Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
Brachial plexopathy due to subclavian artery pseudoaneurysm secondary to comminuted clavicle shaft fracture: A case report
Ahmed Mabrouk
Calderdale and Huddersfield NHS Trust, Huddersfield, HD3 3EA, UK.
*Corresponding Author: Ahmed Mabrouk
Calderdale and Huddersfield NHS Trust, Huddersfield, HD3 3EA, UK.
Email: ahmed.mabrouk3@yahoo.com
Received : Nov 13, 2021
Accepted : Jan 03, 2022
Published : Jan 10, 2022
Archived : www.jcimcr.org
Copyright : © Mabrouk A (2022).
Abstract
In adults, brachial plexopathy due to clavicle fractures is rare and is most commonly caused by nonunion, mal-united fragments, hypertrophic callus, or pseudoaneurysm of the subclavian artery or vein. Conservative treatment of nondisplaced and displaced clavicle shaft fractures in adults usually produces satisfactory outcomes.
This article presents a case of a 82-year-old man who sustained a closed, comminuted midshaft left clavicle fracture complicated by brachial plexus injury secondary to pseudoaneurysm of the left subclavian artery. Initially, the fracture was treated conservatively. However, he returned 5 days later with left brachial plexopathy.
Computed tomography angiogram confirmed left subclavian artery pseudoaneurysm secondary to the fracture. The patient had endovascular stenting of the left subclavian artery to exclude the aneurysm. 12 weeks later, he had malunited clavicle and no improvement in brachial plexus function. 16 weeks after the injury, he had left brachial plexus exploration, decompression and open reduction and internal fixation of his left clavicle mal-united fracture. 4 weeks post operative, patient started to develop signs suggestive of significant re-innervation.
Citation: Mabrouk A. Brachial plexopathy due to subclavian artery pseudoaneurysm secondary to comminuted clavicle shaft fracture: A case report. J Clin Images Med Case Rep. 2022; 3(1): 1543.
Introduction
Major neurovascular injury has been well documented with non operative management of clavicle fractures [1]. Direct injury to the vessels and brachial plexus can occur at the time of the fracture or present in a delayed manner secondary to pseudoaneurysms [1-5].
A pseudoaneurysm is an extravascular haematoma communicating freely with the intravascular space through a defect in the vessel wall [1,2]. Pseudaneurysm wall is the tissue compressed by the haematoma, contrary to the three layers arterial wall of a true aneurysm [1-3]. Most Subclavian pseudoaneurysm patients either present with late upper limb claudication between two to ten years postoperatively [1]. Or present as an acute deterioration to limb threatening ischaemia as a result of emboli to the upper limb [6,7].
All reported cases of brachial plexus injury had similar presentation of severe radicular pain, most commonly in the arm and shoulder. Associated with incomplete but profound sensory loss and paralysis [8,9]. The brachial plexus is susceptible to injury through traction, compression and entrapment. The inflammatory reaction associated with a fracture can cause any adjacent tissues, including the plexus, to become adherent to the fracture fragments and callus [8,10].
Case report
We presenting a case of 82 yrs Right hand dominant male, with background of Parkinson’s disease, who fell whilst running and sustained closed left midshaft clavicle comminuted fracture (Figure 1) and left 2nd and 3rd ribs fractures. Patient was seen in the emergency department and on physical examination had intact sensory and motor function of his left upper extremity, and palpable radial pulsations with pink well perfused hand. Patient was put in a broad arm sling and given an appointment in the fracture clinic the following da.
Patient was seen on the following day in the fracture clinic. On physical examination had intact sensory and motor function of his left upper extremity. Palpable radial pulsations with pink well perfused hand. Decision was taken on conservative management of this injury.
Five days later, patient presented to the emergency department with unremitting, progressive left arm pain, swelling and generalized numbness that has been ongoing over the past 12 hours. On physical examination he was confused because of chest sepsis but observations were stable. There was swelling and extensive bruising over the left clavicle, left shoulder and left anterior chest wall. Neurological assessment reveleaed absent sensations on all the left upper limb dermatomes C5-T1. Motor power of all left upper limb myotomes were MRC grade 0/5. Vascular assessment revealed palpable and equal brachial, radial and ulnar pulsations bilaterally with pink and well perfused left hand.
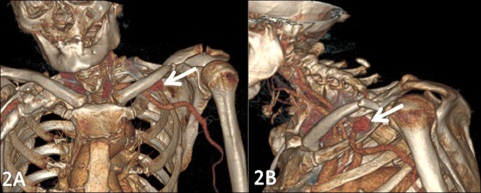
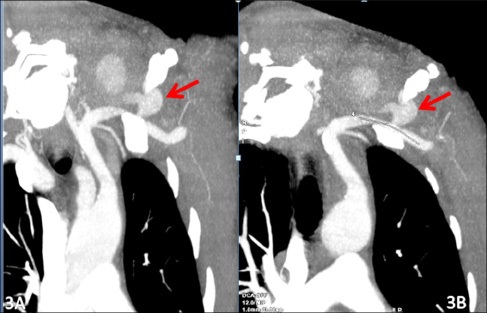
The orthopaedics and vascular teams reviewed the patient and a primary diagnosis of brachial plexus injury was made and further investigated with a CT Thorax Angiogram (Figure 2,3) which delineated the comminuted fracture of the left calvicle and left ribs fracture.
Also, it revealed a Large bilobed 7 X 4 X 5 cm pseudoaneurysm in infraclavicular fossa extending into the root of neck arising from the superior aspect of the 3rd part of the left subclavianartery as it runs over the 1st rib.
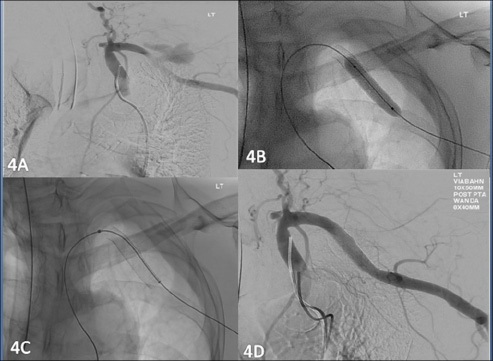
The following day, patient had left subclavian stent insertion (Figure 4). Angiography confirmed the CT findings of a large pseudoaneurysm arising from distal left subclavian artery/Subclavianaxillary junction. This was treated with a 10 X 50 mm Viabahn covered stent, postdilated with an 8 mm balloon with good angiographic result with exclusion of the pseudoaneurysm.
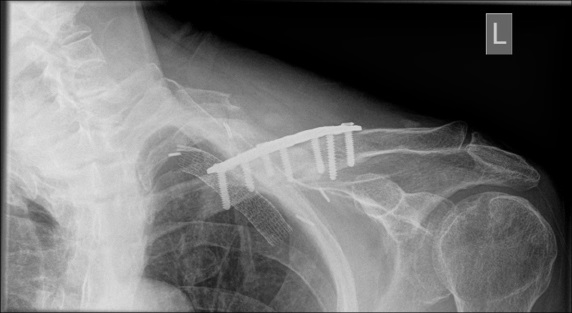
Twelve weeks after the initial injury, the patient had his left clavicle fracture mal-united (Figure 5). There was no improvement in the brachial plexus function. An agreement has been made on exploration of the brachial plexus supra and infraclavicular, and open reduction and internal fixation of the malunited clavicle fracture which were performed sixteen weeks after the initial injury.
During the procedure, thorough dissection around the malunited clavicle fracture was carried out. Brachial plexus was approached and dissected supra-clavicular first. Prominent posterior spike from the lateral end of the clavicle fracture was identified compressing both subclavian artery and brachial plexus. The posterior spike was carefully dissected and excised. Further dissection to mobilise the plexus carried out and infraclavicular dissection carried out to aid the exposure. Tight fascial points and compression points from subclavian artery and brachial plexus were decompressed. Then, clavicle ends were debrided, reduced and fixed in a compression mode (Figure 6).
Patient had his wound checked in two weeks, which was well healed. Patient was allowed active and passive range of motion at four weeks but weight bearing was avoided until fracture union. At follow up, four weeks after the operation, the wound healed up with no complications, clavicle fracture fixation was satisfactory with no signs of loosening and patient started to develop hypersensitive fingertips and had a positive Tinel sign allover his arm, which is suggestive of significant reinnervation.
Discussion
This case emphasizes the following points: Patients should be counseled on symptoms and signs of neurovascular compromise following clavicle fracture. The neurologic status of the arm after clavicle shaft fracture must be serially documented; fractures of the middle one-third of the clavicle are prone to displacement; patients should be advised to report immediately any new symptoms in the arm; when fracture displacement is the cause of brachial-plexus compression then a trial of conservative therapy is indicated; the prognosis for neurologic recovery after this injury is good.
Pseudoaneurysm results from a variety of causes such as infection, trauma, and surgical procedures. The most common mechanism is disruption of arterial continuity with extravasation of blood into surrounding tissue. This results in the formation of fibrous tissue capsule which progressively enlarges because of underlying arterial pressure [11].
Differentiation between simple hematoma and pseudoaneurysm may be difficult by clinical examination alone. Hematoma usually appears shortly after the procedure and tend to resolve in time depending on size, location, and extent of injury whereas pseudoaneurysm may appear later with pulsatile and expanding mass. Duplex USG will help to differentiate between two, and a selective angiogram is necessary to determine precise origin and extent of injury. Because of close anatomic relationship between brachial plexus and subclavian artery in the thoracic inlet, even a small false aneurysm can result in compression injury to the neuroplexus [11].
Because brachial palsy has a poor prognosis when recognition is delayed, an aggressive approach is advocated. Treatment options for pseudoaneurysm are USG-guided compression, percutaneous thrombin injection, coil embolization, endovascular stents, and open surgical repair [12-14].
Conclusion
Patients with clavicle shaft fractures that are amenable to non operative management should be thoroughly counselled on the risks and complications. Any symptoms of brachial plexopathy after midshaft clavicle fracture should arise the suspicion of pseudoaneurysm and confirmed by an angiogram. A symptomatic pseudoaneurysm should be treated without delay to prevent permanent neurological damage.
Declarations
Declaration of conflicting interests: None declared.
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
References
- Clitherow HD, Bain GI. Major neurovascular complications of clavicle fracture surgery. Shoulder Elb. 2015; 7: 3–12.
- Choo HJ, Kim JH, Kim DG. Arterial pseudoaneurysm at the arthroscopic portal site as a complication after arthroscopic rotator cuff surgery: A case report. J Shoulder Elbow Surg. 2013; 22: e15-19.
- Gullo J, Singletary EM, Larese S. Emergency bedside sonographic diagnosis of subclavian artery pseudoaneurysm with brachial plexopathy after clavicle fracture. Ann Emerg Med. 2013; 61: 204–206.
- Shih JS, Chao EK, Chang CH. Subclavian pseudoaneurysm after clavicle fracture - A case report. Taiwan Yi Xue Hui Za Zhi. 1983; 82: 332–335.
- Corriere MA, Guzman RJ. True and false aneurysms of the femoral artery. Semin Vasc Surg. 2005; 18: 216–223.
- Bain GI, Galley IJ, Keogh ARE, Durrant AW. Axillary artery pseudoaneurysm after plate osteosynthesis for a clavicle nonunion: A case report and literature review. Int J Shoulder Surg. 2010; 4: 79–82.
- Shackford SR, Connolly JF. Taming of the screw: A case report and literature review of limb-threatening complications after plate osteosynthesis of a clavicular nonunion. J Trauma. 2003; 55: 840–843.
- Thavarajah D, Scadden J. Iatrogenic postoperative brachial plexus compression secondary to hypertrophic non-union of a clavicle fracture. Ann R Coll Surg Engl. 2013; 95: e55–e57.
- Jeyaseelan L, Singh VK, Ghosh S, Sinisi M, Fox M, et al. Iatropathic brachial plexus injury: A complication of delayed fixation of clavicle fractures. Bone Jt J. 2013; 95-B: 106–110.
- Carofino BC, Brogan DM, Kircher MF, Elhassan BT, Spinner RJ, Bishop AT, et al. Iatrogenic nerve injuries during shoulder surgery. J Bone Joint Surg Am. 2013; 95: 1667–1674.
- Mol TN, Gupta A, Narain U. Brachial plexus compression due to subclavian artery pseudoaneurysm from internal jugular vein catheterization. Indian J Nephrol. 2017; 27: 148–150.
- Pastores SM, Marin ML, Veith FJ, Bakal CW, Kvetan V. Endovascular stented graft repair of a pseudoaneurysm of the subclavian artery caused by percutaneous internal jugular vein cannulation: Case report. Am J Crit Care Off Publ Am Assoc Crit-Care Nurses. 1995; 4: 472–475.
- Mc Connell PI, Rehm J, Oltman DL, Lynch TG, Baxter BT, et al. Thrombin injection for treating a subclavian artery pseudoaneurysm. Surgery. 2000; 127: 716–718.
- Marin ML, Veith FJ, Panetta TF, Cynamon J, Sanchez LA, Schwartz ML, et al. Transluminally placed endovascular stented graft repair for arterial trauma. J Vasc Surg. 1994; 20: 466–473.