Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
Posttraumatic intradural caroticocavernous fistula
Marco Antonio Stefani*; Eduarda Tanus Stefani; Mariana Tanus Stefani
Department of Neurosurgery, Hospital de Clinicas de Porto Alegre, Federal University of Rio Grande do Sul, Porto Alegre, Brazil.
*Corresponding Author: Marco A Stefani
Department of Neurosurgery, Hospital de Clinicas de
Porto Alegre, Federal University of Rio Grande do Sul,
Porto Alegre, Brazil
Email: mstefani@hcpa.edu.br
Received : Oct 16, 2021
Accepted : Dec 03, 2021
Published : Dec 10, 2021
Archived : www.jcimcr.org
Copyright : © Stefani MA (2021).
Abstract
Posttraumatic Caricocavernous Fistulas (CCf) occur in the intracavernous segment of the internal carotid artery. The authors present an unique case where the CCf developed in the intradural segment of the internal carotid artery. The clinical course and treatment employed are also presented and possible mechanisms for this rare situation are discussed.
Keywords: cerebrovascular disorders; vascular malformations; head injury; angiography; embolization.
Abbreviations: CCf: Caroticocavernous Fistula; CT: Computed Tomography; DSA: Digital Subtraction Angiography; ICA: Internal Carotid Artery
Citation: Stefani MA, Stefani ET, Stefani MT. Posttraumatic intradural caroticocavernous fistula. J Clin Images Med Case Rep. 2021; 2(6): 1466.
Introduction
Intradural CCf is a very rare condition and has been reported in association with craniofacial injuries [1-4]. The mechanism of formation of these arteriovenous fistula is unknown, but it may involve the traumatic rupture of the cavernous sinus’ superior dural wall with subsequent communication between the ICA and the cavernous sinus [5]. The authors present a rare case where the CCf was created in the intradural segment of the ICA.
Case report
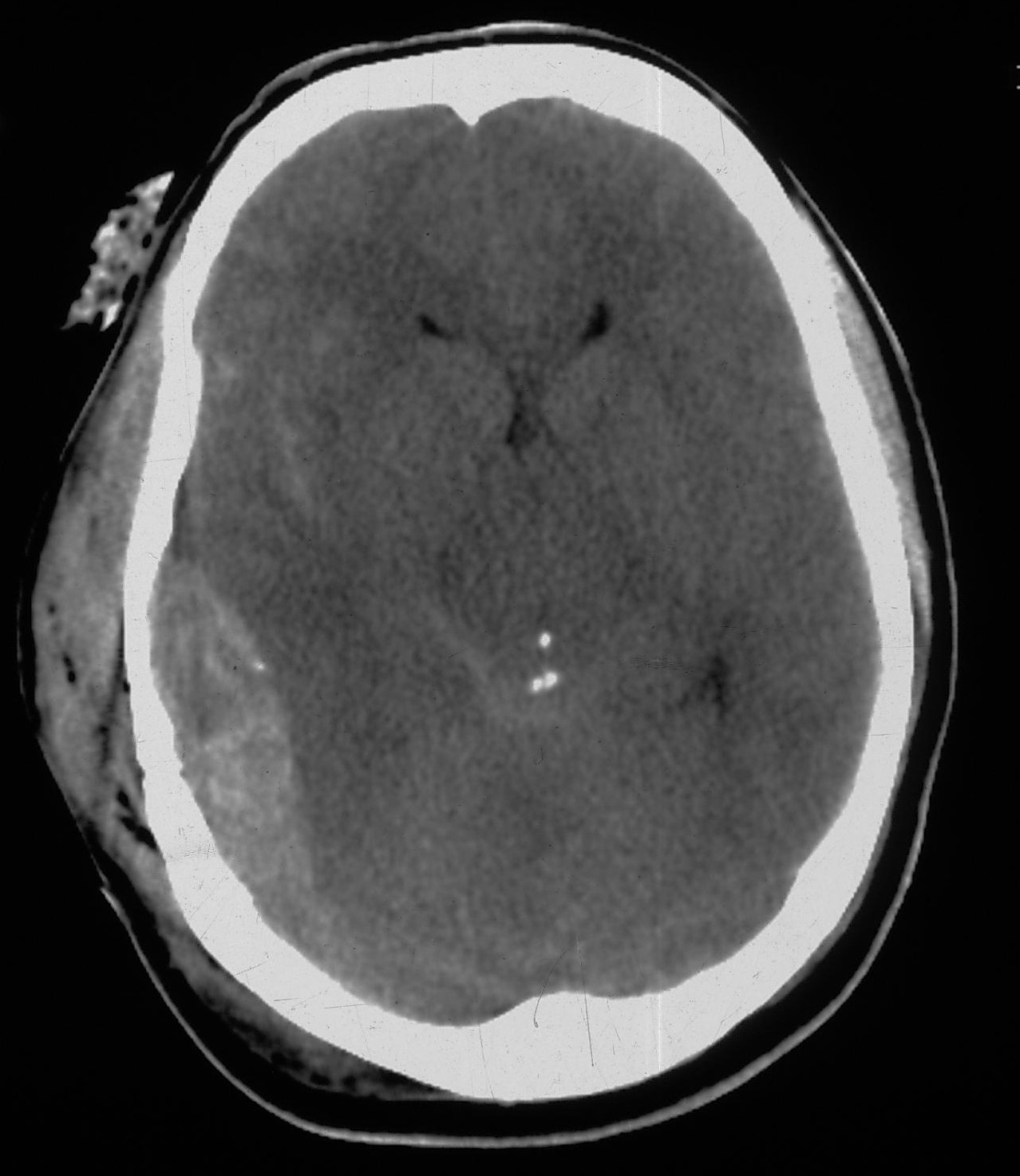
A 35-year-old man was admitted to the emergency room of a tertiary trauma center after sustaining severe head injury in a motor vehicle accident. He was admitted confused and the Skull radiogram revealed a large temporoparietal fracture. The initial Computed Tomography (CT) showed the presence of an epidural hematoma and diffuse subarachnoid hemorrhage (Figure 1A). The patient was submitted to hematoma evacuation and remained 30 days in intensive care, with progressive neurologic improvement, being discharged to ambulatory care alert and cooperative, without neurologic deficits. The patient started to present vascular congestion in the right eye and some degree of proptosis eight months after the discharge. The hypotheses of CCf was raised and confirmed after a CT angiography.
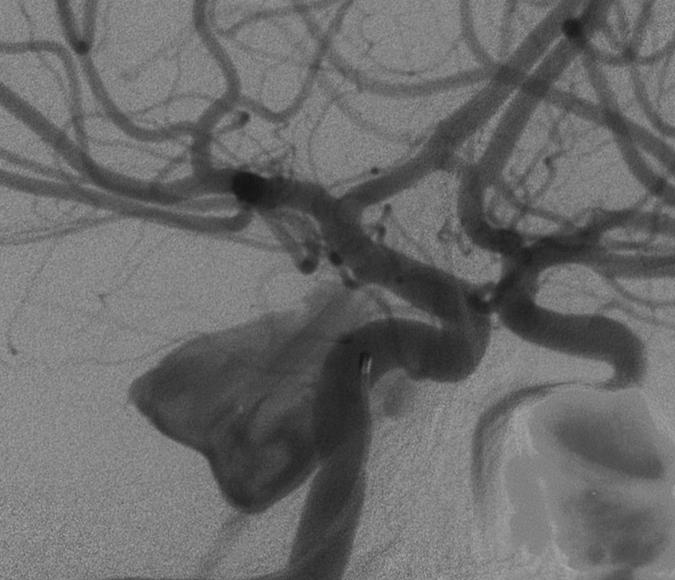
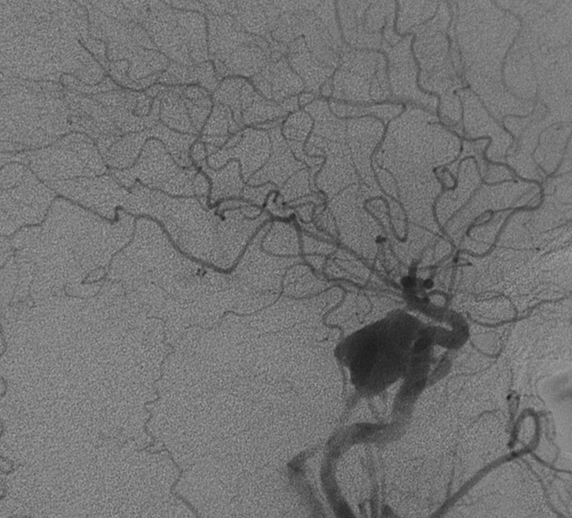
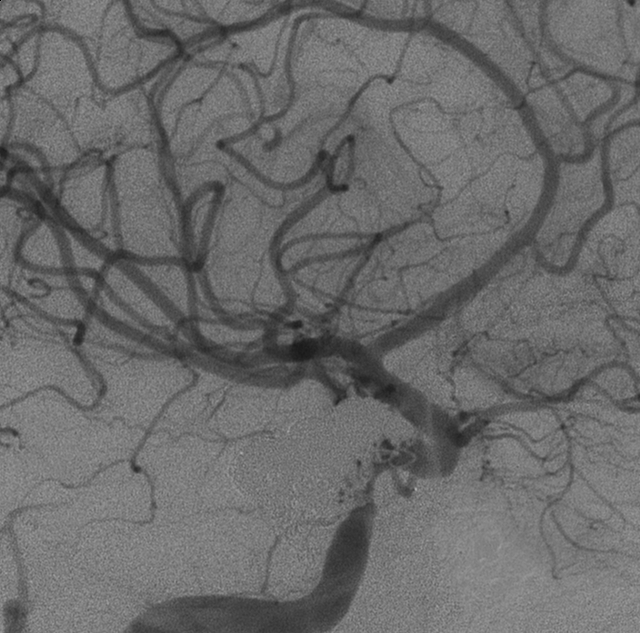
The patient was hospitalized for endovascular treatment and a direct carotid-cavernous fistula located in the internal carotid artery’s intradural segment was noticed during the angiogram, with a small arterial communication draining directly into a large paraclinoid venous pouch (Figure 1B). The ICA rupture was located close to the posterior communicating artery’s origin and the venous sac drained toward the ophthalmic vein and inferior petrosal sinus (Figure 1C). Balloon occlusion was not considered suitable due to the large size of the venous sac and the arterial route was chosen. A micro catheter was advanced into the shunt and 20 platinum coils were placed until the complete occlusion of the fistula (Figure 1D).
Discussion
Caroticocavernous fistulas are frequently associated with craniofacial trauma and in the majority of the cases involve the intracavernous segment of the ICA. Only five case of intradural CCf have been reported in the literature [1,5]. In the set of a head injury with laceration of the intradural ICA, the subsequent subarachnoid hemorrhage would be massive and probably fatal. When there is a traumatic rupture of the cavernous sinus’ superior dural wall and associated traumatic dissection from the injured ICA, a late communication between the two compartments may occur, with the clinical picture related to the increased pressure in the cavernous sinus [5].
Different treatment strategies have been advocated, with most cases being successfully treated by endovascular approaches. The best option for treatment is unclear and the management should be individualized. The arterial route remains an option when the arterial defect is small and the coils can be safely placed.
One of the main concerns for endovascular treatment is whether or not the intradural ICA wall would have the necessary resistance to allow intraluminar navigation with the microcatheter and microguide wire and to accommodate coils or balloons. The rupture of a false intradural ICA wall would represent a major neurological catastrophe, with significant risk of immediate mortality. In the present case, the endovascular treatment was uneventful and coils were placed safely. The scar tissue surrounding the injured ICA may have played a protective role, preventing arterial rupture, and subsequent pseudoaneurismal formation.
Acknowledgements: The authors have no conflict of interest.
References
- Fu Y, Ohata K, Tsuyuguchi N, Hara M. Direct surgery for posttraumatic carotid-cavernous fistula as a result of an intradural pseudoaneurysm: case report. Neurosurgery. 2002; 51: 1071-1073.
- Masana Y, Taneda M. Direct approach to a traumatic giant internal carotid artery aneurysm associated with a carotid-cavernous fistula. Case report. J Neurosurg. 1992; 76: 524-527.
- Kinugasa K, Higashi H, Ohmoto T. Fistula of the posterior communicating artery and cavernous sinus. AJNR Am J Neuroradiol. 1995; 16: 1626-1628.
- Weaver KD, Ewend MG, Solander S. Successful transarterial Guglielmi detachable coil embolization of posttraumatic posterior communicating artery-cavernous sinus fistula: technical note. Neurosurgery. 2003; 52: 458-460.
- Oran I, Parildar M, Memis A, Dalbasti T. Posttraumatic intradural internal carotid artery-cavernous sinus fistula associated with ipsilateral carotid dissection. Transarterial embolization with detachable coils. Interv Neuroradiol. 2004; 10: 63-68.