Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
Injection of methylene blue in the lungs during laparoscopic cholecystectomy
Brouna Abou Jaoude; Hazem Kafrouni*
University of Balamand, Saint George Hospital University Medical Center, Department of Anesthesiology, Beirut 1100-2807, Lebanon.
*Corresponding Author: Hazem Kafrouni
University of Balamand, Saint George Hospital
University Medical Center, Department of
Anesthesiology, Beirut 1100 2807, Lebanon.
Email: hazemkafrouni@yahoo.com
Received : Oct 17, 2021
Accepted : Nov 29, 2021
Published : Dec 06, 2021
Archived : www.jcimcr.org
Copyright : © Kafrouni H (2021).
Abstract
In a surgical setting, intraoperative methylene blue usage is a safe and effective technique in detecting gastric leak during laparoscopic abdominal surgery [1]. A Nasogastric (NG) tube is commonly used to empty the stomach and to monitor the occurrence of bowel occlusion after major abdominal surgery. The incidence of misplacement of NG tubes into the airways ranges between 0.3% and 15% [2] and is associated with significant morbidity and mortality [3].
A 68-year-old male patient presented to the operating room for scheduled laparoscopic cholecystectomy. After tracheal intubation and commencement of surgery, an 18 Fr. NG tube was inserted blindly through the nostril with no means of assessing its position. A solution of methylene blue was prepared and 240 ml were injected in the NG tube. Upon applying negative pressure suction on the NG, a noticeable change in airway pressure was noted and investigation through the use of fiber optic vision revealed the presence of bluish liquid in the bronchi. The NG tube was then re-inserted, the surgeon made the final confirmation of its proper placement within the stomach and the surgery continued uneventfully. Postoperative chest x-ray was suggestive of hypersensitivity pneumonitis and emphysema. Patient was first admitted to the intensive care unit where treatment was initiated, to be then transferred to the ward and later discharged on post-operative day three.
Keywords: laparoscopic cholecystectomy; methylene blue; nasogastric tube; hypersensitivity pneumonitis; emphysema.
Citation: Jaoude BA, Kafrouni H. Injection of methylene blue in the lungs during laparoscopic cholecystectomy. J Clin Images Med Case Rep. 2021; 2(6): 1455.
Introduction
In a surgical setting, intraoperative methylene blue usage is a safe and effective technique in detecting gastric leak during laparoscopic abdominal surgery [1]. A Nasogastric (NG) tube is commonly used to empty the stomach and to monitor the occurrence of bowel occlusion after major abdominal surgery. The incidence of misplacement of NG tubes into the airways ranges between 0.3% and 15% [2] and is associated with significant morbidity and mortality, as seen in the review of the literature [3].
The following case report is of a 68-year-old patient undergoing laparoscopic cholecystectomy, who was subject to intraoperative blind misplacement of nasogastric tube into the trachea and injection of 240 ml of methylene blue solution leading to airway pressure changes, postoperative hypersensitivity pneumonitis and emphysema. Patient was immediately started on treatment and follow-up supportive care. By highlighting this occurrence, we hope to increase clinical awareness of the risks of intraoperative blind nasogastric tube insertion and the high occurrence of misplacement as well as the dangers of accidental methylene blue injection in the lungs.
Case presentation
A 68-year-old male patient known to have diabetes mellitus II (HbA1c 6) and a history of gallstones presented to the operating room for scheduled laparoscopic cholecystectomy. History goes back to one day prior to presentation when the patient started complaining of right upper quadrant pain lasting for one hour then spontaneously relieved. On the day of presentation, the patient suffered from epigastric and right upper quadrant pain radiating to the right scapula increasing in intensity. Patient also reported diaphoresis, while denying nausea, vomiting, diarrhea, fever or chills. On physical examination, the abdomen was soft, non-distended with positive bowel sounds. Murphy and Mc Burney signs were negative. A CT scan of the abdomen was performed after IV contrast administration showing; a distended gallbladder with thickened walls and multiple gallstones the largest 18 X 15 mm, fluid around the gallbladder and fat streaking, and a 6 mm calculus in the common bile duct but no distention of the duct. The findings were compatible with acute calculus cholecystitis. ERCP was done on day 4 of hospitalization and laparoscopic cholecystectomy was scheduled the next day. Patient was studied preoperatively with complete investigations, a multidisciplinary workup including specialist counseling (gastroenterology, anesthesiology, cardiology, and endocrinology), and complete performance status evaluation. On physical examination, he had clear auscultation of the lungs, good bilateral air entry with no adventitious sounds. Chest radiography depicted infiltrates in the lingual, otherwise clear and a cardiac index within normal range. Patient was well informed about the surgical procedure, including all possible complications.
Patient presented to the operating room after fasting for more than 6 hours. General anesthesia was administered; endotracheal tube size 8.5 was inserted under vision with its cuff inflated (approximately 7 cc’s of air). Chest auscultation was done and found to be bilateral, symmetrical and clear. The tube was then secured in place (22 cm mark) and the eyes protected. The stomach was decompressed using a suction catheter 18 French, 53 cm and left in place under free drainage. Dexamethasone 8 mg and ranitidine 50 mg were administered intravenously as Postoperative Nausea and Vomiting (PONV) prophylaxis. Surgery was started through laparoscopy and adhesions were first noted around the gallbladder requiring excessive dissection. The gallbladder was then removed and the surgeon requested insertion of a Nasogastric (NG) tube to verify the integrity of the stomach by injecting methylene blue tinted solution. The suction catheter was removed and NG tube 18 French was inserted through the nostril. No difficulty or obstruction was encountered. Since the surgery was in progress and sterility established, the position of the NG tube could not be confirmed. A solution of methylene blue (1% 100 mg 10 ml vial diluted in 1000 ml sterile water) was prepared and 240 ml of the solution was injected by increments of 60 ml in the NG tube. The surgeon declined distention of the stomach. Upon applying negative pressure suction on the NG tube, no fluid was collected but a decrease in airway pressure was noted. Therefore suspicion was raised about the position of the NG tube being in the lungs instead of the stomach. The NG tube was removed, and fiber optic vision of bluish liquid in the bronchi confirmed suspicions. The patient’s oxygen saturation did not decrease from baseline and vitals remained stable. Anterior auscultation of the chest was clear and negative for adventitious sounds. Hydrocortisone 100 mg intravenous was administered as prophylaxis. An orogastric tube 18 French was then inserted and the injection of air distended the stomach as seen by the surgeon confirming proper positioning of the tube. Injection of 60 ml of the methylene blue solution followed and integrity of the stomach was verified and the surgery concluded. The patient was then awakened and extubated after spontaneous breathing with good volumes and 100% saturation with clear lungs on auscultation. The patient’s vitals remained stable as he was transferred to the Post Anesthesia Care Unit (PACU).
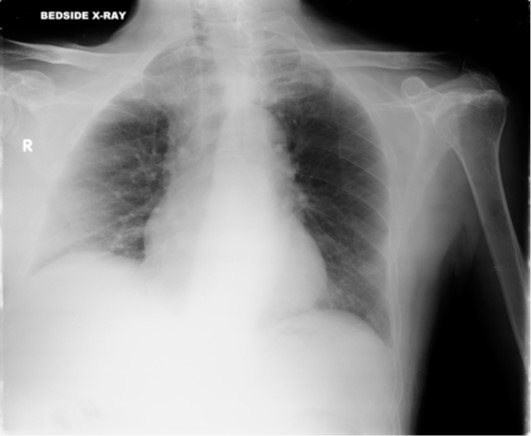
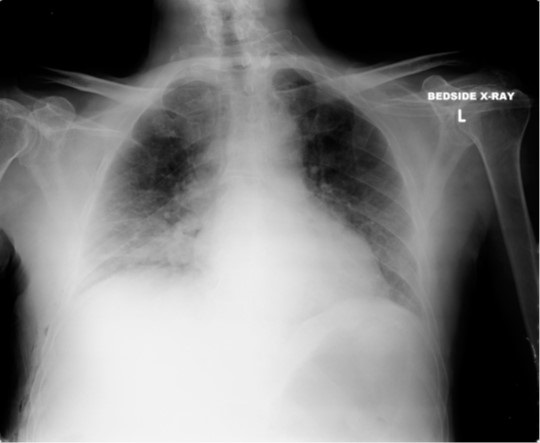
In the PACU the patient was put on facemask 5 L oxygen to increase his saturation from 90% to 99%. Immediate post-operative chest X-ray (Figure 1 & 2) was done in the PACU showing congested lungs, infiltrates in the right base and soft tissue emphysema on the right at the level of the lower chest and abdomen. The patient was transferred to the intensive care unit for monitoring and was started on prophylactic treatment for hypersensitivity pneumonitis after further examination.
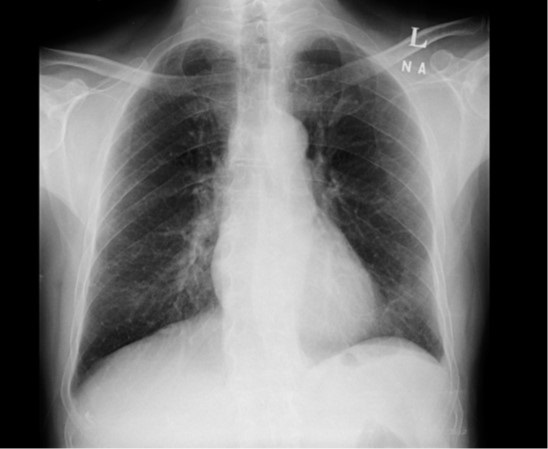
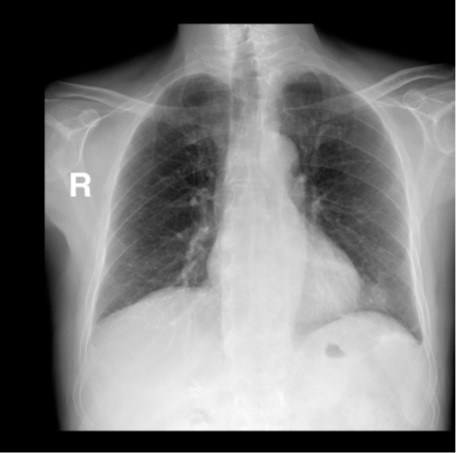
Another chest x-ray (Figure 3) done later that same day showed; a decrease in the right basal infiltrates and soft tissue emphysema, and so the patient was taken off oxygen supplementation. The next day, the chest x-ray (Figure 4) showed a further decrease in infiltrates. The patient’s laboratory work-up was improving with a significant decrease in white blood cell count and CPR level. Therefore the patient was transferred to the regular ward where he resided for two more days. The consequent chest radiographs (Figure 5 & 6) showed no active lung infiltrates and the patient was discharged home on postoperative day three.
Discussion
Review of the literature sheds light on the different complications and risk factors that are associated with blind tube insertion, and evaluates the validity of correct placement verification methods. Patients are exposed to potentially serious morbidity and mortality from blindly inserted NG tubes. It has been associated with numerous adverse outcomes such as aspiration pneumonia, nasal mucosal bleeding, intracranial placement, esophageal and other enteric perforation, hypertension, tachycardia, arrhythmia, bronchial placement, pneumothorax, hydrothorax, empyema, and vascular penetration [5-7]. Risk factors associated with malposition include blind insertion, the presence of endotracheal tubes, altered sensorium, and previous tube misplacements [8]. The National Patient Safety Agency (NPSA) issued guidelines for NG tube insertion with a list of recommended tests to confirm correct gastric position [9]. It included measuring the acidity/alkalinity of aspirate (stomach contents) using pH indicator strips in the range 0 to 6 and radiography, emphasizing the inaccuracy of other tests still in use such as the “whoosh” test, and monitoring for bubbling at the proximal end of the tube because the stomach also contains air and could falsely indicate respiratory placement [9]. Tackling the incidence of injecting profuse amounts of methylene blue solution into the lungs, no literature was found but rather some studies on injecting minute amounts of methylene blue for localization of pulmonary nodules, staining technique for identifying intersegmental planes, and retrograde instillation during bronchoscopy for diagnoses of bronchopleural fistula [10-12]. We came upon only one similar case report with the injection of 150 ml of methylene blue stain into the lungs during gastric bypass to check for the absence of digestive fistula [12]. Patient management and outcome was briefly discussed, with the use of ultrasound for diagnosis of NG tube misplacement into the trachea [12].
We report this case due to its rare incidence, favorable outcome and potential in illustrating the importance of proper verification of NG tube placement.
Conclusion
Methylene blue staining may be used to identify tissues in the lungs but the frank injection of copious quantities of the solution in the lungs is not standard practice. The consequences of such an act were not extendedly reported in the literature so far.
In this case, the accidental injection of a rather large volume of methylene blue solution into the lungs did not lead to deterioration in the ventilatory status of the patient. Nonetheless radiologic signs lead to a high suspicion of hypersensitivity pneumonitis that was successfully treated in a few days without any sequelae.
Declarations
Consent: Written consent was obtained from the patient for this case report.
Conflict of interest: The authors declare that there are no conflicts of interest.
References
- Abdul Raheem O, Yousef M, Saleem Mohran A, Abdallah H and Gaber A. The role of methylene blue in laparoscopic sleeve gastrectomy. Al Azhar Assiut Medical Journal. 2016; 14: 122.
- Rassias A, Ball P and Corwin H. A prospective study of tracheopulmonary complications associated with the placement of narrow-bore enteral feeding tubes. Critical Care. 1998; 2: 25.
- Pillai J. Thoracic complications of nasogastric tube: Review of safe practice. Interactive CardioVascular and Thoracic Surgery. 2005; 4: 429-433.
- Kerforne T, Chaillan M, Geraud L and Mimoz O. Ultrasound diagnosis of nasogastric tube misplacement into the trachea during bypass surgery. British Journal of Anaesthesia. 2013; 111: 1032- 1033.
- Hung C and Lee W. A novel method to assist nasogastric tube insertion. Emergency Medicine Journal. 2008; 25: 23-25.
- Bautista E. Complications of Nasogastric Tube Insertion. Chest. 1988; 93: 1119- 1120.
- Fassoulaki A and Athanassiou E. Cardiovascular responses to the insertion of nasogastric tubes during general anaesthesia. Canadian Anaesthetists’ Society Journal. 1985; 32: 651-653.
- Long M, Machan M and Tollinche L. Intraoperative Gastric Tube Intubation: A Summary of Case Studies and Review of the Literature. Open Journal of Anesthesiology. 2017; 07: pp.43-62.
- Nnng.org.uk. Good Practice Guideline Safe Insertion of Nasogastric (NG) Feeding Tubes in Adults. 2018.
- Wicky S, Mayor B, Cuttat J and Schnyder P. CT-Guided Localizations of Pulmonary Nodules With Methylene Blue Injections for Thoracoscopic Resections. Chest. 1994; 106: 1326-1328.
- Zhang Z, Liao Y, Ai B and Liu C. Methylene Blue Staining: A New Technique for Identifying Intersegmental Planes in Anatomic Segmentectomy. The Annals of Thoracic Surgery. 2015; 99: 238- 242.
- Kerforne T, Chaillan M, Geraud L and Mimoz O. Ultrasound diagnosis of nasogastric tube misplacement into the trachea during bypass surgery. British Journal of Anaesthesia. 2013; 111: 1032- 1033.
- Martin T and Aunspaugh J. The “Other Tube” in the Airway. Anesthesia & Analgesia. 2014; 118, 501-503.
- Ozer S and Benumof J. Oro and Nasogastric Tube Passage in Intubated Patients: Fiberoptic Description of Where They Go at the Laryngeal Level and How to Make Them Enter the Esophagus. Survey of Anesthesiology. 2000; 44: 175-176.
- Vijayakumar V, Velusamy P and Govindarajulu D. Common source but a rare cause for intraoperative breathing circuit leak: Every anaesthesiologist should be aware of. Indian Journal of Anaesthesia. 2014; 58: 495.
- Sahu A. and Baliarsing L. Unusual Cause of Sudden Collapse of Reservoir Bag during Positive Pressure Ventilation. Bombay Hospital Journal. 2018.
- Kalava A, Clark K, McIntyre J, Yarmush J, Lizardo T, et al. Mistaken Endobronchial Placement of a Nasogastric Tube During Mandibular Fracture Surgery. Anesthesia Progress. 2015; 62: 114-117.