Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
Priapism in a patient with COVID-19: A case report
Agulleiro Juan Cruz*; Lapenna Leandro; Koren Claudio; Labrador Jorge; Coronado Paul; Villalba Bachur Roberto
Complejo Hospital Churruca, Visca Urology Service, Argentina.
*Corresponding Author: Juan Cruz Agulleiro
Complejo Hospital Churruca, Visca Urology Service,
Argentina.
Email: juancruzagulleiro@hotmail.com
Received : Oct 30, 2021
Accepted : Dec 21, 2021
Published : Dec 28, 2021
Archived : www.jcimcr.org
Copyright : © Cruz AJ (2021).
Abstract
A pro-inflammatory response in patients with coronavirus disease provokes hypercoagulability and hyperviscosity, following an excessive liberation of acute phase reactants. Thromboembolic complications such as Deep Venous Thrombosis, Pulmonary Embolism, Stroke and Acute Coronary Syndrome were described from the beginning of the pandemic as possible manifestations of this new virus. Priapism is a medical urgency that demands quick assessment and timely treatment.
A case of priapism is presented in a patient undergoing hospitalization for COVID-19. He was treated with cavernosal blood aspiration, irrigated with 0.90% w/v saline solution and intracavernosal injection of the sympathomimetic agent (adrenaline), with favorable response.
Keywords: priapism; COVID-19; thrombosis.
Citation: Haghighat S, Karimi A. Hypercalcemia and multiple osteolytic bone lesions: A rare presentation of acute lymphoblastic leukemia. J Clin Images Med Case Rep. 2021; 2(6): 1467.
Introduction
Since 2019, the world has been under a global health crisis because of COVID-19, affecting over 160 million people to date [1]. As we already know, the respiratory system is the most compromised. Nonetheless, manifestations at gastrointestinal, neurological, dermatological, and cardiovascular levels have also been reported.
Around 5% of the patients require Intensive Care Unit management, mainly due to Acute Respiratory Distress Syndrome [2].
Within this group of patients, 31% suffer thromboembolic complications [3], with potentially fatal consequences such as: Deep Venous Thrombosis, Pulmonary Thromboembolism, Stroke and Acute Coronary Syndromes.
This case report presents a patient on his second day after admission because of COVID-19 infection, with priapism as a urogenital pathology. This finding aims at adding diagnostic and therapeutic evidence to the few cases already reported [4-6].
Case report
A 62-year-old man with history of Arterial Hypertension, Mellitus Diabetes type 2, Grade 2 Obesity, and no urological history was admitted to the emergency room with febrile syndrome, headache, non-productive cough, anosmia, dysgeusia, myalgia, and generalized arthralgia. He had developed an unfavorable response, including respiratory failure. Supplemental oxygen was supplied at 10 L/min with a reservoir mask, and Intensive Care Unit management was required. COVID-19 diagnosis was confirmed by real-time reverse transcriptase-polymerase chain reaction on a nasopharyngeal swab specimen.
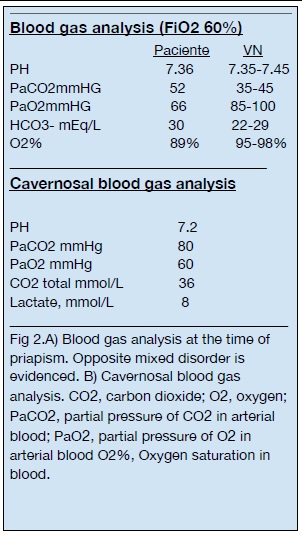
He then experienced hemodynamic failure, with supplemental O2 at 15 L/min, unstable respiratory mechanics, tachypnea and respiratory failure; therefore, orotracheal intubation and mechanical respiratory assistance were established. (FIO2 60% and PaO2 /FiO2 ratio of 85) (Figure 2).
Chest-Computed Tomography (CT) and CT angiography were performed at the initial admission and showed diffuse and bilateral involvement of the pulmonary parenchyma, with some areas indicating ground-glass opacity. No signs of proximal pulmonary embolism were identified.
After 24 hours of admission into the ICU, the patient presented a 5-hour episode of priapism.
A consequent increase in D-dimer was observed, among other acute phase reactants, which expressed its maximum value on the fourth day with a level of 4885, requiring anticoagulation, enoxaparin twice daily (BID) at a dose of 40 mg [7]. The patient was sedated and unable to answer questions on his medical record and pain levels. He had no previous history of priapism, he was not receiving any treatment for erectile sexual dysfunction, there was no trauma associated, and no medication nor current disease could be identified as an etiologic agent of priapism [8].
Physical examination revealed in duration of the corpora cavernosa with a flaccid glans. Given the persistence of the erection, the lack of response to local ice, and the inability to perform exercises to reduce priapism, it was decided to continue with the stepped care.
Two Abbocath 18 catheters, one in each corpora cavernosa, were placed at 3 and 9 o’ clock and dark blood with clots appeared.
Thus, 4 ml of this dark blood were drawn and cavernosal blood gases analysis showed a venous sample with a pattern of metabolic acidosis (Figure 2). This finding served for a clinical diagnostic suspicion of Ischemic, Low flow or Veno-Occlusive priapism.
The patient was irrigated two times with 0.90% w/v saline solution at 20-minute intervals, with no satisfactory response.
The next therapeutic step was an injection in each corpora cavernosa with 1 ml of adrenaline (dilution of 1/100 ml w/v saline solution) at 20-minute intervals, with no satisfactory response.
The therapeutic process was repeated. After 20 minutes, a decrease in the erection was confirmed. A compressive bandage and local ice were placed to avoid bruising.
The patient did not repeat episodes of priapism in the following days.
Discussion
Priapism is defined as a partial or complete erection, with or without sexual stimulation, that persists for more than 4 hours, which can be painful.
According to its pathophysiology, it can be classified into 3 types: • Ischemic, low-flow or veno-occlusive • Non-ischemic, high-flow, or arterial. • "Stuttering", recurring or intermittent.
In this case, we will focus on Ischemic priapism.
Ischemic priapism presents as rigidity of the corpora cavernosa associated with a flaccid state of the glans penis. It represents >95% of the cases.
It is a urological emergency that requires quick assessment and timely treatment. If the erection persists over time, the smooth muscle cells suffer necrosis, producing fibrosis of the corpora cavernosa, leading the patient to permanent erectile sexual dysfunction.
The most relevant data from the clinical history of a patient with priapism include: Duration of erection, presence and severity of pain, previous episodes of priapism and treatment provided, whether the patient is undergoing any treatment for erectile sexual dysfunction, medication or related drugs, hematological diseases (sickle cell disease, aplastic anemia, agranulocytosis, thrombocytopenia, paraneoplastic syndromes, among others).
Focusing on the physiopathology of this condition, we find different metabolic alterations depending on the time of evolution. The smooth muscle cells of the corpora cavernosa experience hypoxia, hypercapnia, glycopenia and metabolic acidosis [9,10].
A histological analysis with serial biopsies of the muscle cells of the corpora cavernosa during an episode of priapism shows predominantly interstitial edema at 12 o'clock. After 24 hours, destruction of the sinusoidal endothelium is mainly observed, exposing the basement membrane and revealing adhesion of platelets. After 48 hours, irreversible changes appear in the cells of the corpora cavernosa with necrosis and scar tissue [11].
In the case of the patient presented, the erection was maintained for over 5 hours, the presence of pain could not be verified (because of the patient’s condition) and there was no etiological factor for priapism in the clinical history.
The type of erection, already described above, the color of the blood and the arterial gas blood test results strongly bring us closer to the clinical suspicion of ischemic priapism.
The only finding that could be considered discordant was the presence of a partial pressure of O2 > 30 mmHg in the gases of the corpora cavernosa. There could be a correlation between this finding and the fact that the patient was intubated with 60% FIO2 at the time.
It is already known that COVID-19 causes a pro-inflammatory state in patients, which also favors a pro-thrombotic state; and this is evidenced by the presence of hyperviscosity, hypercoagulability, favored by leukocytosis and endothelial dysfunction generated mainly by the release of interleukins and nitric oxide. This leads to a prothrombotic state, plus endothelial dysfunction. Some of these factors may trigger priapism.
Conclusion
The existence of the pandemic pushes health care workers of all specialties to the limit, since it demands maximal physical and mental effort.
The multidisciplinary approach to this medical emergency allows us to carry out a fast and effective treatment, which, if not established in a timely manner, may lead to permanent sequelae.
Limitations
Due to the limited number of published cases, evidence to confirm that COVID-19 virus is an etiological agent of priapism is not conclusive.
Acknowledgments : Urology Service from the Medical Complex of the federal police Churruca-Visca Hospital. Intensive Care Unit service from the Medical Complex of the federal police Churruca-Visca Hospital.
References
- Johns Hopkins University (Baltimore, USA), local authorities Last update of figures. GMT. 2021; 8: 39.
- Liang W., Liang H., Ou L. Development and Validation of a clinical risk score to predict the occurrence of critical illness in hospitalized patients with COVID-19. JAMA intern Med. 2020; Pub ahead of print.
- Klok F.A., Kruip M., van der Meer N.J.M. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020.
- Lamamri M, Chebbi A, Mamane J, Abbad S, Munuzzolini M, Sarfati F, et al. Priapism in a patient with coronavirus disease 2019 (COVID-19): A case report. Am J Emerg Med. 2020; 39: P251.
- Abdulmalik Addar, Omar Al Fraidi, Ahmed Nazer, Naif Althonayan, Yahya Ghazwani, Priapism for 10 days in a patient with SARSCoV-2 pneumonia: A case report, Journal of Surgical Case Reports. 2021; Volume 2021, Issue 4, rjab020.
- Silverman, Matthew L et al. “Priapism in COVID-19: A thromboembolic complication.” The American journal of emergency medicine, S0735-6757(20)31191-8. 2021;
- COVID-19 and VTE-Anticoagulation - Hematology.org. 2020. https:// www.hematology.org/covid-19/covid-19-and- vte-anticoagulation Accessed August 20, 2020.
- EUA guidelines on Sexual and Reproductive Health, Page 108, Table 32.
- El-Bahnasawy, M.S., et al. Low-flow priapism: Risk factors for erectile dysfunction. BJU Int. 2002.
- Muneer A et al. Investigation of cavernosal smooth muscle dysfunction in low flow priapism using an in vitro model. Int J Impot Res. 2017.
- Vreugdenhil S., et al. Ischemic priapism as a model of exhausted metabolism. Physiol Rep. 2019.