Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 2
Young pregnant woman with hyperemesis gravidarum and cognitive alterations
Sandra Badial-Ochoa; Arturo Gonzalez-Lara; Melissa Hernandez-Vega; Felipe Alberto Monternach-Aguilar; Ildefonso Rodriguez-Leyva*
Neurology Service, Medicine Faculty, Universidad Autonoma de San Luis Potosi, Hospital Central, San Luis Potosi, SLP, Mexico.
*Corresponding Author: Ildefonso Rodriguez-Leyva
Neurology Service, Medicine Faculty, Universidad
Autonoma de San Luis Potosi, Hospital Central, San
Luis Potosi, SLP, Mexico.
Email: ilrole@yahoo.com.mx
Received : Nov 30, 2021
Accepted : Jan 11, 2022
Published : Jan 18, 2022
Archived : www.jcimcr.org
Copyright : © Rodriguez-Levya I (2022).
Abstract
A 26-year-old woman, 21.6 weeks gestation, was diagnosed with hyperemesis gravidarum a month earlier. She continued with vomiting and started with weakness in extremities, unsteadiness and slurred speech. She was hospitalized, had hypokalemia (2 mEq/L), received intravenous potassium phosphate replacement, and was discharged. One week later, she started with dizziness and confusion. In the disease course, she received medical attention focused on the apparent weakness and gastrointestinal alterations. Three weeks later, the patient started with inattention, and she came to our institution. For this time, she had developed nystagmus, inability to complete eye movements, confabulation and confusion. The diagnosis then was Wernicke-Korsakoff encephalopathy, a neurological complication of thiamine deficiency. MRI was the primary tool to confirm the diagnosis showing hyperintensity in the paramedian thalamic region, periaqueductal grey matter and mammillary bodies. She was discharged after treatment in better condition but still with cognitive and coordination problems. Management should begin as soon as possible with thiamine substitution; the delay will cause more important neurological sequelae and increase mortality up to 10 to 20%.
Citation: Badial-Ochoa S, Gonzalez-Lar A, Hernandez-Vega M, Monternach-Aguilar FA, Rodriguez-Leyva I. Young pregnant woman with hyperemesis gravidarum and cognitive alterations. J Clin Images Med Case Rep. 2022; 3(1): 1577.
Background
Wernicke-Korsakoff encephalopathy mainly affects people who have a thiamine deficiency due to chronic alcoholism. Other etiologies that can cause this problem are malnutrition, prolonged parenteral nutrition, neoplasms, immunodeficiency syndromes, liver disease, hyperthyroidism, anorexia nervosa, and hyperemesis gravidarum [1]. Vitamin B1 or Thiamin is an essential B-complex vitamin obtained from the diet that acts as a cofactor for more than 24 enzymes. Most importantly, pyruvate dehydrogenase for ATP production in the Krebs cycle, transketolase for lipid metabolism, branched-chain amino acids, production and maintenance of myelin sheath, and 2-oxoglutarate dehydrogenase for the synthesis of acetylcholine and GABA. Vitamin B1 is also essential in maintaining osmotic gradients across cell membranes, especially in the central nervous system. Therefore, its deficiency is associated with intracellular and extracellular oedema that can progress to glial cell proliferation, neuronal demyelination, and eventually cellular degeneration. In hyperemesis gravidarum, thiamine deficiency results from the combination of poor nutritional intake, frequent vomiting, and increased metabolic demands of pregnancy [2].
Wernicke encephalopathy is acute and may present with varied signs or symptoms in patients with underlying deficiency or malnourishment[3]. The classic triad of gait ataxia, eye signs (nystagmus, ophthalmoplegia), and global confusion is more common in alcohol-related cases [4]. The main characteristic of Wernicke’s encephalopathy is altered eye movements, especially the presence of nystagmus. Other manifestations are associated with the oculomotor, abducens, and vestibular nuclei, causing limitation and alteration in conjugate gaze. Pupillary sluggishness, ptosis, and pupillary asymmetry may also be present. Another significant finding in Wernicke’s encephalopathy is the presence of gait ataxia, in which patients will present a wide-supported gait.
Disorientation and altered sensorium characterize encephalopathy. Some patients present a spontaneous confabulation especially noted in the acute Wernicke state. A severely depressed level of consciousness leading to coma and even death may occur in less than 5% of cases [1].
Case presentation
The family brought a 26-year-old woman at 21.6 weeks gestation to the emergency department with a story of weakness that developed inattention and paretic eyes. Her illness began one month earlier with nausea and incoercible vomiting. She was diagnosed with hyperemesis gravidarum and hypokalemia (2 mEq/L) and received a reposition with potassium phosphate intravenous with the improvement of the weakness. However, three weeks later, she continued vomiting and started with cognitive impairment characterized by inattention, confusion and slurred speech. Also, she begins with nystagmus and an inability to complete eye movements, vertigo and ataxia in four limbs. The family was not present to help with the interrogation, and the patient mentioned she was a drug consumer. Hence, we suspected an intoxication. However, when her family arrived, and we could talk to them, we realized that she was confabulated and never used drugs.
The patient depicts a subacute clinical course characterized by inattention, oculomotor abnormalities, gait disorder and dysarthria, in the context of a young previously healthy woman with a second-trimester pregnancy, presenting after an episode of hyperemesis gravidarum with the hallmark of nausea, incoercible vomiting leading to volume depletion and electrolytic disturbance. During pregnancy, some physiological changes can predispose to certain types of neurological complications (preeclampsia/eclampsia, cerebral venous thrombosis, posterior cerebral vasoconstriction syndrome, to mention a few) or some states related to vitamin and mineral deficits due to the increase of requirements to supply the metabolism of the baby and the mother adequately. The etiological diagnosis includes metabolic causes like severe hypokalemia (due to gastrointestinal losses) and persistent vomiting. In addition, some electrolytes could be altered significantly due to a reduced oral intake, such as potassium, calcium, magnesium, sodium, and bicarbonate. The decrease in the levels of these elements can also generate changes in the mental status. It is also essential to rule out infectious diseases involving the central nervous system since they can be lifethreatening in patients with acute and subacute mental status changes.
Investigations
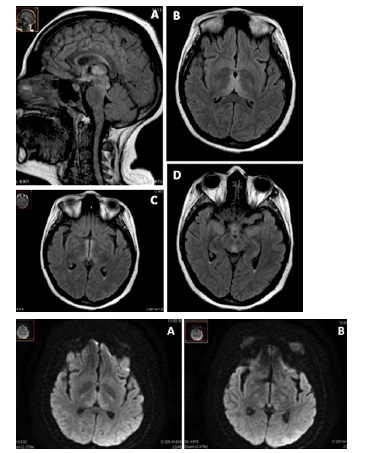
Along with the approach we took with our patient, we excluded alterations in electrolytes. After the correction of hypokalemia, there was no other change, the sodium remained at normal levels, and there was no variation documented that could cause an osmotic myelinolysis. In the beginning, with not knowing her medical background and the chronological appearance of symptoms. We performed routine laboratories in parallel; the glucose was average, complete blood count, thyroid function test, hepatic function test, serum creatinine, and urea were all unremarkable. Serological tests against HIV, Hepatitis C and B, and a TORCH panel were negative. The toxicology screen was negative for any drug. The initial CT scan showed no sign of oedema, venous thrombosis, ischemic or hemorrhagic changes. We performed a lumbar puncture, CSF gram stain, glucose, proteins, and cells were expected, the cultures showed no growth. A brain MRI showed High FLAIR/T2 signal lesions in the corpus callosum, hypothalamus, fornix, mammillary bodies, thalamus, and midbrain (Figure 1) with DWI restricted diffusion in the same areas (Figure 2), which it’s a characteristic finding in Wernicke-Korsakoff encephalopathy.
Differential diagnosis
Wernicke encephalopathy is acute and may present with varied signs or symptoms in patients with underlying deficiency or malnourishment [3]. The classic triad of gait ataxia, eye signs (nystagmus, ophthalmoplegia), and global confusion is more common in alcohol-related cases [4]. The main characteristic of Wernicke’s encephalopathy is altered eye movements, especially the presence of nystagmus. Other manifestations are associated with the oculomotor, abducens, and vestibular nuclei, causing limitation and alteration in conjugate gaze. Pupillary sluggishness, ptosis, and pupillary asymmetry may also be present. Another significant finding in Wernicke’s encephalopathy is the presence of gait ataxia, in which patients will present a wide-supported gait.
The differential diagnosis must include deep cerebral venous thrombosis, top-of-the-basilar syndrome, paramedian thalamic syndrome, viral infection (like Japanese encephalitis o influenza). Another possibility is an atypical Creutzfeldt-Jakob disease may present with bilaterally symmetric lesions in the medial thalami. Metronidazole induced encephalopathy to make symmetric signal-intensity alterations of dentate nuclei, midbrain, dorsal pons, medulla, cranial nerves nuclei, red nuclei, corpus callosum and splenium [5].
It is also essential to rule out hepatic encephalopathy, alcohol withdrawal syndrome, delirium tremens or chronic hypoxia [1].
Treatment
Treatment should be started with intravenous thiamine as soon as possible, even without having laboratories that confirm thiamine deficiency. We started the treatment with thiamine IV 500 mg IV TID for three days and continued with 200 mg IV TID for one week. After that, we switch to oral ingest with 100 mg daily until her discharge. Initial oral treatment is not recommended due to absorption defects associated with malnourished and alcoholic patients [6].
Wernicke encephalopathy is a progressive disease, and even with treatment, mortality can be 10-20%. Ocular alterations usually resolve within the first hours of treatment. However, horizontal nystagmus may persist in up to 60% of patients [7]. Gait disturbances may persist for several months in up to 30% of patients. These present a low percentage of improvement regarding cognitive alterations, 20% significantly when associated with Korsakoff syndrome [8].
Outcome and follow-up
The patient was treated with thiamine, her physical condition and hygiene improved. She had been admitted with pediculosis that required treatment. The stories she confabulated were very much concerning what the physicians could question her about different items. For example, she had accepted that she used drugs and all the presented were known to her, when in fact, the husband confessed to us that she was not addicted or exposed to them. She required intensive care because she had no diagnosis initially, she was pregnant, and the product had to be protected. However, it was damaged, and the patient had an abortion. Once the MRI was done, autoimmune problems were ruled out and also considered, supported by the fact that the immunological profile was unremarkable. With the administration of thiamine, the patient gradually improved, she was transferred to the general ward. Although she persisted with discrete nystagmus, her ophthalmoplegia improved, as did her coordination, and she stopped confabulating, although she continued with amnesic problems.
Discussion
The diagnosis of this problem begins with clinical suspicion in a patient with associated risk factors. In general, laboratory studies may result in normal parameters, except for serum thiamine and erythrocyte transketolase activity may be decreased, in addition to elevated serum pyruvate [9]. The evaluation of cerebrospinal fluid is not relevant since it may be expected and is of help only to rule out other pathologies. Tomography is not essential in this pathology, and, like cerebrospinal fluid, it is necessary for differential diagnosis, especially when magnetic resonance imaging (MRI) is not possible. MRI is the diagnostic method of choice; in T2/FLAIR sequences, hyperintense bilateral lesions are observed in the paramedian thalamic region, the most frequent site, followed by periaqueductal grey matter, mammillary bodies (the area that enhances the most), tectum, and less frequently the dorsal medulla, spinal cord, cerebellum, splenium, and cortical region. In diffusion, they will restrict the areas mentioned above and in T1, mainly in severe cases, hyperintensities in the mammillary bodies and thalamus corresponding to areas of petechial haemorrhage [10]. It is because of the distribution of these lesions, the primary differential diagnoses correspond to Optic Neuromyelitis Spectrum, Cerebral Thrombosis of the deep venous system, Percheron artery infarction, or viral infections [11].
Treatment should be started with intravenous thiamine as soon as possible, even without having laboratories that confirm thiamine deficiency. The recommended dose is 500 mg IV every 8 hours for two days followed by 100 to 250 mg IV or IM every 8 hours for one week and then 100 mg PO every 24 hours until hospital discharge. Initial oral treatment is not recommended due to absorption defects associated with malnourished and alcoholic patients [6].
Wernicke encephalopathy is a progressive disease, and even with treatment, mortality can be 10-20%. Ocular alterations usually resolve within the first hours of treatment. However, horizontal nystagmus may persist in up to 60% of patients [7]. Gait disturbances may persist for several months in up to 30% of patients. These present a low percentage of improvement regarding cognitive alterations, 20% significantly when associated with Korsakoff syndrome [8].
Wernicke encephalopathy is a pathology that must be suspected in all patients with nutritional deficiencies and typical symptoms of ocular disorders, ataxia, and encephalopathy. In most cases, the three alterations are not found in the same patient. MRI is the primary tool to confirm the diagnosis in which alteration must be sought in the paramedian thalamic region, periaqueductal grey matter, and mammillary bodies. Management should begin as soon as possible, and that its delay will cause more significant neurological sequelae and increase mortality up to 10 to 20%.
Pearls to know
• The Wernicke-Korsakoff syndrome refers to a pathology caused by thiamine deficiency mainly associated with alcoholism and malnutrition but may have other origins, as in this case.
• Wernicke’s encephalopathy is usually the acute manifestation of the problem and consists of inattention, ataxia, nystagmus and ophthalmoplegia. Korsakoff’s presentation is usually more chronic and associated with the presence of amnesia and confabulation. But both problems are a continuum.
• Hyperemesis gravidarum associated with malnutrition may favour this problem, and if it is not identified, the consequences may even be fatal for the mother and her product.
• Differential diagnoses include cerebral deep vein thrombosis, NMOSD (neuromyelitis optic spectrum disorders), Percheron artery infarction, and Bickerstaff’s encephalitis.
• Suspicion on its own requires immediate treatment with high-dose intravenous thiamine, especially if there are absorption problems.
• The sequelae and mortality are high. In addition, once the patient has amnesia problems, it is difficult to recover completely.
References
- Vasan S, Kumar A. Wernicke Encephalopathy. [Updated 2020 Nov 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021.
- Chiossi G, Neri I, Cavazzuti M, Basso G, & Facchinetti F. Hyperemesis Gravidarum Complicated by Wernicke Encephalopathy: Background, Case Report, and Review of the Literature. Obstetrical & Gynecological Survey. 2006; 61(4): 255- 268.
- Latt N, Dore G. Thiamine in treating Wernicke encephalopathy in patients with alcohol use disorders. Intern Med J. 2014; 44(9): 911-5
- Welsh A, Rogers P, Clift F. Nonalcoholic Wernicke’s encephalopathy. CJEM. 2016; 18(4): 309-12.
- Ota Y, Capizzano A, et al. Comprehensive review of Wernicke encephalopathy: pathophysiology, clinical symptoms and imaging findings. Japanese Journal of Radiology. 2020; 38: 809- 820.
- Day E, Bentham P, Callaghan R, et al. Thiamine for WernickeKorsakoff Syndrome in people at risk from alcohol abuse. Cochrane Database Syst Rev. 2004; CD004033.
- Victor M, Adams RA, Collins GH. The Wernicke-Korsakoff syndrome and related disorders due to alcoholism and malnutrition, FA Davis, Philadelphia. 1989.
- Carota A, Schnider A. Dramatic recovery from prolonged Wernicke-Korsakoff disease. Eur Neurol. 2005; 53:45.
- Davies SB, Joshua FF, Zagami AS. Wernicke’s encephalopathy in a non-alcoholic patient with a normal blood thiamine level. Med J Aust. 2011; 194: 483.
- Ashraf VV et al. Wernicke’s encephalopathy due to hyperemesis gravidarum: clinical and magnetic resonance imaging characteristics. J Postgrad Med. 2016; 62(4): 260-263.
- Liong CC et al. Nonalcoholic Wernicke encephalopathy: an entity not to be missed! Can J Neurol Sci. 2016; 43(5): 719-20.