Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 3
Management anesthesia in carotid artery aneurysm caused by a Behcet’s disease: A case report
Hamidreza Azizi Farsani1; Sogol Asgari2; Faranak Behnaz3*
1 Assistant professor of Anesthesiology, Shohada Tajrish hospital, Shahid Behehti University of Medical Sciences, Tehran, Iran.
2 Fellowship of Neuroanesthesiology, Shohada Tajrish hospital, Shahid Behehti University of Medical Sciences, Tehran, Iran
3 Associated professor of Anesthesiology, Shohada Tajrish hospital, Shahid Behehti University of Medical Sciences, Tehran, Iran.
*Corresponding Author: Faranak Behnaz
Associated Professor of Anesthesiology, Shohada Tajrish
hospital, Shahid Behehti University of Medical Sciences,
Tehran, Iran.
Email: faranak.behnaz@gmail.com
Received : Nov 27, 2021
Accepted : Jan 31, 2022
Published : Feb 07, 2022
Archived : www.jcimcr.org
Copyright : © Behnaz F (2022).
Abstract
Objective: Arterial manifestations of Behcet’s disease are challenging and can lead to fatal complications. One of the causes of carotid aneurysm is Behcet’s disease. Extracranial internal carotid artery aneurysms are rare. This aneurysm is rare but important because it is associated with a high risk of neur thromboembolic events, cranial nerve damage, and rupture.
Method: We describe a 19-year-old man with a history of Behcet’s disease who presented with a gradual enlargement of the right neck mass with shortness of breath when he is supine.
Result: This report examines the challenges of treating carotid aneurysms by spreading to the mediastinum in a patient with Behcet’s disease.
Conclusion: It is important to pay attention to the need for awake intubation by expanding to the mediastinum.
Keywords: management anesthesia; carotid artery; pseudoaneurysms; Behcet’s disease.
Citation: Farsani HA, Asgari S, Behnaz F. Management anesthesia in carotid artery aneurysm caused by a Behcet’s disease: A case report. J Clin Images Med Case Rep. 2022; 3(2): 1641.
Introduction
Behcet’s Disease (BD) is a chronic inflammatory disease characterized by extensive vasculitis with recurrent ulcers of the mouth and genitals, ocular symptoms, and involvement of the musculoskeletal, nervous, cardiac, pulmonary, and gastrointestinal systems. Behcet’s neurological diseases are a difficult diagnosis [1], so life-threatening neurological involvement cannot be completely ruled out. Cardiac involvement may occur in the form of endocarditis, myocarditis, pericarditis, intracardiac thrombosis, endomyocardial fibrosis, and valvular disease [2]. Therefore, after the diagnosis of Behcet’s disease, accurate cardiac evaluation should be performed for myocardial involvement, endocardial fibrosis, myocardial aneurysm, and thrombosis. Mucosal cutaneous ulcers are the most common manifestations. Planned anesthesia management for a Behcet patient with an extra cranial carotid aneurysm whose neck mass extends to the mediastinum is challenging, and by focusing on the airways, hemodynamics, bleeding control, and possible manifestations of neural neuralgia. Airway management can be difficult due to soft tissue lesions of the larynx and throat, as well as the presence of a large neck mass [3]. The disease manifests itself in the form of oral and genital ulcers, skin lesions, ear and vascular inflammation, central nervous system and gastrointestinal involvement [1,4]. Because BD is a systemic vasculitis of small and large vessels, including arteries and vessels, large vascular damage in BD patients, so-called vasculo-BD, is characterized by venous thrombosis, arterial occlusion, and aneurysms [4]. Arterial involvement has received special attention because of its significant association with mortality, as it accounts for more than a quarter of all BD deaths [3,4]. Surgical repair combined with the administration of an immunosuppressive system is recommended for peripheral arterial aneurysms, and this recommendation is basically supported by experience and evidence from experimental and observational studies. Surgical bypass has previously been a traditional choice, and its safety and efficacy have been proven to allow aneurysm rupture to survive. Behcet’s disease is a chronic recurrent vasculitis that is unknown in etiology and is unique in its ability to affect all arteries regardless of size. Usually, the known genetic factor in the pathogenesis of Behcet’s disease is the role of self-antigenic for human leukocyte-B51 antigen. Vasculitis in Behcet’s disease can cause thrombosis and bleeding complications. There are some reports in the literature about hemorrhagic complications of Behcet’s disease, such as recurrent biliary, intracranial, and pulmonary hemorrhages [5].
Reports of extra cranial carotid aneurysms are limited, and radiotherapy treatments and surgery are deferent. In both treatments, there are possibility of risk for Cranial nerve damage, vascular accidents, prolonged hospitalization and mortality. Endovascular treatments are recommended, especially in cases where the aneurysm is close to the base of the skull and the proximal and distal carotid arteries are very difficult to control. It also minimizes risks in patients undergoing neck reoperation and in patients undergoing radiotherapy to the neck. The most important problem with endovascular procedures is that the rate of reprocessing, such as restenosis, is higher than surgery. Advantages of endovascular treatment include fewer complications [7]. Extra cranial carotid aneurysms are rare lesions and make up 1% of peripheral aneurysms. The most common fundamental cause is atherosclerosis, which is seen in 37% -42% of aneurysms, followed by trauma is the second most common cause (35%-51%) [7,8]. If young patients have Extra Cranial Carotid Artery Aneurysm (ECAA), the cause of the infection, such as tuberculosis or human immunodeficiency virus, should be investigated. Other causes of collagen vascular disease include fibro muscular dysplasia, radiation, Behcet’s disease, Takayasu arthritis, or Cogan syndrome. Connective diseases that can affect the carotid arteries, including Marfan syndrome, EhlersDanlos syndrome, and osteogenesis imperfactica, can also be causes. Atherosclerotic aneurysms are more common in the elderly. The most common clinical manifestations are pulsating neck mass and localized pain [9]. The gold standard diagnostic tool for ECAA is conventional digital subtraction angiography. CT angiography is typically a diagnostic tool that provides anatomical details of the extravascular system and can be used to plan surgical procedures. Magnetic Resonance Angiography (MRA) is alternative suitable diagnostic instrument that has the lead of preventing ionizing radiation exposure and contrast. We should also check the patient for adequate cerebral circulation. This is done by digital compression of the carotid artery under neurological monitoring or it can be combined with a radiological diagnosis such as MRA to increase accuracy [8]. Conventional angiography with temporary balloon occlusion is an aggressive decision that has practical accuracy, although 10% -25% of those who passed the test still had CVA with carotid artery occlusion. 90% of patients with cerebral blood flow less than 30 ml per 100 g / h have CVA after carotid artery occlusion [10].
Case presentation
This study was approved with Ethical Committee of Shahid Beheshti University of Medical Sciences. Furthermore, informed consent was provided from the patient included.
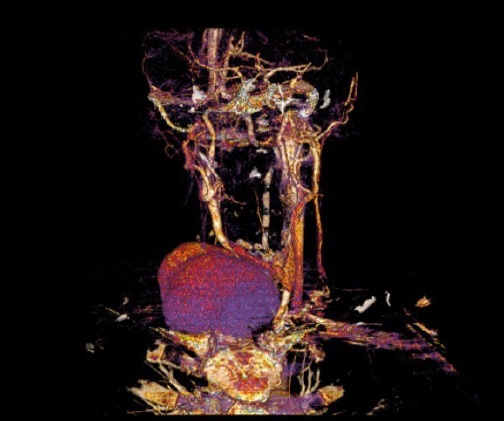
The patient was a 19-year-old man with a history of oral plague from childhood and weakness and lethargy and weight loss from one year ago, who had been suffering from hoarseness for 4 months and then noticed a right throbbing neck mass, which had increased in size. According to the patient, the cervical mass has grown significantly during the last 4 months and he has also developed shortness of breath, so that he could not tolerate sleeping on his back. During taking the history and examination of the patient, he was sitting and slightly bent forward. He has severe shortness of breath and speaks sharply. A large throbbing mass is seen on the right side of the neck, which is audible, and also causes the patient to tilt his head slightly to the opposite side and does not allow the neck to move freely. He has no history of allergies, smoking and alcohol use. The patient has been treated with prednisolone 20 mg daily for 4 months and has been treated twice with steroid pulse, cisplatin and cyclophosphamide. In the Angiography, the aneurysm is located at the site of brachiocephalic artery bypass correction (Figure 1). There is a mass of space in the neck and anterior mediastinum, which causes deviation and narrowing of the trachea before the carina. He does not tolerate the supine position and has nasal flare while breathing. On examination, skin rash is seen in the chest and abdomen. In the folds of the body and in the axillary and groin areas have scaly dermatitis. The plague is seen inside the mouth. After explaining awake intubation to the patient, the patient was intubated under local anesthesia with lidocaine spray and 0.5 mg atropine with fibropeptic with tube number 6 with a length of 42 cm (Figure 2). After confirming the location of the tube and ventilation, the patient was anesthetized with 50 micrograms of fentanyl titer, 120 mg of propofol, and anesthesia was continued with infusion of 100 macrogram/ minpropofol and 10 micrograms/min of remifentanil and 1MAC isoflurane. No intramuscular relaxant was injected. The patient’s aneurysm was clipped endo-vascular and after ensuring spontaneous and regular breathing and alertness, the patient was extubated and transferred to the ICU.
Discussion
Behcet's Disease (BD) is a multisystem disease of unknown reason. The three symptoms, originally described by Hulusi Behçet, include oral aphthous ulcers, genital ulcers, and ocular lesions. Absolute diagnosis is based on the identification of numerous clinical symptoms. Vascular involvement is considered by the development of aneurysms and obstruction of large arteries [11]. Aneurysm respond poorly to medical treatment and surgical procedure is required [12]. The risk factors of cardiovascular disease with cardiac symptoms, vascular involvement should be considered first. Since our patient had no traditional cardiovascular risk factors, coronary aneurysm was attributed to BD. Extra cranial internal carotid artery aneurysms are rare lesions and make up less than 1% of the total aneurysm [13]. Atherosclerosis is the most common cause of true aneurysm and is the leading cause in 37% to 42% of aneurysm cases [14]. In this study, the patient presented with a throbbing growing mass in the neck, which had shortness of breath while lying on its back and a pleasant sound. ECAA may present with central neurological symptoms due to cerebral embolism, although it may be associated with mass, pain, and / or local compression that causes nerve palsy [15]. Vascular surgery is often considered necessary to relieve local symptoms and reduce the risk of stroke and aneurysm rupture [16]. Both surgical and endovascular therapies have been used in recent decades. The choice of intervention methods based on the cause, location of the aneurysm and morphology of the artery as well as the professional experience of the researcher is medically qualified [14]. Open surgery was performed under general anesthesia by inserting a shunt during carotid ligation. Endovascular procedures were usually performed under conscious sedation, unless general anesthesia was required for hemodynamic instability [17]. In our case, due to the size of the mass and the effect of pressure on the airway, as well as the expansion of the aneurysm to the mediastinum, the difficulty of the airway is raised. In these cases, despite difficult airway symptoms, intubation is most appropriate. Other methods include: blind nasal, awake video laryngoscopy, awake fibrooptic intubation, or awake tracheostomy. Awake fibropeptic may have the highest reliability. Oral laryngoscopy in the presence of a large neck mass and airway obstruction is not helpful [18].
Conclusion
It is important that the anesthesiologist pays attention to the airway of these patients before surgery.
References
- Demirelli S, Degirmenci H, Inci S, Arisoy A. Cardiac manifestations in Behcet’s disease. Intractable & rare diseases research. 2015.
- Giuri PP, Gonnella GL, Catarci S, Ciancia M, Draisci G, et al. Anesthetic management of a parturient with Behcet’s disease and suspected arrhythmogenic right ventricular dysplasia. Korean journal of anesthesiology. 2020; 73: 75.
- Ali O, Nicholl P, Carruthers D, Geoghegan J, Tiwari A, et al. Multiple aneurysms and a transplanted kidney in Behçet disease. Vascular and endovascular surgery. 2017; 51: 108-110.
- Shen C, Li W, Zhang Y, Li Q, Jiao Y, et al. Outcomes of surgery for patients with Behcet’s disease causing aortic pseudoaneurysm: A shift from open surgery to endovascular repair. Clinics. 2016; 71: 302-310.
- Şan F. Spontaneous Auricular Hematoma In Behçet Disease.
- Li Z, Chang G, Yao C, Guo L, Liu Y, et al. Endovascular stenting of extracranial carotid artery aneurysm: A systematic review. European Journal of Vascular and Endovascular Surgery. 2011; 42: 419-426.
- Qiu J, Zhou W, Zhu X, Zhou W, Zeng Q, et al. Treatment of Extracranial Carotid Artery Aneurysm: Fifteen Years’ Experience at a Single Institution. Annals of Vascular Surgery. 2020; 69: 174-181.
- Attigah N, Külkens S, Zausig N, Hansmann J, Ringleb P, et al. Surgical therapy of extracranial carotid artery aneurysms: Longterm results over a 24-year period. European Journal of Vascular and Endovascular Surgery. 2009; 37: 127-133.
- Chavan R, Ichaporia N, Vhora S, Aurangabadkar K, Kamerkar D, et al. Endovascular management of internal carotid artery pseudoaneurysms: Retrospective observational study. Interdisciplinary Neurosurgery. 2021; 24: 101042.
- El Sabrout R, Cooley DA. Extracranial carotid artery aneurysms: Texas Heart Institute experience. Journal of vascular surgery. 2000; 31: 702-712.
- Gutierrez PS, Leite TN, Mangione FM. Male gender and smoking are related to single, but not to multiple, human aortic aneurysms. Cardiovascular Pathology. 2015; 24: 290-293.
- Tekin B, Özen G, Tekayev N, Gerçek Ş, Direskeneli H, et al. Acute coronary syndrome in Behcet’s disease caused by a coronary artery aneurysm and thrombosis. European journal of rheumatology. 2014; 1: 156.
- Pulathan GZ, Hemsinli D. True aneurysms of the extracranial carotid artery: An evaluation of two “giant aneurysms” and the current literature. Journal of Korean Neurosurgical Society. 2018; 61: 282.
- Chen Z, Chen L, Zhang J, Chen Y, Liu C, et al. Management of extracranial carotid artery aneurysms: A 6-year case series. Medical science monitor: International medical journal of experimental and clinical research. 2019; 25: 4933.
- Tanaka H, Yano M, Kuwabara C, Kume A, Tamura Y, et al. Massive hemoptysis due to the rupture of thoracic aortic aneurysm caused by leukemic cell infiltration in a patient with chronic myelomonocytic leukemia. Journal of clinical medicine research. 2019; 11: 145.
- Ogawa S, Yoshino M, Hara T. Extracranial carotid artery aneurysm with myeloproliferative neoplastic cell invasion. Journal of Vascular Surgery Cases and Innovative Techniques. 2020; 6: 243- 246.
- Sharma RK, Asiri AM, Yamada Y. Extracranial carotid artery aneurysm challenges in the management: A case report and review literature. 2019.
- Cathain EO, Gaffey MM. Upper Airway Obstruction. Stat Pearls [Internet]. 2020.