Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
Bilateral staged ureteral stenosis secondary to Wegener’s disease: A case report
Ramzi Mejri1*; Sami Ben Rhouma2; Yassine Nouira2
1 Department of Urology, CHU Mongi Slim La Marsa, Tunis, Tunisia.
2 Department of Urology, Hospital La Rabta, Tunis, Tunisia.
*Corresponding Author: Ramzi Mejri
Department of Urology, CHU Mongi Slim La Marsa,
Tunis, Tunisia.
Email: ramzimejrimed@yahoo.fr
Received : Oct 16, 2021
Accepted : Nov 26, 2021
Published : Dec 03, 2021
Archived : www.jcimcr.org
Copyright : © Mejri R (2021).
Abstract
Wegener’s disease is a rare vasculitis characterized by inflammation of the endometrium of blood vessels. Ureteral stenosis is a rare manifestation of granulomatosis with polyangiitis (formerly known as Wegener’s granulomatosis). We report the case of a 38-year-old woman with acute renal failure in which bilateral hydronephrosis due to staged ureteral stenosis was the second manifestation of the disease after necrotico-inflammatory skin lesions. Our patient had high titers of anti-proteinase 3 c-ANCA, but no upper or lower respiratory tract damage was demonstrated. Hydronephrosis and renal function improved rapidly under immunosuppressive therapy with high dose of corticosteroids. We reviewed the literature and found only ten other reported cases of Wegener’s granulomatosis and intrinsic ureteral stenosis: in two cases the presenting clinical manifestation was unilateral hydronephrosis and in only three others bilateral hydronephrosis. All of these complications have developed on disease relapse except in one case where the first manifestation of vasculitis is bilateral ureteral stenosis. This case highlights the importance of including ANCA-related vasculitis in the differential diagnosis of unusual cases of unilateral or bilateral ureteral stenosis.
Keywords: Wegener’s disease; ureteral stenosis; hydronephrosis; urinary drainage.
Citation: Mejri R, Rhouma SB, Nouira Y. Bilateral staged ureteral stenosis secondary to Wegener’s disease: A case report. J Clin Images Med Case Rep. 2021; 2(6): 1454.
Introduction
Wegener’s granulomatosis (WG) is a necrotizing vasculitis of the small and medium-sized vessels of unknown origin [1]. Its classic triad consists of necrotizing granulomatous vasculitis of the upper and lower respiratory tract associated with pauciimmune crescent glomerulonephritis [1]. It is frequently associated with antineutrophil cytoplasmic antibodies (ANCA) to serine proteinase 3 (PR3). It is a rare disease, with an annual incidence of approximately 10 cases per million population, a prevalence of 22-157 cases per million [2] and a peak incidence in the fourth and fifth decades of life [2]. It is a fatal vasculitis before the introduction of effective immunosuppressive treatments. The use of high-dose corticosteroids in combination with cyclophosphamide has significantly improved survival and renal function in patients with ANCA-associated vasculitis [3]. It can affect almost every organ in the body. Although rare, urogenital manifestations may occur during the course of the disease and may be minimally symptomatic [4]. Granulomatous inflammation of the prostate, bladder, penis, testes, seminal vesicles, ureters, urethra and epididymis has been reported. Localization in the retroperitoneal organs is uncommon and symptomatic ureteral involvement is exceptional. We report a case that illustrates this condition.
Case report
A 38-year-old female patient was found to be a carrier of Wegener’s disease with necrotic inflammatory skin lesions and neurological manifestations of gait disturbances, diffuse myalgia and paresthesia of both legs. The diagnosis of Wegener’s granulomatous vasculitis was evoked by the demonstration of anti-neutrophil antibodies (ANCA). A neuromuscular biopsy revealed a vasculitis of the small arterioles, establishing the diagnosis of Wagener’s disease. No renal biopsy was performed. During the acute attack, the patient received corticosteroid therapy combined with injectable immunosuppressive therapy. Three months later, the patient’s condition was excellent, her motor deficit and paresthesia progressively improved and the ANCA test was negative. After 4 months, the evolution of the disease was marked by the appearance of several episodes of bilateral low back pain. She consulted urgently with urinary retention, accompanied by bilateral back pain more accentuated on the right side, associated with proteinuria (1.5 g/l) and hematuria.
The patient was febrile at 38°C, tachycardic at 105 beats per minute. The physical examination showed a clear right lumbar fossa tenderness. Blood pressure was 100/80 mmHg.
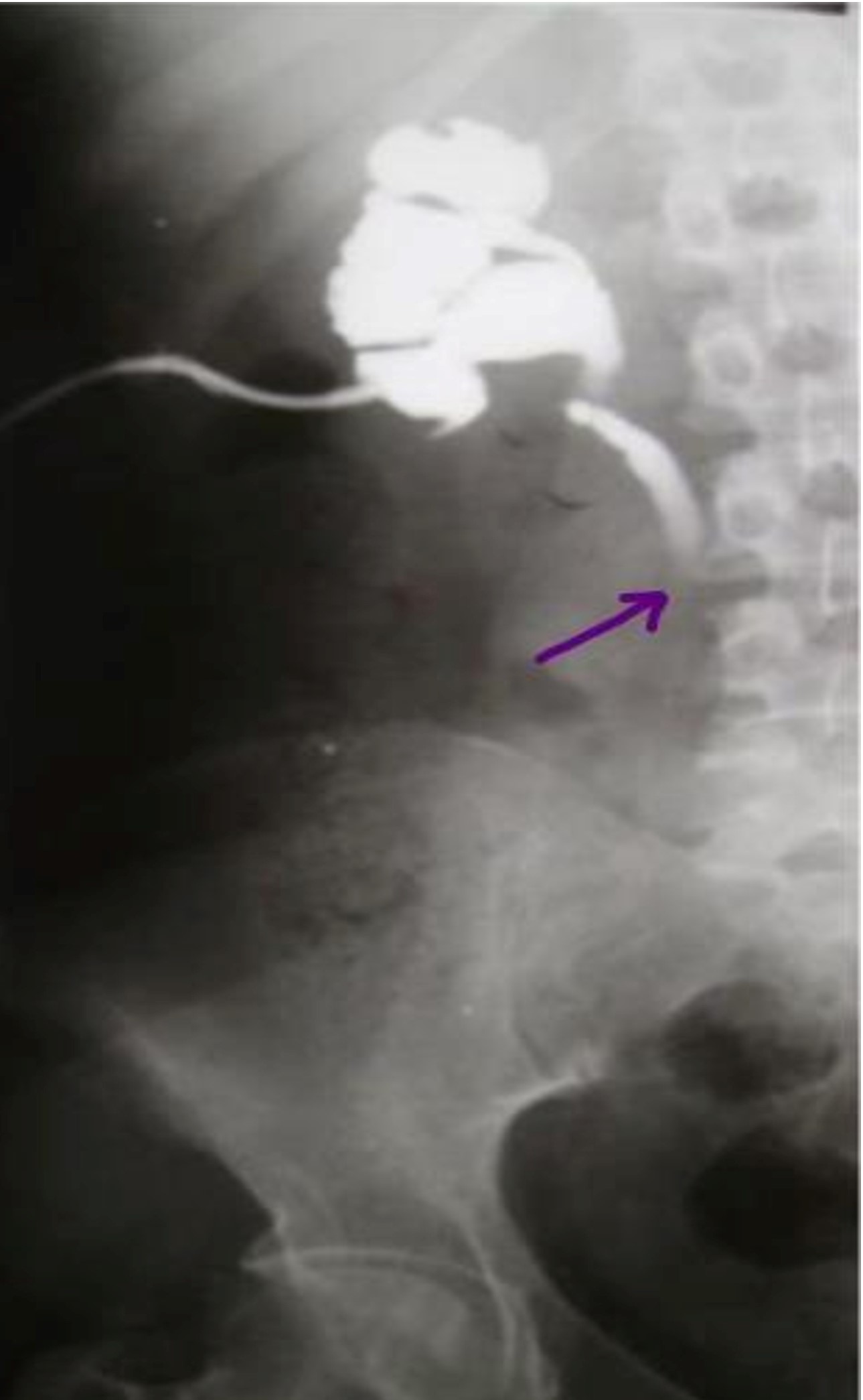
Biologically, she had an inflammatory syndrome with a hyperleukocytosis of 23,000 cells/mm3 and a CRP of 280 mg/l. Minimal renal failure with creatinine clearance of 55 ml/min. The urine was purulent and the urine cytobacteriological examination was positive for E. Coli. Ultrasound of the kidneys revealed dilatation of both collecting systems, particularly on the right side, with localized thinning of the renal parenchyma. Intravenous urography after her renal function had returned to normal (Figure 1) showed a poorly functioning right kidney and a proximal double ureteral obstruction on the left.
The patient had received intravenous antibiotic therapy adapted to her renal function and right-sided urinary drainage with a nephrostomy tube, which resulted in slightly cloudy urine. Opacification through the nephrostomy tube showed intrinsic stenosis with abrupt circumferential narrowing of the lumen (Figure 2). Abdominal CT scan showed bilateral ureteral stenosis. Cystoscopy was normal. Ureteroscopy showed narrow iliac ureteral stenosis on the right and multiple iliac and lumbar ureteral stenosis on the left with normal mucosa on both sides. Treatment with endoscopic dilatation and double J stents on the left resulted in clinical and radiological improvement, while medical treatment was continued. The patient was subsequently treated with corticosteroids and cyclophosphamide for 6 months with no evidence of recurrence. One year later, intravenous urography returned to normal and biological and clinical examinations were unremarkable.
The patient was regularly followed up at our consultation. Despite prolonged drainage of the excretory cavities by a nephrostomy tube on the left and then by a bilateral double J tube, and despite endoscopic ureteral dilatation sessions, the right renal parenchyma was destroyed, necessitating a right nephrectomy. On the left, the lesions stabilized under medical treatment.
One year later, intravenous urography returned to normal on the left and biological and clinical examinations were unremarkable.
During her hospitalization and after the end of the treatment, the patient was delighted with the care she received and seemed optimistic about the evolution of her condition despite the recourse to a nephrectomy for a destroyed kidney due to ureteral stenosis not improved by urinary drainage and combined medical treatment (corticosteroid and cyclophosphamide)
Discussion
Wegener's disease is a vasculitis of which the urogenital location remains rare, affecting the kidney, bladder, testicle and penis. Ureteral localization is exceptional, only about twenty cases have been reported in the literature [5]. Histologically Wegener's disease is characterized by non-specific inflammatory granulomas with a predominance of neutrophilic cells and areas of necrosis. These histological lesions are located in the endothelium of the target organ causing sclerosing stenosing sequelae, as in the case described in the observation, or aneurysmal arterial lesions especially in the kidney
In adults, the most common causes of bilateral ureteral obstruction are retroperitoneal or pelvic neoplasms, stones or retroperitoneal fibrosis. However, the differential diagnosis also includes other rare etiologies such as inflammatory or systemic diseases, including small and medium vessel vasculitis, can cause bilateral hydroureteronephrosis [6]. To our knowledge, we report the third case of a patient with bilateral hydronephrosis complicating ANCA-associated vasculitis.
Urogenital involvement is rare in Wagener’s disease. Large series have reported between 1% and 10% of cases of Wagener’s disease with urogenital involvement [7]. The prostate is the most common site, followed by bladder involvement, orchitis and penile ulceration [4]. When urological involvement is present, it is usually seen as part of a generalized systemic disease associated with upper respiratory tract involvement in 90-100% of cases, lung involvement in 80% and glomerulonephritis in 45- 60% [4]. Isolated urological manifestations may precede the diagnosis of Wagener’s disease in 12-18% of cases with urological involvement [7]. Intrinsic ureteral stenosis is a rare manifestation of GPA as only 12 cases (including ours) have been reported in the literature to date [7,8].
The definitive diagnosis of Wegener's disease in the ureter is a histological diagnosis made on biopsy material from the affected organ. The diagnosis of this disease has been facilitated in recent years by the immunohistochemical test for anti-neutrophil cytoplasm antibody (ANCA).
The clinical manifestation of these lesions is multiple stenoses, often very tight, bilateral, evolving by flare-ups. Combination therapy with glucocorticoids and cyclophosphamide is the basic treatment for Wegener’s disease [9]. A decisive step towards the treatment of WG has been the development of a stepwise induction-maintenance strategy that reduces the cumulative exposure to cyclophosphamide. This strategy uses cyclophosphamide to induce remission, followed by a less toxic immunosuppressant such as azathioprine or methotrexate [10]. This regimen resulted in partial or complete remission in 91% and 75% of patients, respectively [11]. Urogenital manifestations respond rapidly to treatment with cyclophosphamide and glucocorticoids, and most urogenital manifestations can be resolved rapidly with pharmaceutical treatment, although some patients require surgical interventions due to persistent symptoms after receiving immunosuppressants, as in our case a right nephrectomy was performed due to the unresponsiveness of the right kidney to treatment. According to studies, one third of patients had a urogenital relapse during maintenance treatment.
The treatment of these advanced stenoses is disappointing because they progress quietly and the diagnosis is made at a scarred stage. Immunosuppressive therapy has not shown any benefit in our case, perhaps due to delayed diagnosis.
Conclusion
Symptomatic urogenital involvement is a rare feature of WG, but is probably underestimated as it is difficult to diagnose in some cases such as ureteral stenosis. ANCA-related vasculitis should be considered in the differential diagnosis of unusual cases of unilateral or bilateral ureteral stenosis and ANCA testing should be performed in patients in whom a diagnosis is not obvious
Urogenital symptoms appear to be very sensitive to cyclophosphamide and corticosteroid therapy. One third of patients had a urogenital relapse during maintenance therapy. Surgical interventions may be useful in patients with persistent symptoms or forms that do not respond to medical treatment.
Declarations
Conflicts of interest: The authors declare that they have no conflicting financial or personal interests.
Consent: Informed consent was obtained from the patient for us to use the images. She voluntarily gave her informed consent to allow the authors to use her photos for this case report.
Authors' contributions: RM, KC and MB were responsible for the diagnosis and clinical management of the patient. RM drafted the manuscript. SBR participated in the analysis, supervision, writing of the original draft, revision and editing of the manuscript for intellectual content. All authors read and approved the final manuscript.
References
- Jennette JC, Falk RJ, Andrassy K, et al. Nomenclature of systemic Vasculitides. Arthritis & Rheumatism. 1994; 37: 187-192.
- Jennette JC, Nachman PH. ANCA glomerulonephritis and vasculitis. Clinical Journal of the American Society of Nephrology. 2017; 12: 1680-1691.
- Comarmond C, Cacoub P. Granulomatosis with polyangiitis (Wegener): clinical aspects and treatment. Autoimmunity Reviews. 2014; 13: 1121-1125.
- Alba MA, Moreno-Palacios J, Beça S, Cid MC. Urologic and male genital manifestations of granulomatosis with polyangiitis. Autoimmunity Reviews. 2015; 14: 897-902.
- Davenport A, Downey SE, Goel S, Maciver AG. Wegener’s granulomatosis involving the urogenital tract. Br J Urol. 1996; 78: 354- 7.
- Suillot J, Bollmann J, Rotman S, Descombes E. Bilateral Ureteral Stenosis with Hydronephrosis as First Manifestation of Granulomatosis with Polyangiitis (Wegener’s Granulomatosis): A Case Report and Review of the Literature. Case Rep Nephrol. 2020; 2020: 7189497.
- Dufour JF, Le Gallou T, Cordier JF, Aumaître O, Pinède L, et al. Urogenital manifestations in Wegener granulomatosis: Astudy of 11 cases and review of the literature. Medicine (Baltimore). 2012; 91: 67-74.
- Lillaz J, Bernardini S, Algros MP, Bittard H, Kleinclauss F. Wegener’s granulomatosis: a rare cause of hydronephrosis. Case Reports in Medicine. 2011; 2011: 3.
- Carruthers D, Sherlock J. Evidence-based management of ANCA vasculitis. Best Pract Res Clin Rheumatol. 2009; 23: 367-378.
- Pagnoux C, Mahr A, Hamidou MA, Boffa JJ, Ruivard M, et al. Azathioprine or methotrexate maintenance for ANCA-associated vasculitis. N Engl J Med. 2008; 359: 2790–2803.
- Hoffman GS, Kerr GS, Leavitt RY, Hallahan CW, Lebovics RS, et al. Wegener granulomatosis: An analysis of 158 patients. Ann Intern Med. 1992; 116: 488-498.