Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
Non-traumatic spontaneous spinal intradural extramedullary hemorrhage (SIEH) associated with rivaroxaban
David Siu Kei Mak; Yu Tung Lo*; Ji Min Ling; Nolan Colum
Department of Neurosurgery, National Neuroscience Institute, Singapore.
*Corresponding Author: Yu Tung Lo
Department of Neurosurgery, National Neuroscience
Institute, 1 Jln Tan Tock Seng, Level 1, Singapore
308433.
Email: yutung.lo@mohh.com.sg
Received : Oct 21, 2021
Accepted : Dec 10, 2021
Published : Dec 17, 2021
Archived : www.jcimcr.org
Copyright : © Lo YT (2021).
Abstract
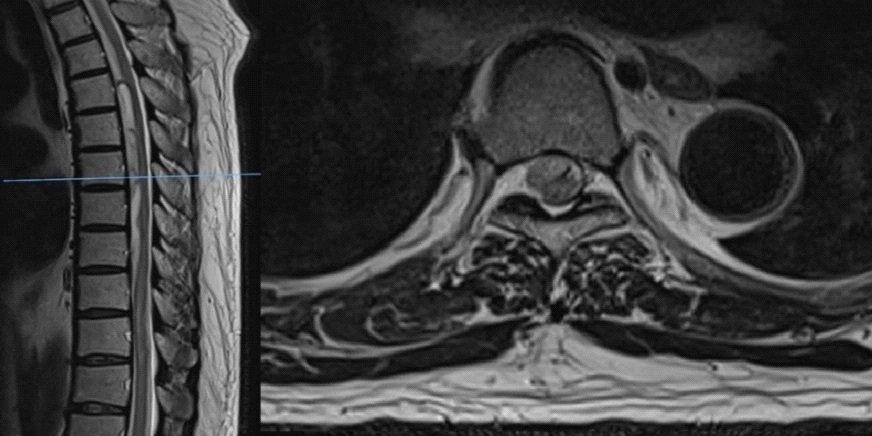
Non-traumatic Spontaneous Intradural-Extramedullary Hematoma (SIEH) is a rare condition. Rivaroxaban is a Novel Oral Anticoagulant (NOAC), and there are few reports of rivaroxaban-associated SIEH. We report a 72-year-old male who had been taking rivaroxaban for his atrial fibrillation. He presented with sudden-onset paraplegia with a T7 sensory level and absent anal contraction. Magnetic resonance images of the spine revealed a long-segment T4-T8 ventral intradural extramedullary hematoma and T9-T10 dorsal intradural extramedullary hematoma both causing cord compression, associated with spinal cord oedema spanning from T8-T10 levels. To address the acute spinal cord compression, T4 to T10 laminectomy and evacuation of SIEH was performed for urgent spinal cord decompression. Sixteen months post-operation, he was able to ambulate independently albeit with residual bilateral lower limb weakness and numbness.
Keywords: SIEH; spinal hematoma; laminectomy; hematoma evacuation; rivaroxaban; NOAC.
Citation: Mak DSK, Lo YT, Ling JM, Colum N. Non-traumatic spontaneous spinal intradural extramedullary hemorrhage (SIEH) associated with rivaroxaban. J Clin Images Med Case Rep. 2021; 2(6): 1489.
Introduction
Non-traumatic spinal subdural hematoma is extremely rare with an uncertain prognosis. It is often impossible to differentiate among a subdural, subarachnoid, or mixed pattern, hence the term Spinal Intradural-Extramedullary Hematoma (SIEH) was proposed by Hausmann et al [1].
Coagulopathy-related spontaneous SIEH is one of the considerations in cases of sudden onset non-traumatic paraparesis as a result of acute cord compression, particularly in patients with known hematological disorders or who are undergoing anticoagulant therapy.
Vitamin-K Anticoagulants (VKA), most commonly warfarin, indirectly inhibit the synthesis of coagulation factors. The known limitations of VKAs have led to the development of NonVitamin K Oral Anticoagulants (NOAC) which directly inhibit specific coagulation factors. Several landmark phase III clinical trials have demonstrated the superiority of NOACs compared with VKAs have resulted in their progressively increased utilization in recent years [2]. To our best knowledge, we are the first to report a case of spontaneous, non-traumatic SIEH secondary to rivaroxaban in our local context.
While there are previous case reports on spontaneous SIEH secondary to VKAs use (warfarin) [3,4], recently there are emerging reports of SIEH secondary to the NOAC rivaroxaban alone [5,6].
Case report
A 72-year-old gentleman with a history of hypertension and atrial fibrillation on rivaroxaban (CHA2DS-VASc2), presented to the Emergency Department (ED) with sudden onset lower limb weakness, associated with bilateral lower limb numbness and lower back pain. There was no history of trauma. His vital signs were stable upon ED admission. Of note, the Activated Partial Thromboplastin Time (APTT) and Prothrombin Time (PT) were all within normal limits and the International Normalized Ratio (INR) was 1.17.
Clinical examination revealed upper limbs with power 5/5, lower limbs power 0/5 in all myotomes bilaterally. Lower limb reflexes were absent. The anal tone was present with no voluntary contraction. There was decreased sensation from T7 level downwards to both light touch and temperature.
Given the history of atrial fibrillation and concurrent anticoagulation use, with the presentation of sudden onset of low back pain together with acute lower limb weakness & numbness, our first impression was that patient most likely has a spontaneous epidural hematoma with acute cord compression. Urgent hematologist consultation was sought. 4-factor Prothrombin Complex Concentrate (PCC) at a dose of 50 units/kg of body weight (patient’s body weight was 90kg) was given.
Given the history of atrial fibrillation and concurrent anticoagulation use, with the presentation of sudden onset of low back pain together with acute lower limb weakness & numbness, our first impression was that patient most likely has a spontaneous epidural hematoma with acute cord compression. Urgent hematologist consultation was sought. 4-factor Prothrombin Complex Concentrate (PCC) at a dose of 50 units/kg of body weight (patient’s body weight was 90kg) was given.
The patient underwent T4 to T10 laminectomy and evacuation of SIEH for urgent spinal cord decompression. Dura was noted to be tense and full after laminectomies were performed. Bluish discoloration of the inferior portion of exposed dura was also noted. Durotomy was performed from T9-T10 levels. Dorsally located subdural hematoma was evacuated partially, as the hematoma was adherent to the spinal cord, samples of the evacuated hematoma was also sent for histological examination. Decision was made not to open dura from T4 to T8 as on MRI imaging, as the hematoma was ventral to the spinal cord with minimal mass effect. Durotomy was repaired primarily with Prolene 5/0 and overlaid with dural sealant. Subfascial surgical drain was placed. The surgical wound was closed in all layers.
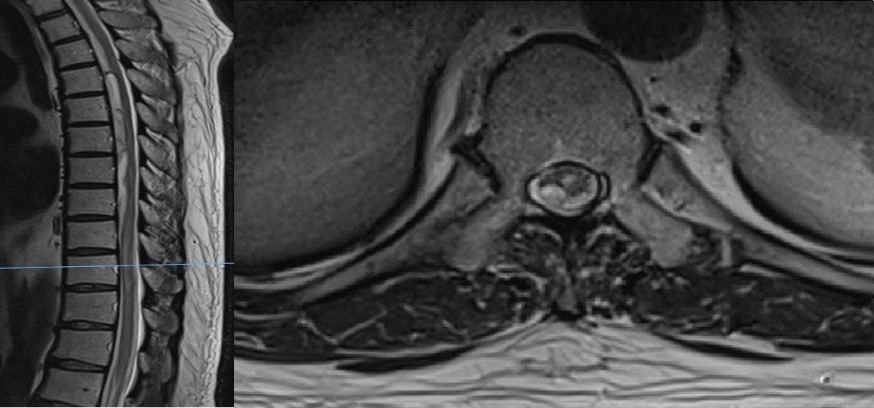
Formal histology of the partially evacuated hematoma confirmed blood clot and acute inflammatory cells with no other unexpected findings. Patient subsequently regained full power and sensation of the left lower limb by the first Post-Operative Day (POD), and MRC grade 2 power and 1+ sensation of right lower limb by POD 3. Patient underwent further rehabilitation.
Patient was last reviewed 16 months post-operation. The right lower limb power had recovered to MRC grade 3+ with residual bilateral lower limb numbness. As reported he was able to ambulate independently and there was no urinary or bowel incontinence. The surgical wound has healed well.
Follow up contrast enhanced spinal imaging confirmed spinal cord decompression with residual myelomalacia of the thoracic spinal cord at T9-10 level, with no evidence of intraspinal or intramedullary enhnacing lesion or mass (Figure 3).
Discussion
SIEH accounts for 4.1% of all intraspinal hematomas [7], and is a rare emergency condition when it results in acute spinal cord compression. SIEH are usually caused by iatrogenic medical procedures for example, spinal anaesthesia or lumbar punctures. Other etiologies include vascular lesions, for example, spinal arteriovenous fistulas or malformations, cavernomas, aneurysms (rare) or secondary to underlying hemorrhagic neoplasm, infection or coagulopathy. Bleeding diatheses such as thrombocytopenia, leukemia, hemophilia and antiplatelet or anticoagulant use may precipitate a SIEH [1]. Physicians should consider SIEH as one of the top differentials in anticoagulated patients presenting with spontaneous acute onset of back or radicular pain followed by paraplegia, with bowel and bladder dysfunction.
(i) Relevant anatomy
SIEHs are often located in the thoracic and thoracolumbar region [1], as in our reported case. The spinal subdural space contains no bridging veins in the subdural space in contrast to the intracranial anatomy. The spinal arachnoid mater is a connective tissue membrane without vessels which is closely attached to the dura mater. The pia mater forms a continuous layer on the surface of the cord to coat blood vessels within the subarachnoid space in a manner similar to that described in the leptomeninges over the human cerebral cortex [8]. The venous drainage system of the spinal cord is formed by a pial network connecting the intrinsic venous perforators and longitudinal venous collectors. Radicular veins follow the nerve roots, piercing the dura in approximately 60% of cases [9]. The vessels responsible for the hemorrhage in cases of SIEH has remained unknown, with rupture of the subarachnoid vessels with secondary dissection through the arachnoid membrane and into the subdural space being a possible explanation [1].
(ii) VKA and NOACs
There are known limitations to VKA as these drugs are influenced by various pharmacogenetic parameters, as well as interactions with other mediations and inconsistent efficacy with specific dietary requirements. Given the narrow therapeutic window, the need for frequent monitoring and dose titration, and variable patient response to VKA, novel Non-Vitamin KDependent Oral Anticoagulants (NOACs) have been developed. Commonly used NOACs approved for clinical use include dabigatran, rivaroxaban, apixaban, edoxaban, and betrixaban [4].
In contrast to VKAs which indirectly inhibit the synthesis of coagulation factors, NOACs directly inhibit specific coagulation factors. Dabigatran inhibits thrombin (factor IIa), whereas apixaban, betrixaban, edoxaban, and rivaroxaban inhibit activated factor Xa. The pharmacokinetics and pharmacodynamics of these agents are more predictable than VKAs, as well as wider therapeutic windows, allowing for fixed oral dosing without the need for monitoring. NOACs have demonstrated superiority to VKAs in certain clinical scenarios, for instance, as stroke prevention in patients with atrial fibrillation [10], and the treatment and prevention of venous thromboembolism [4,11].
There is no correlation between PT or APTT and the pharmacodynamics of the NOACs. In the management of SIEH, hematologists’ consultation is highly recommended for reversible options for NOACs as well as the confirmation of reversed coagulopathy prior to surgical intervention.
Conclusion
We present a rare case of spontaneous, non-traumatic, coagulopathy-related SIEH due to rivaroxaban use, resulting in acute spinal cord compression. As NOACs have several advantages compared to traditional VKAs, there is an increased presecription of NOACs for various indications, and as a result, there are increasing reports of hemorrhagic complications related to these new anti-coagulants. Cases of rivaroxaban related spontaneous SIEH have been reported previously, and to our best knowledge, this is the first reported case of rivaroxaban coagulopathy-related spontaneous SIEH with acute cord compression at our local context.
Physicians should consider SIEH as one of the top differentials in anticoagulated patients presenting with spontaneous acute onset of back or radicular pain followed by paraplegia, with bowel and bladder dysfunction. Discussion with hematologists for reversible options for NOAC associated coagulopathy is highly recommended. MRI imaging of the spine will confirm the condition and the level(s) of involvement. Urgent surgical spinal cord decompression with careful clot evacuation should proceed once reversal of coagulopathy has established.
References
- Hausmann O, Kirsch E, Radu E, et al. Coagulopathy induced spinal intradural extramedullary hematoma: Report of three cases and review of the literature. Acta Neurochir (Wien). 2001; 143: 135–140.
- Bruce Brand RA, Colleran GC, Broderick JM, Lui DF, Smith EM, Kavanagh EC, et al. Acute nontraumatic spinal intradural hematoma in a patient on warfarin. J Emerg Med. 2013; 45: 695–697.
- Girithari G, Dos Santos IC, Alves T, Claro E, Kirzner M, Massano AL. Spontaneous Spinal Intradural Hematoma in an Anticoagulated Woman. Eur J Case Rep Intern Med. 2018; 24; 5: 000951.
- Aronis KN, Hylek EM. Evidence Gaps in the Era of Non-Vitamin K Oral Anticoagulants. J Am Heart Assoc. 2018; 26; 7: e007338.
- Castillo JM, Afanador HF, Manjarrez E, Morales XA. Non-Traumatic Spontaneous Spinal Subdural Hematoma in a Patient with Non-Valvular Atrial Fibrillation During Treatment with Rivaroxaban. Am J Case Rep. 2015; 19; 16: 377-381.
- Gowda S, O’Hagan P, & Griffiths J. Cauda equina syndrome due to Factor Xa inhibitor (Rivaroxaban): Case report and review of literature. Case Reports in Clinical Pathology. 2020; 7: 7.
- Kreppel D, Antoniadis G, Seeling W. Spinal hematoma: a literature survey with meta-analysis of 613 patients. Neurosurg Rev. 2003; 26: 1–49.
- Nicholas DS, Weller RO. The fine anatomy of human spinal meninges. J Neurosurg. 1988; 69: 276-282.
- Rodesch G, Berenstein A, Lasjaunias P. Vasculature and vascular lesions. In: Manelfe C (ed) Imaging of the spinal cord. Raven Press, New York. 1992; pp 565-598.
- Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, et al. Committees A and Investigators. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011; 365: 981–992.
- Agnelli G, Buller HR, Cohen A, Curto M, Gallus AS, et al. AMPLIFY Investigators. Oral apixaban for the treatment of acute venous thromboembolism. N Engl J Med. 2013; 369: 799–808.