Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
A neonate with acquired long QT from placental transfer of medications
Eyal Sagiv1*; Jieun Kwak2; Rachel L Chapman2; Allison C Hill2
1 Seattle Children’s Hospital and University of Washington School of Medicine, Seattle, Washington, USA.
2 Children’s Hospital Los Angeles, Department of Pediatrics, Keck School of Medicine, University of Southern California, Los Angeles, California, USA.
*Corresponding Author: Eyal Sagiv
Seattle Children’s Hospital and University of
Washington School of Medicine, Seattle, Washington,
USA.
Email: Eyal.Sagiv@seattlechildrens.org
Received : Nov 11, 2021
Accepted : Jan 03, 2022
Published : Jan 10, 2022
Archived : www.jcimcr.org
Copyright : © Sagiv E (2022).
Abstract
Long QT Syndrome (LQTS) can present in the neonate with bradycardia and AV block and confers significant risk for life threatening ventricular arrhythmias. We report a case of a neonate presenting with complex bradyarrhythmias secondary to acquired LQTS after maternal overdose of QT-prolonging medications (haloperidol and sertraline). When the mother was brought in to the delivery center unconscious, fetal bradycardia was noted and the baby was emergently delivered prematurely. The newborn’s initial ECG showed bradycardia with AV node conduction block, rate related His-Purkinje conduction aberration with varying QRS morphology and a QTc >600 ms. She continued to be bradycardic through her first day of life with echocardiogram showing mild cardiac dysfunction. With the elimination of the offending medication from her circulation, the infant’s rate and function abnormalities resolved and QTc normalized. Both haloperidol and sertraline are known to be strong suppressors of the HERG potassium channel that plays an important role in myocardial repolarization and both medications can cross the placenta. Maternal overdose can cause transient QT-prolonging effect similar to that of inherited LQTS type 2. Given the high risk for sudden death in affected newborns, reporting this case is aimed to raise the awareness of acquired LQTS by placental transfer of medication. Early identification of neonates at risk should prompt ECG testing. If long QT is identified, the newborn should be closely monitored with care to avoid any further QT prolonging medications or conditions, until the toxic medication effect resolves.
Citation: Sagiv E, Kwak J, Chapman RL, Hill AC. A neonate with acquired long QT from placental transfer of medications. J Clin Images Med Case Rep. 2022; 3(1): 1541.
Introduction
Long QT syndrome (LQTS) is characterized by a prolonged QT interval on ECG and increased risk of Torsades de Pointes (TdP) and sudden death. Two main etiologies of LQTS have been identified: (1)“congenital LQTS” is due to a mutation in specific ion channels, and (2)“acquired LQTS” is due to QT-prolonging medications or electrolyte abnormalities. Congenital LQTS can present early in the fetal or neonatal period with bradycardia and/oratrioventricular (AV) block [1-3] and confers a high risk for life-threatening ventricular arrhythmias [4,5]. In this setting, AV block can be due to “pseudo 2:1 block,” in which the AV node or His-Purkinje system is unable to conduct the next atrial impulse due to the prolonged refractory period [1,5]. Delayed His-Purkinje response, leading to conduction aberration, has also been described [3,6]. We report a case of maternal suicidal attempt by overdose of QT-prolonging medications that lead to fetal and neonatal complex bradyarrhythmiasas a result of acquired LQTS.
Case presentation
The female neonate was born prematurely at 33 weeks gestation to a 31-year-old mother with a known history of affective mood disorder, treated with haloperidol and sertraline throughout pregnancy. On the day of delivery, the mother was brought to the hospital unconscious after a suicide attempt. She had ingested approximately 250 mg of haloperidol (fifty 5 mg tabs) and possibly also sertraline and diphenhydramine pills at unknown doses. Maternal urine and later meconium toxicology were negative for other detectable drugs.
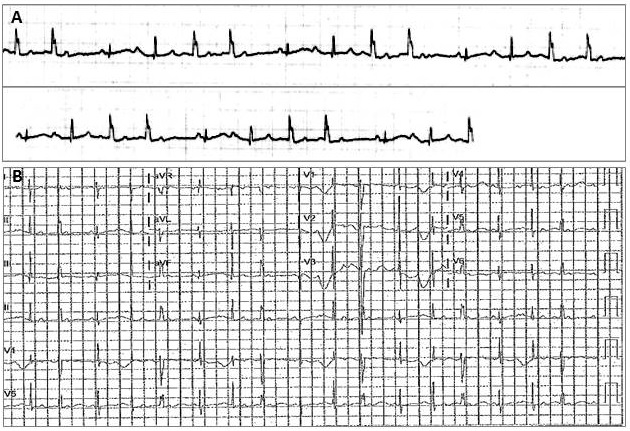
Due to bradycardia and poor reactivity on fetal monitoring, the baby was delivered via emergent cesarean section soon after admission. The infant weighed 2040 grams and had APGAR scores of 3 at 1 minute and 5 at 10 minutes requiring immediate positive pressure ventilation. She was noted to be bradycardic and was transferred to the Neonatal Intensive Care Unit (NICU) at the birth hospital. Telemetry monitoring showed an average heart rate of 100-120 bpm with episodic slowing and rate irregularity, as well as intermittent wide QRS complexes (Figure 1A). In the NICU, the patient was intubated and administered surfactant for Respiratory Distress Syndrome (RDS). She had hypoglycemia that resolved with intravenous fluid administration and remained hemodynamically stable. Still, as her bradyarrhythmias continued, she was transferred to our quaternary NICU at about 15 hours of life for cardiology consultation.
On initial evaluation, the baby was warm and well perfused with stable blood pressures. She had a quiet precordial activity, variable rhythm with slowing to 50-110 bpm and no clicks, rubs or murmurs on auscultation. Her initial ECGs were reviewed (Figure 1B), showing a regular atrial rate of 135 bpm with an irregular QRS rate, averaging about 90 bpm with Wenckebach conduction (Mobitz type-1 block at the level of the AV node) and rate-related wide QRS complex in a left bundle branch block (LBBB) pattern (suggesting additional conduction aberration at the His- Purkinje level, below the AV node). The corrected QT interval (QTc) was difficult to measure due to flattened T waves and rate irregularity but was estimated to be greater than 600 ms. The infant was monitored in the NICU and continued to have occasional episodes of Wenckebach conduction for a few hours. Repeat ECG in our center at 16 hours of life demonstrated normal sinus rhythm with a regular rate and a QTc of 454 ms. Echocardiogram showed mild left ventricular dilation and mild to moderate mitral valve regurgitation, normal ventricular function, no pericardial effusion and a patent ductus arteriosus. By day of life (DOL) 2 she had no further arrhythmias, repeat ECG on DOL 3 showed QTc of 452 ms and repeat echo on DOL 7 showed normal function with only trivial mitral regurgitation. Still requiring support for resolving RDS and feeding immaturity, she was transferred back to her local birth hospital for continued NICU care on DOL 9.
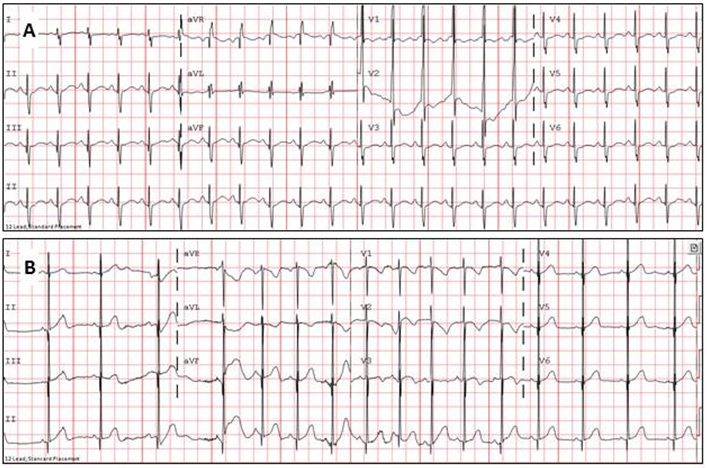
The infant was seen in cardiology clinic at 7 months of age to confirm the diagnosis of acquired (transient) versus congenital LQTS. She was growing and developing well and had not experienced any syncope, cyanosis or other cardiac symptoms. Her ECG at follow up showed sinus arrhythmia with an average rate of 99 bpm and a normal QTc of 396 ms with normal T wave morphology (Figure 2).
Discussion
There have been few reports of acquired LQTS in neonates [7-9] and even fewer by placental transfer of maternal medications [4,10,11]. This report describes the presentation of bradyarrhythmia related to acquired LQTS after maternal ingestion of QT-prolonging medications. We believe this topic is of importance due to the risk of life-threatening arrhythmias and implications for fetal and neonatal management.
Etiology
Our case demonstrates that QT-prolonging medications that cross the placenta can significantly affect the fetal myocardium. In our case, the mechanism of QT prolongation was most likely inhibition of the KCNH2 (or HERG) potassium channel by haloperidol, a similar mechanism to most QT-prolonging medications [9]. The high-potency KCNH2 channel blocking effect of haloperidol is well known and has prompted the US Food and Drug Administration to extend a warning regarding the increased risk for QT prolongation and TdP from administration of IV haloperidol [12,13]. In our case, the mother ingested 50 times the prescribed dose of oral haloperidol (5 mg per day; recommended adult dose is up to 30-100 mg in chronic users). There has been one other report of maternal overdose of haloperidol: Hansen et al. [14] reported a case of a woman at 34 weeks gestation, who collapsed after ingesting 300 mg of haloperidol. In that case, the initial biophysical profile score was 2/10 with a fetal heart rate of 150 bpm that was nonreactive with decreased variability; it corrected only 5 days after the ingestion. In our case, the baby was delivered prematurely and post-natally diagnosed with AV block and aberrant ventricular conduction.
While maternal haloperidol is the most likely cause of the infant’s dysrhythmia, other medications may have contributed. Sertraline can also block the HERG channel and cause acquired LQTS [15,16]. Serotonin reuptake inhibitors like sertraline are lipophilic which leads to high placental permeability [17]. Still, fetal-maternal concentrations and clinical symptoms vary substantially, suggesting variable metabolism [18]. Placental transfer of diphenhydramine has been reported in animal models, but its effects on the fetus are unclear. [19]
Correlating the molecular mechanism to that of genetically inherited LQTS, haloperidol delays repolarization by affecting the same potassium channel that is abnormal in congenital LQTS type 2 (KCNH2 mutation) [20]. This inherited LQTS is more likely to present with conduction-related bradyarrhythmias (as with our patient) and confers a higher risk for TdP compared to the more common LQTS type 1 (that tends to present with sinus bradycardia) [1]. Much research has been done to evaluate the role of neonatal LQTS in sudden infant death syndrome. Recent literature suggests that infantile LQTS is implicated in approximately 10% of cases of the cases [21]. LQTS may also have a significant role in intrauterine fetal demise as Crottiet al [22] showed that pathogenic variants and variants of uncertain significance in common LQTS genes were found in 3.3% and 8.8% of 91 cases of unexplained intrauterine fetal demise, respectively. It is unknown, however, whether acquired LQTS due placental transfer of medications also plays a role in intrauterine fetal demise.
Diagnosis
Given the risk of life-threatening ventricular arrhythmias with neonatal LQTS, accurate and timely diagnosis is of great importance [23]. Bradyarrhythmias in particular can appear in the perinatal period and have been used to predict LQTS (congenital or acquired) [2]. Thus, bradycardia (particularly with 2:1 block) on routine fetal heart rate monitoring should prompt a referral to a pediatric cardiologist for a fetal echocardiogram, during which the rhythm can be roughly assessed [3,25]. Fetal echocardiography allows for evaluation of the atrial to ventricular ratio, but does not allow for assessment of the conduction system. Fetal magnetocardiography is a newer technology that can allow for assessment of the conduction system and offers a modality to monitor the heart rhythm and QTc in cases of particular concern [26,27].
A neonate with relative bradycardia should have an ECG performed as this can be a presenting sign of LQTS. Unexplained syncope and seizures may correlate with episodic TdP and should also be evaluated with an ECG. As QTc changes are dynamic and often prolonged by hypokalemia, hypocalcemia, hypomagnesemia, acidosis, increased intracranial pressure, endocrinologic conditions and medications, telemetry remains an important tool in detection of arrhythmias.
Management
Anticipation of either congenital or acquired LQTS in utero can alter perinatal management. During the pregnancy, cases of fetal LQTS may be managed with close monitoring by specialists, discontinuation of any maternal QT-prolonging medications with placental transmission and consideration of beta- blockade or sodium channel blockade (mexilitine) to shorten repolarization and prevent tachy- and bradyarrhythmias [7,28,29]. A post-natal management plan should also be made to prepare for possible arrhythmias if fetal LQTS is suspected [30]. Neonates with a QTc interval greater than 500 ms are at a particularly increased risk of cardiac events. They should have prompt postnatal evaluation with an ECG and cardiology consultation, and if needed, transfer to a higher level of care. For suspected cases of acquired LQTS, thorough evaluation should be performed including pre- and post-natal medication review, with efforts to discontinue QT-prolonging medications as possible (https://crediblemeds.org/). Correctable etiologies (i.e. electrolyte abnormalities) should be treated accordingly with continued close monitoring.
Conclusion
We describe a case of a neonate with acquired LQTS as a result of maternal ingestion of QT-prolonging medication(s). Postnatally, the infant manifested acquired LQTS with AV block and conduction aberration, which indicated a risk for lifethreatening ventricular tachycardia. This is the first described case of complex bradyarrhythmias due to acquired LQTS secondary to maternal medication overdose. In this case, the bradyarrhythmia resolved once the offending medications were eliminated from the circulation. However, the clinical severity demonstrates the need for further investigation into QTprolonging medications and potential maternal-fetal influences.
References
- Lupoglazoff JM. et al. Long QT syndrome in neonates: Conduction disorders associated with HERG mutations and sinus bradycardia with KCNQ1 mutations. J. Am. Coll. Cardiol. 2004; 43: 826–830.
- Donofrio MT, Gullquist SD, O Connell NG, Redwine FO. Fetal presentation of congenital long QT syndrome. Pediatr Cardiol. 1999; 20: 441–444.
- Gorgels AP, Al Fadley F, Zaman L, Kantoch MJ, Al Halees Z. The long QT syndrome with impaired atrioventricular conduction: A malignant variant in infants. J. Cardiovasc. Electrophysiol. 1998; 9: 1225–1232.
- Fukushima N, Nanao K, Fukushima H, Namera A, Miura M. A neonatal prolonged QT syndrome due to maternal use of oral tricyclic antidepressants. Eur. J. Pediatr. 2016; 175: 1129–1132.
- Scott WA, Dick M. Two: One atrioventricular block in infants with congenital long QT syndrome. Am. J. Cardiol. 1987; 60: 1409–1410.
- Van Hare GF, Franz MR, Rogé C, Scheinman MM. Persistent functional atrioventricular block in two patients with prolonged QT intervals: Elucidation of the mechanism of block. Pacing Clin. Electrophysiol. PACE. 1990; 13: 608–618.
- Blais BA, Satou G, Sklansky MS, Madnawat H, Moore JP. The diagnosis and management of long QT syndrome based on fetal echocardiography. Hear Case Rep. 2017; 3: 407–410.
- Miura M, Yamagishi H, Morikawa Y, Matsuoka R. Congenital long QT syndrome and 2:1 atrioventricular block with a mutation of the SCN5A gene. Pediatr. Cardiol. 2003; 24: 70–72.
- Fobe C, Van Grambezen B, Moniotte S, Vo C, Dussart A, Danhaive O, Piersigilli F. Torsade de pointe due to QT prolongation following erythromycin administration in a preterm infant. Acta Cardiol. 2021; 23: 1-5.
- Parikh R, Hussain T, Holder G, Bhoyar A, Ewer AK. Maternal methadone therapy increases QTc interval in newborn infants. Arch. Dis. Child. Fetal Neonatal Ed. 2011; 96: F141-143.
- Krasemann T. QT prolongation in the newborn and maternal alcoholism. Cardiol. Young. 2004; 14: 565–566.
- Berul C. Acquired long QT syndrome: Definitions, causes, and pathophysiology - Up To Date. Available at: https:// www.uptodate.com/contents/acquired-long-qt-syndromedefinitions-causes-and-pathophysiology?search=acquired%20 long%20qt&source=search_result&selectedTitle=1~72&usage_ type=default&display_rank=1. (Accessed: 25th April 2018)
- Meyer Massetti C, Cheng CM, Sharpe BA, Meier CR, Guglielmo BJ. The FDA extended warning for intravenous haloperidol and torsades de pointes: How should institutions respond? J. Hosp. Med. 2010; 5: E8-16.
- Hansen LM, Megerian G, Donnenfeld AE. Haloperidol overdose during pregnancy. Obstet. Gynecol. 1997; 90: 659–661.
- Lee HA, Kim KS, Hyun SA, Park SG, Kim SJ. Wide spectrum of inhibitory effects of sertraline on cardiac ion channels. Korean J. Physiol. Pharmacol. Off. J. Korean Physiol. Soc. Korean Soc. Pharmacol. 2012; 16: 327–332.
- Klein Schwartz W, Anderson B. Analysis of sertraline-only overdoses. Am. J. Emerg. Med. 1996; 14: 456–458.
- Shea AK, Oberlander TF, Rurak D. Fetal serotonin reuptake inhibitor antidepressant exposure: Maternal and fetal factors. Can. J. Psychiatry Rev. Can. Psychiatr. 2012; 57: 523–529.
- Rampono J. et al. Placental transfer of SSRI and SNRI antidepressants and effects on the neonate. Pharmacopsychiatry. 2009; 42: 95–100.
- Yoo SD, Axelson JE, Taylor SM, Rurak DW. Placental transfer of diphenhydramine in chronically instrumented pregnant sheep. J. Pharm. Sci. 1986; 75: 685–687.
- Drolet B, Khalifa M, Daleau P, Hamelin BA, Turgeon J. Block of the rapid component of the delayed rectifier potassium current by the prokinetic agent cisapride underlies drug-related lengthening of the QT interval. Circulation. 1998; 97: 204–210.
- Saul JP, Schwartz PJ, Ackerman MJ, Triedman JK. Rationale and objectives for ECG screening in infancy. Heart Rhythm. 2014; 11: 2316–2321.
- Crotti L. et al. Long QT syndrome-associated mutations in intrauterine fetal death. JAMA. 2013; 309: 1473–1482.
- Sarquella Brugada G. et al. Early Identification of Prolonged QT Interval for Prevention of Sudden Infant Death. Front Pediatr. 2021; 9: 704580.
- Paech C, Suchowerskyj P, Gebauer RA. Successful treatment of a newborn with genetically confirmed long QT syndrome 3 and repetitive Torsades De Pointes tachycardia. Pediatr. Cardiol. 2011; 32: 1060–1061.
- Relan J, Gujral JS, Reddy SS, Parakh N, Singh S, Ramakrishnan S. Long QT syndrome with AV Wenckebaching & bundle branch block in a neonate. Indian Pacing Electrophysiol J. 2020; 20: 286- 289.
- Cuneo BF, et al. In utero diagnosis of long QT syndrome by magnetocardiography. Circulation. 2013; 128: 2183–2191.
- Menéndez T, et al. Prenatal diagnosis of QT prolongation by magnetocardiography. Pacing Clin. Electrophysiol. PACE. 2000; 23: 1305–1307.
- Cuneo BF, et al. Arrhythmia phenotype during fetal life suggests long-QT syndrome genotype: Risk stratification of perinatal long QT syndrome. Circ. Arrhythm. Electrophysiol. 2013; 6: 946–951.
- Cuneo BF, et al. Prenatal diagnosis and in utero treatment of torsades de pointes associated with congenital long QT syndrome. Am. J. Cardiol. 2003; 91: 1395–1398.
- Greene EA, Berul CI, Donofrio MT. Prenatal diagnosis of long QT syndrome: Implications for delivery room and neonatal management. Cardiol. Young. 2013; 23: 141–145.