Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 3
Neurocysticercosis with convulsion, confusion, and hypomnesia
Guo Zhi-bao1; Yang Yi1*
1 Jiangsu Provincial Key Laboratory of Critical Care Medicine, Department of Critical Care Medicine, Zhongda Hospital, School of Medicine, Southeast University, Nanjing, 210009, Jiangsu, China.
*Corresponding Author: Yang Yi
Jiangsu Provincial Key Laboratory of Critical Care
Medicine, Department of Critical Care Medicine,
Zhongda Hospital, School of Medicine, Southeast
University, Nanjing, 210009, Jiangsu, China
Email: yiyiyang2004@163.com
Received : Dec 16, 2021
Accepted : Jan 25, 2022
Published : Feb 01, 2022
Archived : www.jcimcr.org
Copyright : © Yi Y (2022).
Abstract
Neurocysticercosis (NCC), which is typically caused by the tapeworm Taenia solium after ingesting contaminated food or water, is one of the most common parasitic diseases of the nervous system (NS) in humans, and constitutes a major public health problem for most of the developing countries. The clinical manifestations of NCC can vary from completely asymptomatic infection to death, and largely depend on the number, type, size, location of cysts, and the host’s immune response against the parasite. The NS manifestations usually include seizures, headache, intracranial hypertension, focal neurological signs and mental disorder. NCC diagnosis is usually based on neuroimaging studies (computerized tomography, magnetic resonance) and immunological tests (antibody/antigen detection in the serum and the cerebrospinal fluid). Therapeutic approaches for NCC include symptomatic therapy, antiparasitic treatment and surgery.
Keywords: neurocysticercosis; convulsion; confusion.
Citation: Zhi-bao G, Yi Y. Neurocysticercosis with convulsion, confusion, and hypomnesia. J Clin Images Med Case Rep. 2022; 3(2): 1628.
Case report
A 57-year-old man presented with an sixteen-month history of paroxysmal convulsion accompany with disturbance of consciousness. Sixteen months ago, when sleeping, he suffered from a sudden onset of left angulus oris twisting, and then talked nonsense and lost consciousness without apparent causes. The status eased after several minutes, and the same symptoms recurred two times at the second day. About ten days ago before admission, his response became slow and memory decreased significantly. He was brought to the neurology department of our hospital for treatment. His medical history included an history of fowl feeding, and there was no history of hypertension, diabetes, cardiac disease. On arrival, his vital signs were stable. Physical examination revealed clear consciousness, partial cooperation, decreased memory and computational power, poor directional force and general appearance of weakness. At the same time, his limb muscle strength, muscle tension, tendon reflexes, sensory and coordination movement were normal. Babinski and Lasègue signs were negative bilaterally.
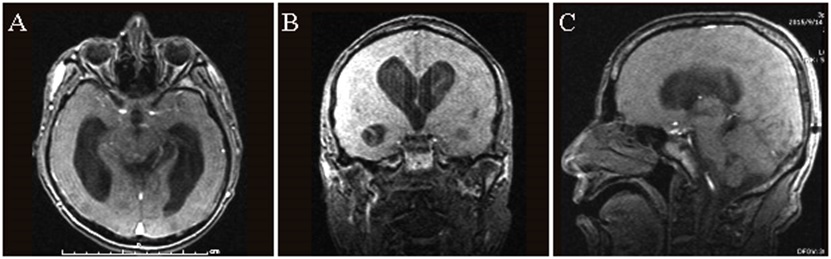
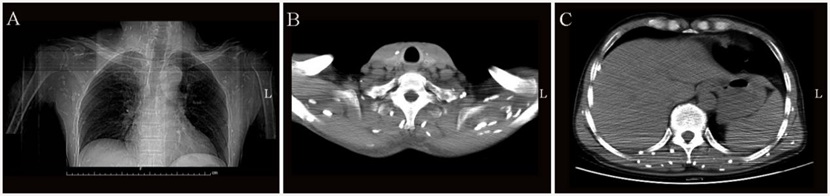
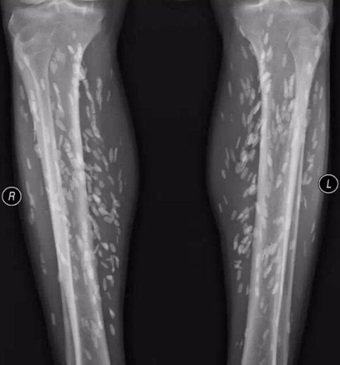
The blood test showed moderately elevated cell count for leukomonocytes and eosinophils. Cerebrospinal fluid (CSF) was clear, with increased pressure, lymphocytic pleocytosis, increased glucose and protein levels. Cysticercus-specific immunoglobin G antibodies were positive in the CSF and serum. Radiological investigations for this patient included brain magnetic resonance imaging (MRI) scan (Figure 1), cervicothoracic computed tomography (CT) scan (Figure 2), and leg X-rays scan (Figure 3). Brain MRI revealed a characteristic ‘rice grain’ appearance and severe supratentorial hydrocephalus (Figure 1). Cervico-thoracic CT showed numerous hyperdense ‘rice grain’ on the neck and chest regions (Figure 2). Plain X-rays revealed innumerable ‘rice grain’ cysticerci on the legs (Figure 3). Prior to drugs treatment, surgical external ventricular drainage was adopted to decrease intracranial pressure, and then albendazole (20 mg/kg/day) was given for 4 weeks. Other treatments included mannitol, dexamethasone and antiepileptic drugs. Accompanied by the completion of anti-cysticercus therapy, the admission abnormal neurological symptoms of this patient were improved notly. Six months after hospital discharge, the patient’s condition was fine from a return visit by telephone.
Discussion
In the last few decades, great progress has been made in diagnosis and treatment of Taenia solim infection in both developed and developing countries [1]. Many factors can be taken into account for contributing to the decline in the number of NCC cases, such as the development of economy and education, improvements in sanitation, increased awareness of the general population [1,2].However, the number of registered NCC cases seems to be growing in nonendemic countries, and many of whom are immigrants from endemic countries or international travelers to endemic area [3,4]. At present, NCC remains a major public health problem in most of developing countries and some industrialized countries. It is reported that there are about 50 million individuals who are suffering from NCC worldwide, approximately 2 million of whom having epilepsy, and more than 50000 deaths due to T. solium infection every year [5-7].
Diagnosis of NCC mainly includes clinical manifestations, serum immunology and neuroimaging. In general, canonical NCC cases can be easily diagnosed by neuroimaging of the brain. On the other hand, if the clinical presentations are atypical, neuroimaging findings are short of specificity, and immunodiagnostic tests show suboptimum predictive values, what’s more, in resource-limited areas where clinical lab and imaging techniques are often lacking, diagnosis and treatment of these NCC cases will be difficult. Generally speaking, the therapeutic strategies of NCC mainly include symptomatic therapy, antiparasitic drugs and neurosurgical procedures. It is critical that antiparasitic treatment should not be administrated before the preexisting intracranial hypertension is controlled, because antiparasitic drugs may increase cerebral edema [8]. In our present case, before albendazole was used, we decreased the increased ICP by external ventricular drainage.
In the future, socioeconomic development of endemic countries is a crucial factor for NCC eradication or tight control. Further researches are urgently needed to provide evidencebased diagnostic techniques and therapies, such as improved immunologic diagnosis and imaging techniques, and new drugs with better pharmacokinetic profiles and efficacy.
Acknowledgements: This work was supported by the Fundamental Research Funds for the Central Universities of Southeast University (2242020K40166).
References
- Medina MT, Aguilar-Estrada RL, Alvarez A, et al. Reduction in rate of epilepsy from neurocysticercosis by community interventions: the Salamá, Honduras study. Epilepsia 2011; 52: 1177-85.
- Sotelo J, Diaz-Olavarrieta C. Neurocysticercosis: changes after 25 years of medical therapy. Arch Med Res 2010; 41: 62-3.
- Serp JA, Graviss EA, Kass JS, White AC Jr. Neurocysticercosis in Houston, Texas: an update. Medicine (Baltimore). 2011; 90: 81-6.
- Sorvillo F, Wilkins P, Shafir S, Eberhard M. Public health implications of cysticercosis acquired in the United States. Emerg Infect Dis. 2011; 17: 1-6.
- Singh G, Burneo JG, Sander JW. From seizures to epilepsy and its substrates: neurocysticercosis. Epilepsia. 2013; 54: 783-92.
- Schantz PM, Cruz M, Sarti E, Pawlowski Z. Potential eradicability of taeniasis and cysticercosis. Bull Pan Am Health Organ. 1993; 27: 397-403.
- Del Brutto OH, Rajashekhar V, White Jr AC, et al. Proposed diagnostic criteria for neurocysticercosis. Neurology. 2001; 57: 177-83.
- Garcia HH, Nash TE, Del Brutto OH. Clinical symptoms, diagnosis, and treatment of neurocysticercosis. Lancet Neurol. 2014; 13: 1202-15.