins ME, Braga TA, Hedley-Whyte ET, Halpern EF, Schaefer PS, Henson JW. Improved detection of metastatic melanoma by T2*- weighted imaging. AJNR Am J Neuroradiol. 2006; 27: 605-8.