Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 3
The rapid disappearance of a large intracranial meningioma-like tumor: A case report
Kamil Krystkiewicz, MD2,3*; Marcin Birski, MD, PhD2; Marcin Tosik, MD, PhD3; Marcin Rudaś, MD, PhD2; Jacek Furtak, MD, PhD2; Marek Harat, MD, PhD1,2
1 Department of Neurosurgery and Neurology, Collegium Medicum in Bydgoszcz, Nicolaus Copernicus University in Torun, Torun, Poland.
2 Department of Neurosurgery, 10th Military Research Hospital, Bydgoszcz, Poland.
3 Department of Neurosurgery and Neurooncology, Copernicus Memorial Hospital, Łódź, Poland.
*Corresponding Author: Kamil Krystkiewicz
Department of Neurosurgery and Neurooncology,
Copernicus Memorial Hospital, Łódź, Poland.
Email: kamil.krystkiewicz@gmail.com
Received : Jan 31, 2022
Accepted : Feb 21, 2022
Published : Feb 28, 2022
Archived : www.jcimcr.org
Copyright : © Krystkiewicz K (2022).
Abstract
The most common “vanishing” central nervous system (CNS) tumor is a primary lymphoma. After steroid administration, patients usually experience partial or complete remission. Importantly, CNS lymphomas are almost entirely intra-axial, and the complete remission of extra-axial tumors is rarely discussed in the literature. We present a unique patient case where a large meningioma-like tumor in the left frontal area disappeared. Initially the tumor was scheduled for resection, but the tumor was absorbed within 10 days of dexamethasone administration. During the follow-up, the patient was diagnosed with multiple myeloma. This case demonstrates that hematological disease should be considered for extra-axial tumors.
Keywords: extra-axial tumor; complete remission; multiple myeloma; meningioma.
Citation: Krystkiewicz K, Birski M, Tosik M, Rudaś M, Furtak J, et al. The rapid disappearance of a large intracranial meningioma-like tumor: A case report. J Clin Images Med Case Rep. 2022; 3(2): 1699.
Case description
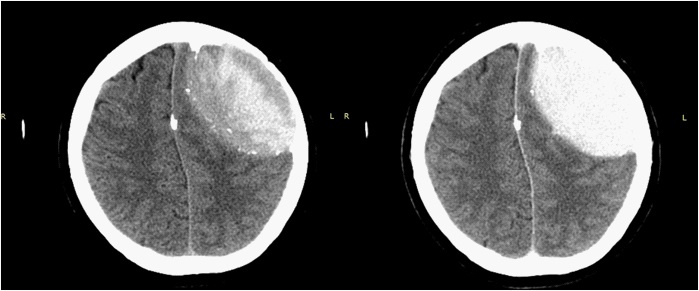
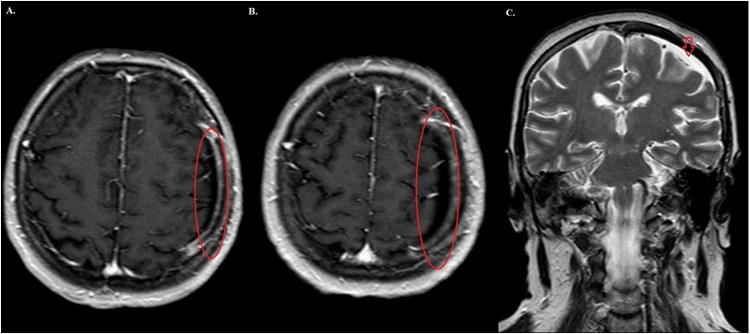
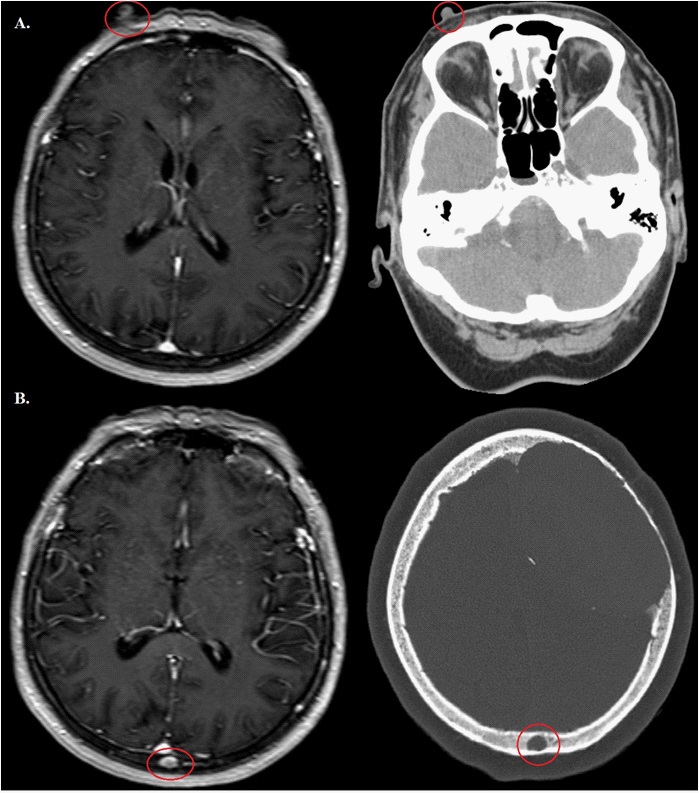
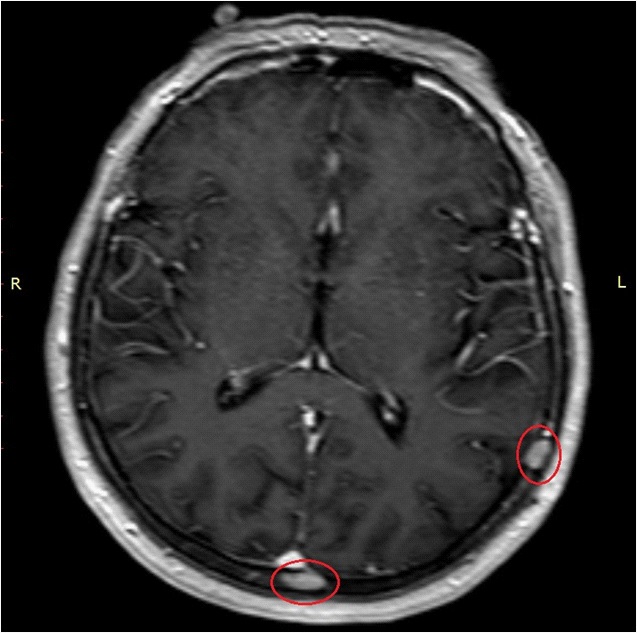
A 61-year-old right-handed woman with mild hypertension was admitted to the neurological department in other hospital with signs of right-sided hemiparesis and central paresis of the right facial nerve. The symptoms had persisted for a few weeks and the neurological examination indicated no other abnormalities. There was no trauma or oncological history. The CT scan revealed a large mass above the left frontal lobe, which caused a mass effect within the brain and thinning of the surrounding frontal bone (Figure 1). Bloodwork revealed no significant abnormalities except mild hypothyroidism. A contrast enhanced CT scan was then performed, and strong enhancement was noted (Figure 1). The initial diagnosis was a large meningioma in the left frontal area and the patient was discharged and prescribed 4 mg per day of oral dexamethasone. She was admitted to our department 11 days after the initial diagnosis and 10 days after the administration of steroids. The patient was scheduled for craniotomy and tumor resection surgery. During admission, significant clinical improvement was noted. The only neurological abnormality was subtle face asymmetry. The full preoperative MRI examination was then performed (Figure 2). Surprisingly, image analysis revealed no tumor. There was no evidence for the mass effect, no signs of brain edema, and no contrast enhancement. The only radiological finding was a linear collection of fluid over the frontal lobe, above the dura, and marked bone thinning. The remission was spectacular; therefore, the first suspicion was that an error had occurred. The patient identity was confirmed using standard protocols and radiological findings, including a skin nodule in the right frontal area and a cranial vault venous sinus in the midline of the parietal bone (Figure 3). Because of the tumor absence and the resolution of the patient symptoms in the recent radiological examination, she was discharged. It was recommended that the patient reduce the dexamethasone dosage and discontinue the drug after a few days. Hematological diagnostic work was completed including a CT scan of the thorax and abdomen, which revealed no signs of systemic lymphoma. The patient had a bone marrow biopsy and trepanobiopsy, which were unremarkable for leukemia and multiple myeloma, but led to a monoclonal gammopathy of undetermined significance (MGUS) diagnosis. Additional radiological and clinical observation were performed. A serial head MRI was done every 3 months. After one year there was no recurrence of the epidural mass above the left hemisphere of the brain. However, there was a visible enhancement in the parieto-occipital region of the skull. Initially, the structure was suspected to be a venous sinus in the skull, but it was eventually identified as another tumor that had “vanished.” The similar new lesion was located in the left parieto-temporal area. An open biopsy of the lesion in the occipital area was completed. Histopathological investigation revealed plasmocytic cells, which led to a multiple myeloma diagnosis. The patient was referred to the hematological center for further treatment.
Discussion
A large extra-axial mass that exhibits enhancement after the administration of a contrast agent suggests a meningioma diagnosis, which is the most frequent extra-axial tumor [1]. However, there are other lesions that should also be considered including dural based metastasis, hemangiopericytoma, hematological diseases (primary or secondary lymphoma), multiple myeloma, Langerhans histiocytosis, or non-neoplastic-extradural hematoma [1]. The initial diagnosis in our case was meningioma due to the intense enhancement after the contrast administration, the extra-axial location in the convexity, the slow symptom evolution, the broad base centered over the frontal bone, and the focal hyperdense areas in the mass that suggested calcifications. However, bone thinning is very uncommon in meningioma cases. Bone destruction is reported in only 3% of cases. A more frequent symptom is hyperostosis, which is found in 50% of benign cases [2]. Usually in large meningiomas there is a vascular supply to the tumor from the underlying cortex, which eliminates the arachnoid plane and causes edema. This presentation is found in 90% of tumors [3,4]. Among hematological diseases, the most accurate diagnosis is a primary CNS lymphoma, which is an extra-nodal pathology that involves CNS structures without evidence of spread into the systemic organs. The most common diagnosis is diffuse large B-cell lymphoma [5]. In most cases, lymphomas are intra-axial diseases that are supratentorial in 60% of cases. Meningeal involvement is present in 30-40% of cases, but exclusive presentation in the leptomeninges is unusual [5]. In a CT scan they are presented as hyperdense masses, usually with lytic changes in the surrounding bones. On an MRI, they present with homogenous, intense enhancement [1]. The characteristic feature for the lymphoma tumor group is their sensitivity to dexamethasone therapy. After the administration of steroids there is massive tumor cell apoptosis, which could cause a tumor to disappear within hours [6].
In our case, the symptoms developed slowly. The patient had mild facial and arm weakness. After steroid administration, she recovered rapidly. The response to dexamethasone therapy suggests lymphoma.
Because of the striking complete remission, we had no final histopathological diagnosis of the primary tumor. The patient was diagnosed with MGUS shortly after being discharged from our department. Multiple myeloma was diagnosed after 1 year of clinical and radiological observation. Therefore, with limited information, it is suspected that the disappearing tumor was also related to a hematological disease.
Dexamethasone has been used to treat multiple myeloma for years. However, the literature indicates that [7] the steroid dose during chemotherapy cycles is higher than what is used in neurosurgery. `Although, the role of the dexamethasone is known and appreciated in the hematology field, the complete disappearance of a large extra-axial tumor is still unexpected. The literature only has one documented case with a similar treatment effect [8]. Azad and colleagues describe a 63-yearold patient with back pain that was diagnosed with CT as a severe spinal canal stenosis at Th11 and L5 and was caused by an extradural mass. The patient was treated four times with 4 mg of dexamethasone. After 36 hours, a MRI was performed and revealed a significant decrease in the mass size. An open biopsy was then performed, and multiple myeloma was diagnosed. What is exceptional in our case, is that the tumor mass was mimicking an extra-axial tumor and that the huge mass disappeared entirely after a relatively small dose of dexamethasone.
Bromberg et al. [9] described a series of 12 cases where a brain tumor disappeared including partial or complete remission of an intracranial mass. In six cases, complete remission of the tumor was observed, and the patient survival was greater than 20 months. In addition, five of the 12 patients were diagnosed with primary CNS lymphoma. One patient from the CNS lymphoma group experienced complete remission. Tumor recurrence in entire cohort was present after 1 to 24 months and five patients died between 4 to 11 months. Notably, all of the lymphomas were intra-axial. There were no extra-axial tumor cases, which was the tumor location in the patient case we presented. Furthermore, our patient had complete and rapid remission for 1 year. The tumor location in combination with the remission rate makes our case exceptional and unique when compared to the literature.
Conclusions
The current approach using direct, preoperative MRI prior to planned surgery for some specific extra-axial tumors may be beneficial to prevent unnecessary surgeries. Furthermore, even in situations where extra-axial neoplasms are present, the hematological disease should be considered during the initial diagnosis, and the administration of steroids before the final histopathological diagnosis should be carefully considered.
Declarations
Acknowledgments: The authors received no financial support for the research, authorship, and/or publication of this article.
Declaration of interest statement: The authors report no conflict of interest.
References
- Rapalino O, Smirniotopoulos JG. Extra-axial brain tumors. Neuroimaging Part I. 2016; 275-291.
- Drevelegas A. Extra-axial brain tumors. Eur Radiol. 2005; 15: 453-467.
- Gasparetto EL, Leite Cda C, Lucato LT et al. Intracranial meningiomas: magnetic resonance imaging findings in 78 cases. Arq Neuropsiquiatr. 2007; 65: 610-614.
- Hou J, Kshettry VR, Selman WR, Bambakidis NC. Peritumoral brain edema in intracranial meningiomas: the emergence of vascular endothelial growth factor–directed therapy. Neurosurgical Focus. 2013; 35(6).
- Louis DN et al., International Agency for Research on Cancer, World Health Organization. WHO classification of tumors of the central nervous system. 2016. International Agency for Research on Cancer, Lyon.
- Deckert M, Engert A, Bruck W, Ferreri AJ, Finke J, lllerhaus G, et al. Modern concepts in the biology, diagnosis, differential diagnosis and treatment of primary central nervous system lymphoma. Leukemia. 2011; 25(12): 1797-807.
- Burwick N, Sharma S. Glucocorticoids in multiple myeloma: past, present, and future. Annals of Hematology. 2018; 98(1):19-28.
- Azad A, Tafreshi A, Liew MS, Yap LP. “Vanishing” spinal cord compression in myeloma: dramatic and rapid response to dexamethasone monotherapy. The Spine Journal. 2013; 13(5): 588- 589.
- Bromberg JEC, Siemers MD, Taphoorn MJB. Is a “vanishing tumor” always a lymphoma? Neurology. 2002; 59(5): 762-764.