Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
Haemosuccus pancreatitis: A rare cause of GI bleed, diagnosis on CT Angiography – Case series & review of literature
Syed Sajjad AH1*; Khan Sadaf Tanaveer1; Syed Jawwad AH2
1 Assistant Professor, Department of Radiology, JIIU’s IIMSR Warudi, Badnapur, Jalna, India.
2 Associate Professor, Department of Preventive & Social Medicine, JIIU’s IIMSR Warudi, Badnapur, Jalna, India.
*Corresponding Author: Syed Sajjad AH
Sahyadri Diagnostic Centre, Vijay Nagar, opposite
CADA office, Gajanan Maharaj Mandir Road,
Aurangabad, India.
Email: Sajjadhashmi84@gmail.com
Received : Oct 13, 2021
Accepted : Nov 25, 2021
Published : Dec 02, 2021
Archived : www.jcimcr.org
Copyright : © Sajjad AH (2021).
Abstract
Haemosuccus pancreatitis also known as Pseudohaemobilia or haemoductal pancreatitis, is defined as upper gastrointestinal hemorrhage originating from the pancreatic duct into the duodenum via the Ampulla of Vater, or major pancreatic papilla.
A triad of epigastric pain, intermittent gastro intestinal bleeding and hyperamylasemia [1,2].
We present three cases of chronic pancreatitis presenting as upper GI bleed and with epigastric pain and sudden drop in Hematocrit.
One had bleed from pseudo aneurysm arising from hepatic artery leaking into pseudo cyst, second had erosion of wall of splenic vein leaking into pancreatic duct through small pseudocyst and the third patient was post cystojejunostomy with who bled into cyst, probably from a vessel in wall of cyst, well demonstrated on venous phase of CT angiography and later responded to conservative management.
Hemorrhage from the pancreatic duct, i.e. Haemosuccus Pancreaticus (HP), is a rare cause of gastrointestinal bleeding. Pancreatic Homosuccus is usually due to the rupture of an aneurysm of a visceral artery, most likely the splenic artery, in chronic pancreatitis. Other causes of HP are rare.
Keywords: haemosuccus pancreaticus; pseudo aneurysm; pancreatitic pseudocyst; upper gastrointestinal bleeding; embolization.
Citation: Sajjad AH, Tanaveer KS, Syed Jawwad AH. Haemosuccus pancreatitis: A rare cause of GI bleed, diagnosis on CT angiography – Case series & review of literature. J Clin Images Med Case Rep. 2021; 2(6): 1448.
Introduction
Hemosuccus pancreaticus occurring from pseudo aneurysm rupture into a pseudocyst is an infrequent cause of life-threatening haemorrhage. It remains a challenge in diagnosis and it should be considered in every patient with a history of chronic pancreatitis who presents with acute or intermittent gastrointestinal hemorrhage.
Hemorrhage from the papilla of Vater via the pancreatic duct, known as haemosuccus pancreaticus, is a rare cause of intermittent upper gastrointestinal bleeding. This condition was first reported in 1931 by Lower and Farrell who mentioned bleeding from an aneurysm of the splenic artery [3]. The expression “haemosuccus pancreaticus” was named by Sandblom in 1970 [4]. Until now, reports on hemosuccus pancreaticus have been quite limited. Difficulties in determining the location of bleeding sometimes cause delay of treatment and critical condition of patients.
We herein report three cases of hemosuccus pancreaticus and discuss problems and pitfalls for managing this disease.
Case presentations
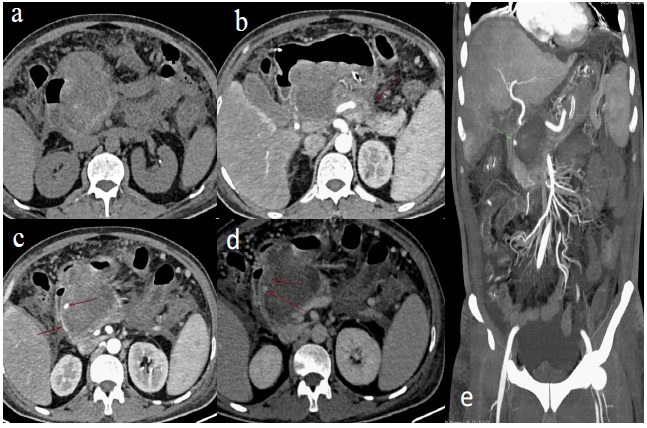
Case I
A 50 year old gentleman, chronic alcoholic with repeated episodes of pancreatitis in past, presented with intermittent episodes of haematamesis and upper abdominal pain, refereed for CT contrast study and angiography, on plain CT, there was a large pseudocyst in head region showing hyperdense contents (density 47 to 52 HU), Arterial angiography phase - Showed a small saccular aneurysm measuring 5 X 4 mm, seen in cyst wall, probably arising from branch from common hepatic artery, with free leak of contrast from aneurysm into pseudocyst on venous and delayed images. The obvious direct communication with pancreatic duct could not be established on CT images.
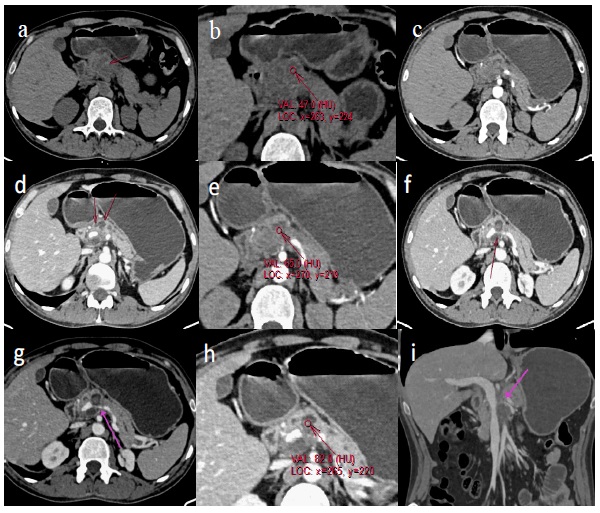
Case II
A 45 year old chronic alcoholic with past history of pancreatitis with pseudocyst presented as bleeding per rectum, dizziness and shock, on investigation found to have severe anemia on haemogram, Colonoscopy revealed fresh blood in descending and sigmoid colon. No obvious active bleeding point was identified. Upper GI scopy reveals- Traces of blood in duodenum.
Patient referred for CT angiography and CT Enterography, which revealed two small pseudo cyst, seen communicating with pancreatic duct, the lower cyst (density 23 HU) was seen closely abutting the splenic vein, just before confluence of portal vein with focal wall irregularity and increase in density of cyst contents (76 HU) on venous & delayed phase , representing leak of venous blood, from splenic vein.
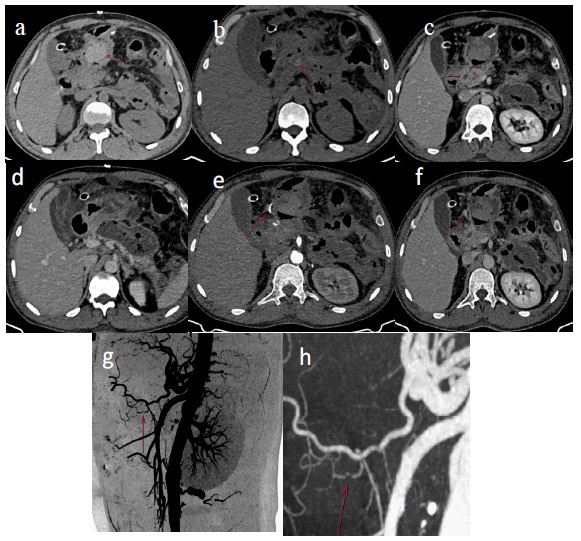
Case III
A 42 yr old gentle man having repeated episodes of pancreatitis in past, had large pseudocyst, underwent cystojejunostomy, was doing well, on day 5 of surgical procedure presented with bleeding per rectum.
Referred for emergency contrast CT, which revealed-hyperdense hemorrhagic fluid contents in cyst and pancreatic duct on plain scan (Figures 3a,b). Contrast study reveal direct communication between cyst and pancreatic duct (Figures 3c).
CT Angiographic phase shows focal wall irregularity & small blister (Figures 3 f,h,i) in branch from gastro duodenal artery along wall of cyst with adjacent focal leak on venous phase seen as fusiform hyper density (Figures 3g). Patient was managed with blood transfusion and responded well to conservatively treatment.
Discussion
Etiology & demographics
Hemosuccus pancreatitis is a rare cause of upper gastrointestinal bleeding due to hemorrhage from the ampulla of Vater via the pancreatic duct. First described by Sandblom in 1970, it occurs in approximately one in 1500 cases and is often life threatening due to massive bleeding [4,5]. It is most frequently caused by the rupture of a splenic artery pseudoaneurysm into the pancreatic duct on a background of chronic pancreatitis [6- 8]. This is thought to be due to pancreatic enzymes destroying the architecture and elastic tissue of the vessel wall leading to pseudoaneurysm formation [8]. Less frequently other peripancreatic vessels such as the gastro duodenal, pancreaticoduodenal, hepatic and left gastric arteries have been implicated [9]. A review of literature has highlighted some uncommon causes of bleeding into the pancreatic duct. Pancreatic neoplasms such as mucinous cystic neoplasm and microcystic adenomas have been identified as potential sources of bleeding [10-13]. Benign causes such as pancreatic pseudocysts and pancreatolithiasis have also been identified as causes [14,15]. Direct pancreatic injury with bleeding secondary to abdominal trauma or iatrogenic causes like biopsy have also been described in case reports [16,17]. The demographics of hemosuccus pancreatitis is not well understood due to the rarity of the condition. A review of patients over 15-years by Rammohan found a mean age of 32 and a male: female ratio of 43: 8-9 [6].
Amongst our Three patients of HP: Case 1 has rupture of common hepatic arterial pseudo aneurysm into pseudocyst., case 2 had a communication between the splenic vein with pancreatic duct via small pseudocyst and case 3 had acute hemorrhage post cysto Jejunostomy probably vessel in the wall of cyst-a branch from gastro duodenal artery.
Clinical & imaging findings
The clinical diagnosis of Haemosuccus pancreatitis is difficult due to its intermittent nature and obscured source of bleeding. Patients often present with multiple episodes of upper gastrointestinal bleeding causing melena and occasionally haematamesis [18]. There may be a characteristic intermittent crescendo-decrescendo epigastric pain, secondary to pancreatic duct distension from bleeding or a clot [19]. A history of chronic pancreatitis and chronic alcohol abuse are also associated with the diagnosis [18]. Blood tests often show chronic anemia; however liver markers, amylase and lipase levels are rarely elevated except in cases with acute pancreatitis. Upper GI endoscopy that shows fresh bleeding from the ampulla of Vater allows for a positive diagnosis [20]. However due to the intermittent nature of bleeding, blood is often noted in the duodenum with no identifiable source of bleeding. CECT imaging is very helpful in the diagnosis of hemosuccus pancreatitis. It allows for the identification of pancreatitis and pseudoaneurysms which are predisposing factors. In patients with intermittent bleeding, clotted blood within the pancreatic duct or “sentinel clot” may suggest the diagnosis [21]. In cases of active bleeding, contrast opacification of the pancreatic duct is suggestive of hemosuccus pancreatitis. The cause, size and site of bleeding into the pancreatic duct can be accurately identified to assist intervention planning. Factors that may complicate treatment such as abnormal vascular anatomy or pancreatic lesions can also be identified. Angiography is the diagnostic standard and first line therapeutic intervention for Haemosuccus pancreatitis [22,23]. It is able to detect small or intermittent bleeds into the pancreatic duct and accurately identifies the vessel involved. Vascular anatomy and collateral supply of the bleeding vessel as well as pseudo aneurysm size and features can also be evaluated.
Treatment & prognosis
The management for HP should be aimed to eradicate the source of bleeding completely. The options for hemostasis in hemosuccus pancreatitis are angiography with endovascular therapy or surgery. Angiography with coil embolization or stent placement is the preferred option in patients who are hemodynamically stable and have a demonstrable source of bleeding [24]. Covered stents retain the patency of the vessel but require enough length on both sides of the pseudoaneurysm for an adequate seal. Also, tortuosity or sharp angulations of the vessel preclude stent placement [25]. Endovascular therapy has been shown to achieve successful hemostasis in 75-100% of the cases with a low post procedure mortality [24,26]. Potential complications include bowel ischemia, splenic infarction and coil or stent migration [27]. Surgery is preferred in hemodynamically unstable patients or when angiography does not demonstrate a source of bleeding. It is also used in cases where there is failure of embolization or rebleeding after embolization. Surgical techniques vary according to the site and cause of bleed and include ligation of the bleeding vessel, pancreatic resection and bypass grafting [24]. For the patient with HP who has a pancreatic disease such as pancreatic pseudocyst, surgical treatment may be appropriate. Surgical success rates of 70-85% and operative mortality rates of 10-50% have been reported. Risk of recurrent bleeding after surgery is between 0-5% [28].
To summaries teaching points
Hemosuccus pancreatitis should be considered in the differential list for upper gastrointestinal bleeding in patients with a history of chronic pancreatitis. Contrast enhanced CT and CT Angiography on multislice CT scanner are very helpful as non invasive tool in many cases for localizing the cause and site of bleed in haemosuccus pancreatitis.
Contrast opacification of the pancreatic duct and pseudoaneurysm formation in peripancreatic vessels on contrastenhanced computed tomography imaging or angiography are characteristic imaging findings.
Interventional radiological therapy should be tried at first for HP. Only when angiography shows no abnormal findings and interventional radiological therapy is not successful, surgical treatment is considered. Intra operative ultrasonography are often performed at surgery to confirm the origin of hemorrhage.
Differential diagnosis
Haemosuccus pancreatitis presents with a clinical picture of intermittent upper gastrointestinal bleeding and chronic anemia. The differential include, Erosive gastritis, Peptic ulcer disease, Gastric carcinoma, Gastric and esophageal varices, Mallory Weiss tear, Metastatic deposits in the upper gastrointestinal tract, bleeding Diverticuli, Angiodysplasia.
Declarations
Declaration of conflict of interests: The authors declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The authors received no financial support for the research, authorship and/or publication of this article.
References
- Han B, Song ZF, Sun B. Hemosuccus pancreaticus: a rare cause of gastrointestinal bleeding. Hepatobiliary & pancreatic diseases international: HBPD INT. 11: 479-88.
- Sakorafas GH, Sarr MG, Farley DR, Que FG, Andrews JC, et al. Hemosuccus pancreaticus complicating chronic pancreatitis: an obscure cause of upper gastrointestinal bleeding. Langenbeck’s archives of surgery. 385: 124-8.
- Lower WE, Farrell JI. Aneurysm of the splenic artery: Report of a case and review of the literature. Arch Surg. 1931; 23: 182–190.
- Sandblom P. Gastrointestinal hemorrhage through the pancreatic duct. Ann Surg. 1970; 171: 61–66.
- Yu P, Gong J. Hemosuccus pancreaticus: A mini-review. Ann Med Surg (Lond). 2018; 28: 45-48.
- Toyoki Y, Hakamada K, Narumi S, Nara M, Ishido K, et al. Hemosuccus pancreaticus: problems and pitfalls in diagnosis and treatment. World J Gastroenterol. 2008; 14: 2776-2779.
- Panackel C, Kumar A, Subhalal N. Education and imaging. Hepatobiliary and pancreatic: Hemosuccus pancreaticus complicating calcific chronic pancreatitis. J. Gastroenterol. Hepatol. 2007; 22: 1691.
- Puri S, Nicholson AA, Breen DJ. Percutaneous thrombin injection for the treatment of a post-pancreatitis pseudoaneurysm. Eur Radiol. 2003; 13[suppl 4]: L79-L82.
- Rammohan A, Palaniappan R, Ramaswami S, et al. Hemosuccus Pancreaticus: 15-Year Experience from a Tertiary Care GI Bleed Centre. ISRN Radiol. 2013; 2013: 191794. PMID: 24959558.
- Shinzeki M. Mucinous cystic neoplasm of the pancreas presenting with hemosuccus pancreaticus: report of a case. Surg. Today. 2010; 40: 470-473.
- Matsumoto Y, Miyamoto H, Fukuya A. Hemosuccus pancreaticus caused by a mucinous cystic neoplasm of the pancreas. Clin. J. Gastroenterol. 2017; 10: 185-190.
- Kuruma S, Kamisawa T, Tu Y, Egawa N, Tsuruta K, et bal: Hemosuccus pancreaticus due to intraductal papillary-mucinous carcinoma of the pancreas. Clin J Gastroenterol. 2009; 2: 27-29.
- Shan YS, Sy ED, Tsai HM. Chronic hemosuccus pancreaticus: A rare complication of pancreatic microcystic adenoma successfully treated with Whipple’s procedure. Pancreas. 2000; 20: 416- 418.
- Garcea G., Krebs M., Lloyd T. Haemorrhage from pancreatic pseudocysts presenting as upper gastrointestinal haemorrhage. Asian J. Surg. 2004; 27: 137-140.
- Jakobs R, Riemann JF. Hemosuccus pancreaticus due to a pressure ulcer in pancreatolithiasis. Dtsch Med Wochenschr. 1992; 117: 1956-61.
- Kim SS, Roberts RR, Nagy KK, Joseph K, Bokhari F, An G, Barrett J. Hemosuccus pancreaticus after penetrating trauma to the abdomen. J. Trauma. 2000; 49: 948-950.
- Cheruvattath R. Hemosuccus pancreaticus after EUS-FNA of a pancreatic tail cyst. Gastrointest. Endosc. 2009; 70: 817.
- Sul HR, Lee HW, Kim JW, et al. Endovascular management of hemosuccus pancreaticus, a rare case report of gastrointestinal bleeding. BMC Gastroenterol. 2016; 16: 5.
- Inayat F, Ali NS, Khan M, Munir A, Ullah W. Hemosuccus Pancreaticus: A Great Masquerader in Patients with Upper Gastrointestinal Bleeding. Cureus. 2018; 10: e3785.
- Anil Kothari R, Leelakrishnan V, Krishnan M. Hemosuccus pancreaticus: A rare cause of gastrointestinal bleeding. Ann Gastroenterol. 2013; 26: 175-177.
- Koizumi J, Inoue S, Yonekawa H, Kunieda T. Hemosuccus pancreaticus: diagnosis with CT and MRI and treatment with transcatheter embolization. Abdom Imaging. 2002; 27: 77-81.
- De Perrot M, Berney T, Bühler L, Delgadillo X, Mentha G, Morel P. Management of bleeding pseudoaneurysms in patients with pancreatitis. British Journal of Surgery. 1999; 86: 29-32.
- Singh-Bhinder N, Kim DH, Holly BP et al. ACR Appropriateness Criteria(®) Nonvariceal Upper Gastrointestinal Bleeding. J Am Coll Radiol. 2017; 14: S177-S188.
- Barge JU, Lopera JE. Vascular complications of pancreatitis: role of interventional therapy. Korean J Radiol. 2012; 13 Suppl 1(Suppl 1): S45-S55.
- Abdelgabar A, d’Archambeau O, Maes J, Van den Brande F, Cools P, Rutsaert RR. Visceral artery pseudoaneurysms: two case reports and a review of the literature. J Med Case Rep. 2017; 11: 126.
- Saqib NU, Ray HM, Al Rstum Z, DuBose JJ, Azizzadeh A, et al. Coil embolization of a ruptured gastroduodenal artery pseudoaneurysm presenting with hemosuccus pancreaticus. J Vasc Surg Cases Innov Tech. 2020; 6(1): 67-70.
- Pitton MB, Dappa E, Jungmann F, et al. Visceral artery aneurysms: Incidence, management, and outcome analysis in a tertiary care center over one decade. Eur Radiol. 2015; 25: 2004- 2014.
- Mandaliya R, Krevsky B, Sankineni A, Walp K, Chen O. Hemosuccus Pancreaticus: A Mysterious Cause of Gastrointestinal Bleeding. Gastroenterology Res. 2014; 7: 32-37.