Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
Non radiographic axial spondyloarthropathy in tuberculoid leprosy
Sujit Kumar Bhattacharya
Professor and Dean (Retired), Faculty of Medicine, Institute of Medical Science, Banaras Hindu University B 15/14-A2, Faridpura, Varanasi-221001, India.
*Corresponding Author: Sujit Kumar Bhattacharya
Professor and Dean (Retired), Faculty of Medicine,
Institute of Medical Science, Banaras Hindu University
B 15/14-A2, Faridpura, Varanasi-221001, India.
Email: sbhattacharya78@gmail.com
Received : Nov 18, 2021
Accepted : Jan 06, 2022
Published : Jan 13, 2022
Archived : www.jcimcr.org
Copyright : © Bhattacharya SK (2022).
Abstract
Rationale: Axial Spondyloarthirtis (ax-SpA) includes a non-radiographic variant, called Non Radiographic Axial Spondyloararthrophy (nr-ax-SpA), which is a very rare type of arthritis of spine. Hansen disease or Leprosy is a chronic infectious disease with various clinical manifestations, which is endemic in India. Various arthritic manifestations have been reported in leprosy patients. Though the condition is treatable and reversible, it may remain unrecognized and undisclosed in patients suffering with Leprosy.
Patient concern: Here we illustrate a case of non-radiographic axial spondyloararthrophy in 40-year old male with diagnosis of borderline Hansen’s disease (leprosy) 15 years ago. Patient had reported chronic back pain for over five years, leading to stiffness of dorsal spine, and presented swollen wrist joint. Leprosy symptoms presented include dry hyper-pigmented, non-ulcerating, hypo-aesthetic (pain and temperature) patches on both legs, buttocks, upper abdomen and iliac crest.
Diagnosis: The patient was diagnosed as border line tuberculoid leprosy with nr-ax-SpA.
Treatments: He was treated with in domethacin, leflunomide and hydroxy-chloroquine, along with a standard treatment regimen to combat BT Leprosy. Follow up at 3 and 6 month revealed significant improvement.
Keywords: spondyloarthritis; leprosy; hydroxy-chloroquine.
Citation: Bhattacharya SK. Non radiographic axial spondyloarthropathy in tuberculoid leprosy. J Clin Images Med Case Rep. 2022; 3(1): 1561.
Introduction
Spondyloarthritis (SpA) is a group of interrelated diseases with axial and peripheral inflammatory joint involvement along with many extra-articular manifestations [9]. The term Axial Spondyloarthirtis (ax-SpA) has been coined in the year 2009 [11] . A subset of Axial Spondyloarthritis (ax-SpA) has been identified where in patients with in-flammatory back disease shows no radiographic changes, and has been classified as Non-Radiographic Axial Spondyloarthritis (nr-ax-SpA) [12]. Some authors view this as a different presentation of a single disease or as a continuum [6].
Hansen disease, commonly known as leprosy, is a chronic infectious disease caused by Mycobacterium leprae, is characterized by damages to the skin and peripheral nerves. It has also been reported to invade visceral and bone joints. Due to the complex and variable clinical manifestations, it is frequently misdiagnosed. In cases of leprosy, rheumatological manifestations are frequent, although often under-recognized [3]. Here we present a case where in a male patient with borderline tuberculoid leprosy (BT-L) hadnr-ax-SpA.
Case presentation
A 40 year old male patient, presented with chronic back pain of more than 5 year duration. Pain started at lumbo sacral region, which was relieved on movement. Over the past one year, pain had spread to dorsal spine as well as to neck, with resultant stiffness and restriction of movement in these regions. Both of his wrist joints had swelling and pain. Bogginess and fluctuations were noted along muscle tendons at both the wrist joints.
He has been diagnosed to be suffering from Hansen’s disease (BT-L) for over 15 years and was getting treated intermittently over this period of time. Social and family histories were unremarkable. He was working as an office assistant and had the habit of chewing tobacco. The man was of average built, weighing 70 Kgs, with Blood Pressure (BP) 150/90 mmhg. Oedema, palor, and lymphadenopathy were absent. Body temperature was normal.
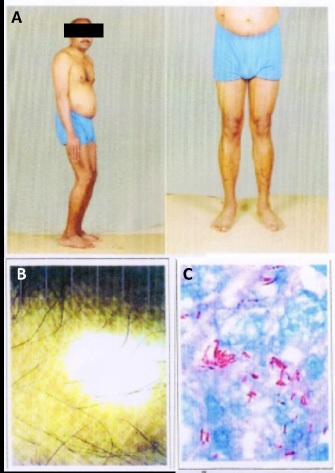
Dermatological examination revealed dry hyper pigmented, non-ulcerating, hypo aesthetic (pain and temperature) patches on both legs and buttocks. Hypo pigmented area were also found on upper abdomen and iliac crest (Figure 1A,B). Ulnar and posterior tibial nerves were think end but not tender. Examination of spine shows tenderness in lumbosacral and upper dorsal region. The patient also had a positive Schoberg’s test. Both his wrist joints were swollen and tender. Result of investigation was as follows: Hemoglobin 12.0 gm per dl, ESR 26 m for the first hour. Blood glucose, urea, creatinine and uric acid levels were normal. Serum rheumatoid factor (Method ELISA) and anticcp2ab were within normal limits. HLA-B27 assay was negative, so were tests for HIV.I, II, and blood VDRL. Radiographic examination- MRI, showed a few budding osteophytes at lumber region. Saorociliac joint were normal. Signal intensity on T2 W1 of marrow was normal at all levels of spine. Skin scrapping from the diseased area revealed bunches of Mycobacterium leprae (Figure 1C).
This patient was diagnosed as border line tuberculoid leprosy with nr-ax-SpA. He was put on indomethacin, Leflunomide and hydroxy-chloroquine along with a standard treatment regimen to combat BT Leprosy. Follow up at 3 and 6 month revealed significant improvement.
Discussion
Leprosy is a chronic infectious disease. Apart from cutaneousmanifestations, nail changes and leprotic neuropathy involving peripheral nerves, are other key manifestation of this disease. Musculoskeletal involvement can occur inform of peripheral arthritis which may go unrecognized or undisclosed [7,10]. Axial (spine) manifestation are of rare occurrence in leprosy [2,4]. In the case under discussion, while the patient was suffering from leprosy (BT) for a long time, but only recently started experiencing inflammatory back pain, along with wrist joint Arthritis. Restriction of spine movement was profound. Radiographic examination of spine and sacroiliac joint showed no gross abnormality. His HLAB27 was negative; so were common serological markers for arthropathy.
Non radiological, non HLA-B27 spondyloarthropathy, with or without sacroilitis, pose unique diagnostic dilemma, especially when occurring in a leprosy patient. In their series, Prasad and colleagues had observed spondyloarthropathy in 7 out of 44 leprosy cases examined in a tertiary super-specialty referral hospital clinic [10]. It was remarkable that all of these cases had radiological changes, but the symptoms were not reversible in all.
Arthritic manifestations in leprosy do occur in association with a reactive episode, and may remit with treatment [8]. Occasionally these factures are seen independent of reaction, and fail to resolve despite adequate treatment [1]. In the case presented here, despite long duration of the disease (BT-L), features suggestive of a reactive episode were conspicuous by their absence. Previously, cases has been reported where Mycobacterium leprae been cultured from a case with spondylodiscitis of cervical region [4]. Conversely, patients with rheumatoid arthritis undergoing treatment with Enaercept, have been reported to have developed leprosy [4,5]. An auto immune central axis with IL-23/IL-17 pathway is believed to be operative in pathogenesis, of axial spond-arthropathy [6], both in nr.ax. Spond and classical groups.
Conclusions
Leprosy is a common malady in India. Muscloskeletal manifestations, do occur in this disease but are often missed. Non radiographic axial spond-Arthropathy is a new entity in association with leprosy. The present case serves as illustration.
References
- Bhattacharya S, Girgla H, Gurmohan S. Necrotizing reaction in lepromatous leprosy. Leprosy review. 1973; 44: 29-32.
- Cossermelli Messina W, Cossermelli W. Articular inflammatory manifestations in patients with different forms of leprosy. The Journal of rheumatology. 1998; 25: 111-119.
- Gao LN, Zhong B, Wang Y. Rheumatoid arthritis-like features in Hansen disease: A case report. Medicine. 2018; 97: e11590.
- Kim SJ, Lee TH, Shin JJ, Chae GT. Leprotic cervical spondylodiscitis. European Spine Journal. 2010; 19: 211-215.
- Oberstein EM, Kromo O, Tozman EC. Type 1 reactions in Hansens’s disease with exposure to adalimubab a case report. Arthritis Rheumatology. 2008; 59: 1040-1043.
- Paine A, Ritchlin CT. Targeting the interleukin-23/17 axis in axial spondyloarthritis. Curr Opin Rheumatol. 2016; 28: 359-367.
- Pal S, Singh S, Bhattacharya S. Immunological parameters in leprosy patients with and without arthritis. Journal of the Indian Medical Association. 1995; 93: 266-267.
- Pereira H, Ribeiro S, Pennini S, Sato E. Leprosy-related joint involvement. Clinical rheumatology. 2009; 28: 79.
- Perez Fernandez OM, Mantilla RD, Cruz Tapias P, Rodriguez Rodriguez A, Rojas Villarraga A, et al. Spondyloarthropathies in autoimmune diseases and vice versa. Autoimmune Dis. 2012; 2012, 736384.
- Prasad S, Misra R, Aggarwal A, Lawrence A, Haroon N, Wakhlu A, et al. Leprosy revealed in a rheumatology clinic: A case series. International Journal of Rheumatic Diseases. 2013; 16: 129-133.
- Rudwaleit M, van der Heijde D, Landewe R, Listing J, Akkoc N, et al. The development of Assessment of Spondylo Arthritis international Society classification criteria for axial spondyloarthritis (part II): Validation and final selection. Ann Rheum Dis. 2009; 68: 777-783.
- Rudwaleit M, van der Heijde D, Landewe R, Listing J, Akkoc N, et al. The development of Assessment of Spondylo Arthritis international Society classification criteria for axial spondyloarthritis (part II): Validation and final selection. Ann Rheum Dis. 2009; 68: 777-783.