Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
Löfgren’s syndrome - An uncommon presentation of a common disease
Kieran VJ Mullins1*; Gideon Mlawa2
1 Registrar in Acute Internal Medicine, Department of Acute Internal Medicine, Queen’s Hospital, Rom Valley Way, Romford, London, RM7 0AG, UK.
2 Consultant Endocrinologist, Diabetelogist and General Physician, Department of Acute Internal Medicine, Queen’s Hospital, Rom Valley Way, Romford, London, UK, RM7 0AG.
*Corresponding Author: Kieran VJ Mullins
Registrar in Acute Internal Medicine, Department
of Acute Internal Medicine, Queen’s Hospital, Rom
Valley Way, Romford, London, UK, RM7 0AG.
Email: kieran.mullins@nhs.net
Received : Oct 18, 2021
Accepted : Dec 22, 2021
Published : Dec 29, 2021
Archived : www.jcimcr.org
Copyright : © Mullins KVJ (2021).
Abstract
A 24 year old woman presented to our institution with a two week history of multiple discrete, painful, nodular and indurated foci of erythema on her lower limbs against a six week background history of a constellation of more nonspecific symptoms including intermittent dry cough, malaise, migrating arthralgias, subjective fevers, anorexia and weight loss. She denied B symptoms. There were no ophthalmic, neurological or cardiovascular symptoms. Examination was significant for features of mild hyper-metabolism manifest by low grade pyrexia with accompanying diaphoresis in conjunction with bilateral lower limb predominant erythema nodosum. Laboratory studies revealed a neutrophilic leucocytosis, raised acute phase reactants/ inflammatory markers, normal serum calcium, ACE, Vitamin D, renal and liver indices. Chest radiography revealed bilateral hilar adenopathy with minimal interstitial involvement. A diagnosis of Löfgren’s syndrome was suspected, an uncommon variant of multisystem sarcoidosis. Subsequent bronchoscopy with trans-bronchial tissue biopsy revealed non-caseating granulomas. The diagnosis was confirmed and treatment instituted with non-steroidal anti-inflammatory medication.
Citation: Mullins KVJ, Mlawa G. An uncommon presentation of a common disease. J Clin Images Med Case Rep. 2021; 2(6): 1526.
Background
Sarcoidosis is common at northern latitudes particularly amongst Irish and Scandinavian populations. Despite a potential for multisystem involvement and thus heterogeneity of presentation respiratory symptoms typically predominate accounting for first contact with health providers in the majority of cases. This was an atypical presentation in that the patient’s principal complaints were an indurated rash and constitutional upset with paucity of respiratory features. Caucasian and African patients presenting with erythema nodosum with or without associated systemic upset should alert the attending physician to the possibility of Lofgren’s syndrome and a new diagnosis of sarcoidosis.
Case presentation
A 24 year old woman presented to our institution in June 2017 with a multi-focal, evolving and painful bilateral lower limb rash in association with subjective fevers and malaise. The rash had been present for two weeks, initially involving only the distal lower limbs but over the past week new lesions had developed on the patient’s thighs and upper limbs. The patient was malaised, anorexic and sweaty, had subjective fevers, flitting arthralgias and occasional dry cough over the course of the preceding six weeks. She had been well prior to the current illness. A consultation with a general practitioner four days before presentation to hospital led to prescription of a beta-lactam antibiotic for a presumptive diagnosis of cellulitis. There was minimal improvement in her constitutional symptoms and the rash persisted. Clinical examination was significant for multiple upper and lower limb foci of injurated erythema consistent with erythema nodosum. The patient was flushed in appearance and there was associated mild generalised diaphoresis. There were no neurological, cardiovascular or ophthalmic symptoms or signs.
The patient’s past medical history included anxiety and depression for which she took 20 mg citalopram orally once daily (no recent dose adjustments), childhood asthma, a raised BMI and remote appendicectomy as a teenager. She had no known drug allergies. She had received the full vaccination schedule as a child with appropriate boosters when indicated. She had never had a blood transfusion or blood products. She had multiple upper and lower limb tattoos though had had no new tattoos in the preceding year. The patient denied current or previous intravenous drug use. There were no sick contacts. She was not pregnant and did not use hormonal contraception. She had long standing oligomennorrhoea which was not under investigation. Her cervical smear history was up to date.
The patient was of Polish origin though had lived the majority of her life in London. She was not in paid employment. She was a smoker of between ten and twenty roll up cigarettes since her early teens and drank only moderate amounts of alcohol. The patient was in a committed same sex relationship for the past five years with no other sexual partners. She denied prior STIs. She had returned from a holiday in Poland with her partner two months previously during which they had engaged in mountain hiking through bush. She reported no tick bites or rashes around the time of the holiday. They had not engaged in any fresh water activities or come into contact with domestic or farm animals. They had eaten only at their accommodation.
There was no family history of inflammatory conditions including inflammatory bowel disease or rheumatoid arthritis.
Clinical examination revealed a healthy appearing young woman with a raised BMI. She had multiple tattoos predominantly on the lower limbs. She was not in respiratory distress.
The patient had a low grade pyrexia of 37.8 degrees Celsius. Closer inspection revealed subtle signs suggestive of hypermetabolism including mild diaphoresis and a slightly flushed facial appearance. The patient had multiple, discrete, erythematous, nodular and indurated lesions on the lower limbs up to the groin. There were a few burgeoning similarly discrete lesions on the upper limbs. Examination of the eyes revealed normal visual fields, extra-ocular motility and no signs of uveitis. She had normal cranial nerves bilaterally. Examination of the chest and cardiovascular system was unremarkable as was the abdominal examination.
Investigations
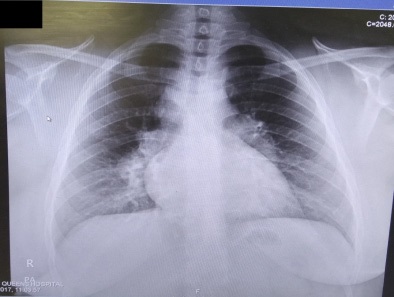
The patient’s antibiotics were stopped and treatment with antipyretics and anti-inflammatory medication instituted. A urinalysis including beta-hCG was normal. Electrocardiogram revealed normal sinus rhythm with no bundle blocks or axis deviation. A plain radiograph of the chest revealed bulky bilateral hilae consistent with bilateral hilar adenopathy. There were no parenchymal infiltrates visible. Laboratory studies revealed a mild and non-specific neutrophil predominant leucocytosis, a normal serum vitamin D, normal calcium and serum ACE. Renal and hepatic indices as well as a coagulation profile were all within normal limits. The patient was discharged. She proceeded to high resolution CT scan of the chest and bronchoscopy with transbronchial biopsy of an intra-thoracic node. The resulting specimen analysed by the pathology department at our centre revealed a primary granulomatous process characterised by non-caseating granulosmas. A presumptive diagnosis of sarcoidosis was made.
Differential diagnosis
The differential diagnosis for erythema nodosum: 1. Granulomatous disease – non-caseating (e.g. sarcoidosis), caseating (e.g. TB, histoplasmosis, coccidioidomycosis) 2. Bacterial disease – Streptococcus, chlamydia, Yersinia, Mycoplasma 3. Viral infection – HIV, EBV, HSV, HBV & HCV 4. Drugs – Oral contraceptives, beta lactam antibiotics 5. Inflammatory disorders – UC and Crohn’s (less common with the latter)
Treatment
The patient did not meet criteria for initiation of corticosteroids; accepted indications include ocular involvement, stage II or greater on chest X-ray investigation, cardiac involvement, sarcoid related hypercalcaemia and neurosarcoidosis. The patient was treated with a non-steroidal anti-inflammatory (NSAID). She was referred to a tertiary referral centre where lung function tests revealed no significant airflow obstruction. She was commenced on inhaled corticosteroid therapy
Outcome and follow-up
At six weeks follow up in clinic the patient had subjective symptomatic improvement, normalising inflammatory markers and leucocyte count and continued on an oral non-steroidal anti-inflammatory agent with excellent effect. At one year follow up her sarcoidosis was in remission, repeat CT thorax revealing resolution of the mediastinal lymphadenopathy.
Discussion
Löfgren’s syndrome is an acute form of sarcoidosis. It was first described in 1953 by the Swedish physician Sven Halvar Löfgren. He observed the clinical triad of bilateral hilar lymphadenopathy, erythema nodosum and periarticular inflammation of the ankles often in conjunction with a fever [1]. A search of PubMed for publications with ‘Löfgren’ contained in the title yields thirty-six results only five of which document case reports of this syndrome from across the world [2-7]. Common amongst reported cases is an association with Caucasian ethnicity and those at northern lattitudes are known to be at increased risk [8]. Thus, Löfgren’s is an important clinical entity for the physician practising in the northern hemisphere and particularly in the region of northern Europe.
Sarcoidosis is a chronic inflammatory granulomatous disorder against an as yet unidentified antigen [9]. It represents a T-cell mediated or type IV hypersensitivity reaction according to the classic Gell and Coombs classification system.
Of the variously described sarcoid presentations Löfgren’s syndrome is an acute variant associated with a good prognosis and predicts a good response to conservative management [6]. Diagnosis is clinico-radiological but tissue biopsy may be necessary to exclude other granulomatous disease such as mycobacterium tuberculosis, malignancies such as lymphoproliferative disorders and other infectious aetiologies as guided by history and physical examination.
Glucocorticoid pharmacotherapy is commonly employed in the treatment of sarcoidosis. Importantly, it is well known that patients with Löfgren’s typically do not need treatment initiation with corticosteroids thus avoiding the broad spectrum of adverse events associated with such agents [10]. Unfortunately misdiagnosis is common and often patients will receive inappropriate treatment with antibiotics before the correct diagnosis is made [3]. With timely and careful evaluation these patients may be safely managed with reassurance regarding the nature of the condition, pharmacotherapy with non-steroidal anti-inflammatory agents and appropriate clinical follow up. It is therefore essential for the clinician to be aware of this clinical entity given the importance of correct patient counselling with respect to disease prognostication and treatment. Patients with Löfgren’s should expect disease remission within two months with conservative measures and may expect an overall excellent long term prognosis [7].
Learning points/take home messages
1. Sarcoidosis is common amongst Celtic Europeans and follows a chronic course 2. Suspect acute sarcoidosis/Lofgren’s syndrome in any patient presenting with a triad of erythema nodosum, arthralgias, bilateral hilar lymphadenopathy often in conjunction with fever 3. This presentation portends a good long term prognosis and obviates the need for glucocorticoids
References
- Kirresh O, J. Schofield, G. George. Acute sarcoidosis: Lofgren’s syndrome. Br J Hosp Med (Lond), 2015; 76: p. 154-158.
- Bourdillon L., et al., Lofgren syndrome and peritoneal involvement by sarcoidosis: Case report. Chest, 2007; 132: p. 310-312.
- Klevtsova E., et al., Lofgren Syndrome Misdiagnosed as LowerExtremity Cellulitis. J Clin Rheumatol, 2015; 21: p. 271-272.
- Misteli M., V. Festini. A case from practice (232). Stage I sarcoidosis with erythema nodosum and febrile arthropathy (Lofgren syndrome). Schweiz Rundsch Med Prax. 1991; 80: p. 1388-1389.
- Revol L. and J. Maitrepierre. Lofgren syndrome; two case reports of bilateral hilar adenopathies with polymorphic or nodose erythema of undetermined etiology and regressive evolution. Sem Hop. 1957; 33: p. 3959-3964.
- Stiefelhagen P., Arthralgia with erythema nodosum. Lofgren syndrome in acute pulmonary sarcoidosis with erythema nodosum. MMW Fortschr Med. 1999; 141: p. 53-54.
- Tejera Segura B., et al., Lofgren syndrome: A study of 80 cases. Med Clin (Barc) 2014; 143: p.166-169.
- Mana J, Considerations about Lofgren syndrome. Med Clin (Barc), 2014; 143: p. 163-165.
- Ponhold W. The Lofgren syndrome: Acute sarcoidosis. Rontgenblatter. 1977; 30: p. 325-327.
- Mannhart R., T.C. Medici, E. Tanner. Does steroid therapy have an effect on the course of Lofgren syndrome? Catamnestic studies on 25 patients with Lofgren syndrome at the Zurich county hospital. Schweiz Med Wochenschr. 1977; 107: p. 187-190.