Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
A rare case of mucosal metastases 14 years after resolution of a primary uveal melanoma
Naz Ece Kundak1; Raaid Musa1; Serkan Celik2; Bala Başak Oven2; Mustafa Kemal Demir3
1 Bahçeşehir University Faculty of Medicine, Istanbul, Turkey.
2 Yeditepe University Faculty of Medicine, Department of Medical Oncology, Istanbul, Turkey.
3 Bahçeşehir University Faculty of Medicine, Department of Radiology, Istanbul, Turkey.
*Corresponding Author: Naz Ece Kundak
Bahçeşehir University Faculty of Medicine, Istanbul,
Turkey.
Email: nazece.kundak@bahcesehir.edu.tr
Received : Nov 15, 2021
Accepted : Jan 04, 2022
Published : Jan 11, 2022
Archived : www.jcimcr.org
Copyright : © Kundak NE (2022).
Abstract
Uveal melanoma has a high metastasis rate. Following the initial diagnosis, up to 50% of patients are affected by late recurrence and gastrointestinal metastasis is found to be one of the least frequent. We report the case of a 47-year-old woman who underwent proton therapy for uveal melanoma. Fourteen years after the initial diagnosis, she presented to the hospital complaining of an enduring gas in stomach. Dark colored, metastatic lesions were discovered in gastric mucosa during endoscopy and hyperintense hepatic lesions were spotted in T1 weighted MR imaging. Long term metastasis is commonly seen in patients with uveal melanoma and its management is more difficult when compared to other melanoma types, hence regular follow-ups are crucial for patient well-being.
Keywords: uveal melanoma; gastric metastases; mucosal metastases; gastric mucosa; intraocular tumors.
Citation: Kundak NE, Musa R, Celik S, Oven BB, Demir MK. A rare case of mucosal metastases 14 years after resolution of a primary uveal melanoma. J Clin Images Med Case Rep. 2022; 3(1): 1549.
Introduction
The most frequent intraocular tumor in adults is Uveal Melanoma (UM). UM is an inclusionary term for neoplasms of melanocytes residing in iris, ciliary body, and the choroid. The highest incidence for uveal melanomas is seen in choroid with a rate as high as 90% [1]. Primary UMs are considered responsive to treatment and short-term metastatic melanoma is rarely found, only present in less than 1% of patients at the time of early screenings [2]. Conversely, after the definite treatment of primary tumor, metastasis rate tends to increase over long time periods, indicating a non-detectable dissemination might have occurred before medical attention [3]. Malignant uveal melanoma tends to favor liver for metastasis and gastrointestinal tract is seldom affected [1]. Due to the rarity of the condition, medical literature on this malignancy is scarce and thus, we present a case report of a patient with a late metastasis of malignant melanoma to the gastrointestinal tract.
Case presentation
A 48-year-old woman presented with long standing bloating, abdominal pain and weight loss. The patient illustrated that the pain was mostly related to the bloating she had been having and described it as “diffuse”. She did not have any dysphagia, vomiting or gastrointestinal bleeding of any form.
Her history was significant for melanoma of the choroid and ciliary body of the right eye that was diagnosed fourteen years ago. It was located at the lower temporal section and measured 22.7 X 19.8 mm with a thickness of 10.4 mm. The tumor had a classification T3 N0 M0 (Stage 2B). It was treated with proton therapy with 60 Gray in four fractions. The patient was further routinely followed up with ultrasonography and cranial Magnetic Resonance Imaging (MRI). Aside from this, the patient has not had any other significant health history.
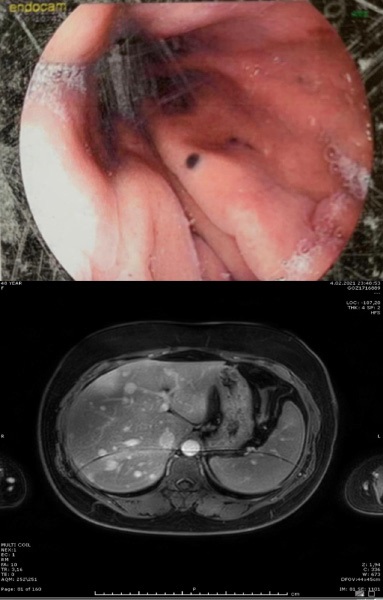
With the presenting symptoms, the patient was sent for a gastroduodenoscopy. The results were significant for a smooth, hyperpigmented mucosal lesion of about 2 mm at the corpus, of which a biopsy was taken (Figure 1a). The results of the biopsy stated a metastatic melanoma with infiltration into the lamina propria. Immunohistochemical examination with SOX10 confirmed this diagnosis.
For this reason, she was sent for PET/CT which shows focal FDG involvement in the stomach corpus and a suspicious involvement of the liver also. A follow-up MRI (Figure 1b) of the abdomen revealed multiple metastatic lesions in the liver, pancreas corpus and probable lesions in the posterior right kidneys. Aside from these, there were no other sites of the disease.
With the diagnosis of metastatic melanoma, the patient was referred for genetic testing, which was done with the next generation sequencing, came out positive for a GNAQ and TP53 mutation and negative for BRAF gene.
The patient started to receive dual therapy with Ipilimumab and Nivolumab. As of eight months after the beginning of the aforementioned treatment, the condition of the patient remains stable.
Discussion
Imaging features of HCC on MRI
Long-term metastasis is frequent in patients with UM and disease recurrence is common in liver [1]. Therefore in patients with an UM history even the most common or relatively usual complaints must be examined thoroughly. Since the manifestation of the disease can be accompanied with mild to severe complaints, symptoms might appear discrete, non-specific and unconnected. Our case report implies that the metastasis risk is still existent years after the initial diagnosis and further inspection with utmost care is vital in any report of discomfort. In gastrointestinal metastases, patients may present with complaints of abdominal gas, abdominal pain and weight loss.
After the presenting symptoms were evaluated, our patient had undergone gastroduodenoscopy. Hyperpigmented mucosal lesions were detected during the procedure. Biopsies were taken from the mentioned lesions and SOX-10 was found positive in immunohistochemical staining. Further genetic testing showed GNAQ and TP53 mutations and the specimens were negative for BRAF gene mutation. In patients with uveal melanoma, GNAQ and GNA11 are commonly affected by mutations with an approximate rate of %80 whereas non-uveal melanomas rarely have a gene profile involving mutant GNAQ and GNA11 [4]. Despite the low affinity of GI tract for UM metastases, the results indicated a recurrence of melanoma after 14 years of initial diagnosis.
In patients aged between 21-60 years, metastasis rate is estimated as 12% within 5 years, 23% within 10 years, and 34% within 20 years [5]. Most common metastasis site for uveal melanoma is the liver (88%) and gastrointestinal metastasis is considered unusual (~1%) [1]. Long term metastasis should be considered if a patient has a history with UM. At early presentation, metastasis detection rate in patients is <1%, which is correlated with poor clinical indications [6]. Strikingly, long-term data collected from treated primary UM patients reveals considerably higher metastasis rates; 31%, 45% and almost 50% respectively for 5-year, 15-year and 25-year follow-ups [7].
Characterizing indeterminate liver lesions in a patient with cirrhosis due to cardiac congestion: Beyond LI-RADS
PET/CT imaging of the patient demonstrated stomach involvement and MRI revealed that the liver was also a metastatic site. Since PET/CT imaging was not enough to demonstrate involvement of the liver in our patient, further scanning via magnetic resonance might be helpful to expose the full extent of the disease when hepatic metastasis is suspected.
Median survival time is poor for patients with UM metastasis. Progression of symptoms in patients who are treated with suitable therapy is known to be considerably slower when compared to those who are not [8]. Median survival is reported as 6.3 months for the former and 1.7 months for the latter [8]. In our case, immunotherapy was promptly started after the diagnosis and a combination of Ipilimumab and Nivolumab was used as single agent immunotherapy fails to induce significant response in metastatic UM.
A combination of nivolumab and ipilimumab is expected to show improved results on UM metastases when compared to single-agent immune checkpoint blockade [3]. Ipilimumab monotherapy showed no overall response rate (0%) and a median Overall Survival (OS) of 6.8 months in a phase II trial whereas the OS was 19.1 months and response rate was 18% with nivolumab and ipilimumab; favoring the combination over single-agent checkpoint inhibition [9].
Since molecular alterations and clinical onset of the diseases vary between melanoma types, differences in efficacy rates are expected even when an identical treatment strategy is applied. Notably, in one of the trials, an increase in OS was recorded only in patients with extrahepatic metastases and combination therapy showed higher efficacy in metastatic cutaneous melanoma [9].
A trial for mucosal melanoma treatment also showed a higher efficacy for combination therapy. In single agent therapy with nivolumab, median progression-free OS for mucosal melanoma was reported as 3 months and objective response rate was 23.3% whereas median progression-free OS was 5.9 months with objective response rates of 37.1% when nivolumab and ipilimumab were collectively used [10].
Conclusion
Although uveal melanoma is a treatable disease when early diagnosis is evident, metastasis risk still exists for many years after the initial curative treatment. Given the long metastatic period and relatively harder management when compared to metastatic cutaneous melanoma, the importance of long term follow ups including gastrointestinal regions stands out strikingly.
References
- Jochems A, Van der Kooij MK, Fiocco M, Schouwenburg MG, Aarts MJ, et al. Metastatic Uveal Melanoma: Treatment Strategies and Survival-Results from the Dutch Melanoma Treatment Registry. Cancers. 2019; 11: 1007. https://doi.org/10.3390/cancers11071007
- Diener West M, Reynolds SM, Agugliaro DJ, Caldwell R, Cumming K, et al. Screening for metastasis from choroidal melanoma: The Collaborative Ocular Melanoma Study Group Report 23. Journal of clinical oncology: Official journal of the American Society of Clinical Oncology. 2004; 22: 2438–2444. https://doi. org/10.1200/JCO.2004.08.194
- Eskelin S, Pyrhönen S, Summanen P, Hahka Kemppinen M, Kivelä T, et al. Tumor doubling times in metastatic malignant melanoma of the uvea: Tumor progression before and after treatment. Ophthalmology. 2000; 107: 1443–1449. https://doi. org/10.1016/s0161-6420(00)00182-2
- Livingstone E, Zaremba A, Horn S, Ugurel S, Casalini B, et al. GNAQ and GNA11 mutant nonuveal melanoma: a subtype distinct from both cutaneous and uveal melanoma. Br J Dermatol. 2020; 183: 928-939. https://doi.org/10.1111/bjd.18947
- Shields CL, Kaliki S, Furuta M, Mashayekhi A, Shields JA, et al. Clinical spectrum and prognosis of uveal melanoma based on age at presentation in 8,033 cases. Retina (Philadelphia, Pa.). 2012; 32: 1363–1372. https://doi.org/10.1097/IAE.0b013e31824d09a8
- Diener West M, Reynolds SM, Agugliaro DJ, Caldwell R, Cumming K, Earle JD, et al. Screening for metastasis from choroidal melanoma: The Collaborative Ocular Melanoma Study Group Report 23. Journal of clinical oncology : Official journal of the American Society of Clinical Oncology. 2004; 22: 2438–2444. https://doi.org/10.1200/JCO.2004.08.194
- Kujala E, Mäkitie T, Kivelä T. Very long-term prognosis of patients with malignant uveal melanoma. Investigative ophthalmology & visual science. 2003; 44: 4651–4659. https://doi.org/10.1167/ iovs.03-0538
- Lane AM, Kim I K, Gragoudas E S. Survival Rates in Patients After Treatment for Metastasis From Uveal Melanoma. JAMA ophthalmology. 2018; 136: 981–986. https://doi.org/10.1001/ jamaophthalmol.2018.2466
- Pelster MS, Gruschkus SK, Bassett R, Gombos DS, Shephard M, et al. Nivolumab and Ipilimumab in Metastatic Uveal Melanoma: Results From a Single-Arm Phase II Study. Journal of Clinical Oncology. 2020. JCO.20.00605. doi:10.1200/jco.20.00605
- Sandra PD Angelo, James Larkin, Jeffrey A Sosman, Celeste Lebbé, Benjamin Brady, et al. Journal of Clinical Oncology. 2017; 35: 226-235.