Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 3
Epstein-Barr virus-associated lymphoproliferative disorder of donor origin after heart transplantation
Anush Barkhudaryan1,2; Otmar Pfister1,3; Beatrice Drexler4; Christian Mueller1,3; Qian Zhou3,5*
1 Cardiovascular Research Institute Basel, Basel, Switzerland
2 Department of Cardiology, Clinic of General and Invasive Cardiology, University Hospital № 1, Yerevan State Medical University, Yerevan, Armenia.
3 Division of Cardiology, Department of Internal Medicine, University Hospital Basel, Basel, Switzerland.
4 Division of Hematology, Department of Internal Medicine, University Hospital Basel, Basel, Switzerland.
5 Department of Cardiology and Angiology I, University Heart Center Freiburg – Bad Krozingen, University of Freiburg, Freiburg, Germany
*Corresponding Author: Qian Zhou
Department of Cardiology, University Hospital Basel
Petersgraben 4, CH-4031 Basel, Switzerland
Email: qian.zhou@usb.ch
Received : Feb 02, 2022
Accepted : Feb 23, 2022
Published : Mar 02, 2022
Archived : www.jcimcr.org
Copyright : © Zhou Q (2022).
Abstract
Post-Transplant Lymphoproliferative Disorder (PTLD) represents a group of lymphomas, which may develop after solid organ transplantation and decrease the survival of transplant recipients. The main challenge of treatment is to achieve disease remission by avoiding the risk of allograft rejection. This report describes a successful treatment of PTLD in an adult patient who underwent allogeneic stem cell transplantation as a child and cardiac transplantation as a young adult. We present the case of a 33-year-old female, who was diagnosed with a Diffuse Large B-Cell Lymphoma (DLBCL) triggered by Epstein - Barr virus (EBV) 8 months after receiving orthotopic heart transplantation from an EBV-positive donor. The patient was treated with R-CHOP chemotherapy followed by maintenance therapy with rituximab, resulting in complete morphologic and metabolic remission of the lymphoma. The echocardiographic examinations and routine endomyocardial biopsies performed during and after chemotherapy did not reveal any signs of cardiac allograft rejection. The patient was asymptomatic on Heart Failure (HF) therapy and continued to remain in complete remission after the cancer treatment. This case underlines the importance of timely surveillance and treatment of seronegative patients after receiving EBV-positive donor organs.
Keywords: post-transplant lymphoproliferative disorder; EpsteinBarr virus; immunosuppression; cardiac transplantation; chemotherapy
Abbreviations: ACE: Angiotensin-Converting Enzyme; CMV: Cytomegalovirus; CRP: C-Reactive Protein; CT: Computed Tomography; DLBCL: Diffuse Large B-Cell Lymphoma; EBV: Epstein-Barr Virus; 18F-FDG PET-CT: 18F-fluorodeoxyglucose positron emission tomography with computed tomography; HF: Heart Failure; HLA: Human Leukocyte Antigen; hs-cTnT: High-Sensitive Cardiac Troponin T; LV: Left Ventricle; LVEF: Left Ventricular Ejection Fraction; mTOR: Mammalian Target Of Rapamycin; NT-proBNP: N-Terminal Pro B-Type Natriuretic Peptide; PTLD: Post-Transplant Lymphoproliferative Disorder.
Citation: Barkhudaryan A, Pfister O, Drexler B, Mueller C, Zhou Q. Epstein-Barr virus-associated lymphoproliferative disorder of donor origin after heart transplantation. J Clin Images Med Case Rep. 2022; 3(3): 1704.
Introduction
Heart transplantation is considered a treatment option for patients with advanced Heart Failure (HF) who remain irresponsive to optimal medical therapy [1]. The survival following heart transplantation has improved over the last two decades with the introduction of immunosuppressive therapy [2]. However, cancer remains the most frequent cause of death five years after heart transplantation [3,4]. Post-Transplant Lymphoproliferative Disorder (PTLD) is one of the most important malignancies after solid organ transplantation. It comprises a group of heterogeneous diseases, ranging from benign hyperplasia to aggressive lymphomas [5] and is associated with an EpsteinBarr Virus (EBV) infection in more than 70% of cases [6,7]. The treatment of this disease requires an individual approach, and a variety of treatment strategies, including chemotherapy and adoptive immunotherapy, have been proposed. We report the case of an EBV-seronegative patient who developed PTLD after heart transplantation with an EBV-positive organ.
Case presentation
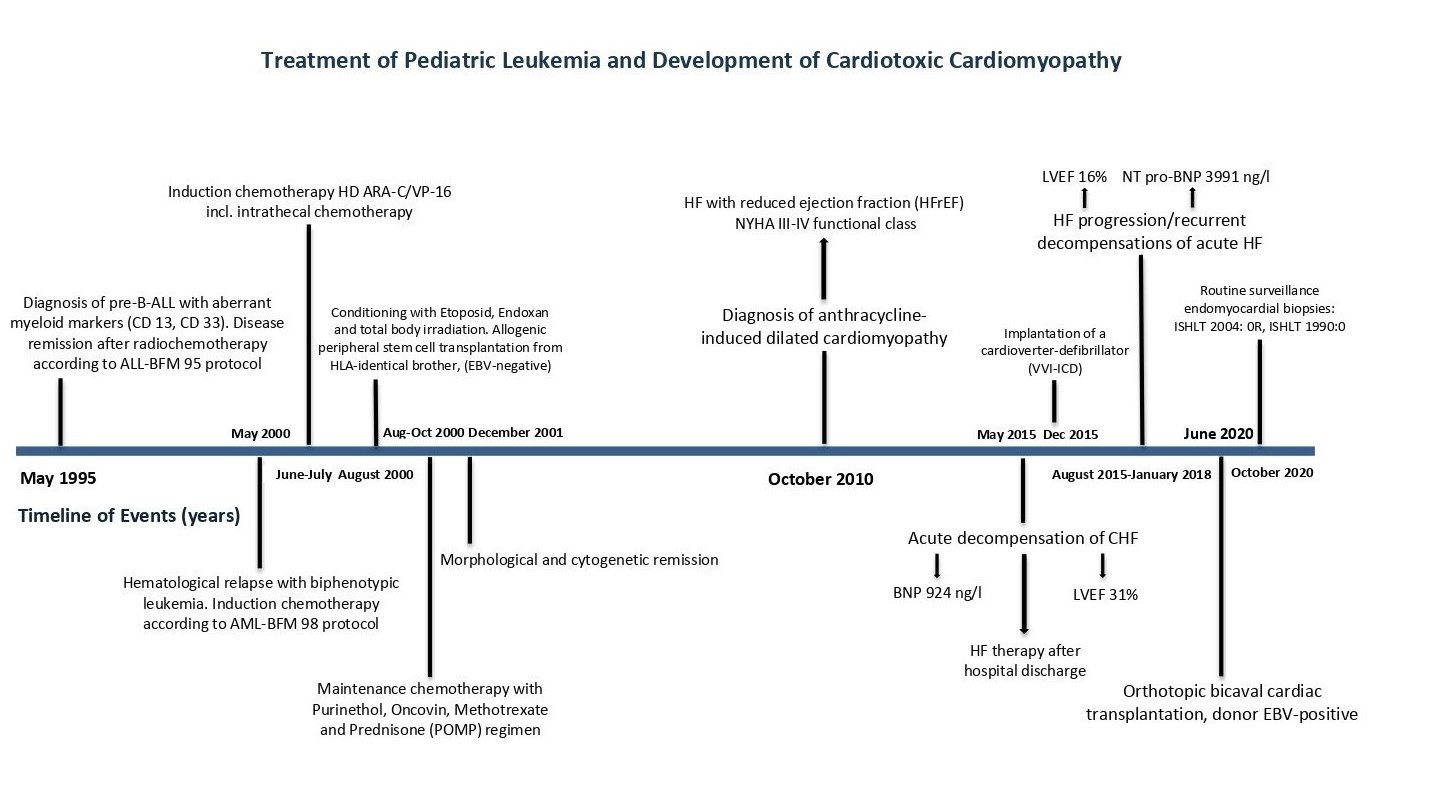
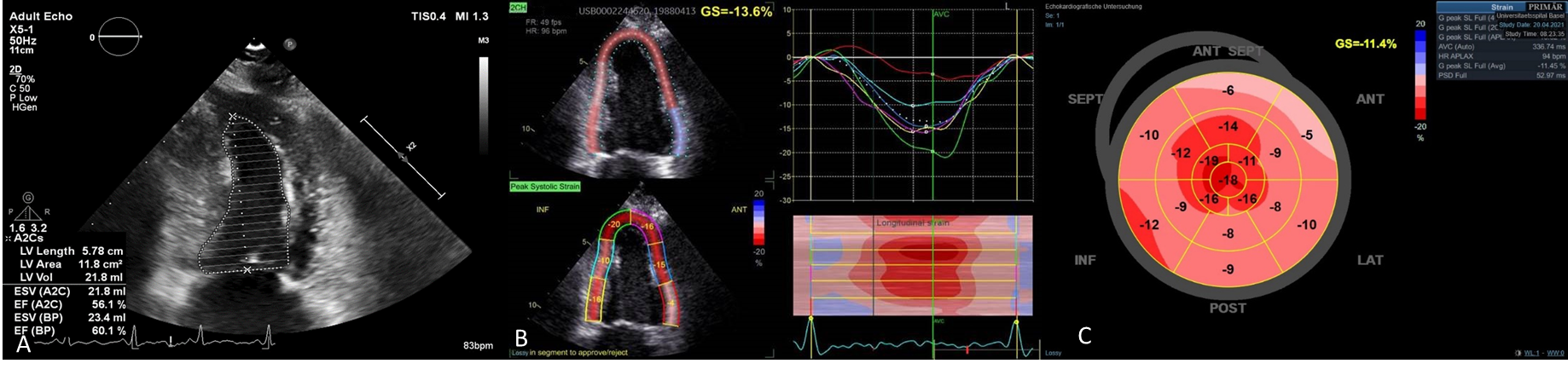
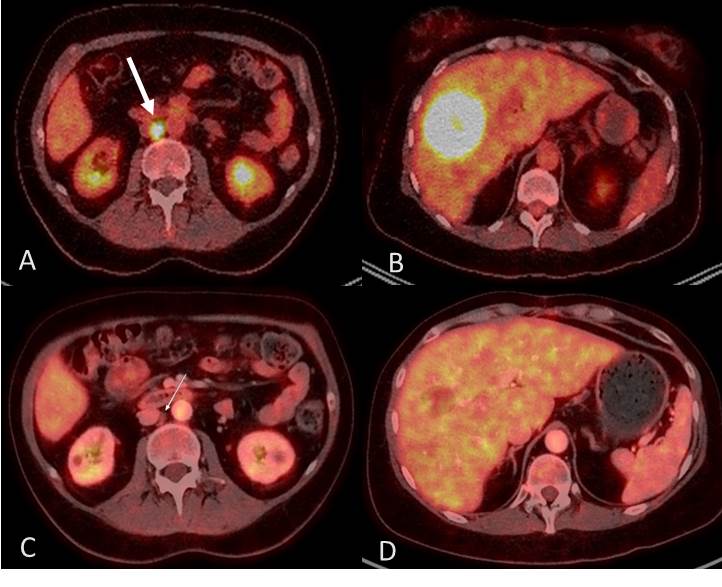
A 33-year-old female presented with symptoms of discomfort in the abdomen, intermittent nausea, fatigue, and fever for a week. Physical examination was unremarkable. The patient reported a complex medical history. She had been successfully treated for a precursor B-cell acute lymphoblastic leukemia as a child and received allogenic peripheral stem cell transplantation from her Human Leukocyte Antigen (HLA) identical brother at the age of 12 due to disease relapse. She developed chemotoxic cardiomyopathy 10 years later and received an orthotopic bicaval cardiac transplantation in 2020 due to end-stage HF (Figure 1). She was EBV-seronegative at the time of transplantation, but received an EBV-positive organ followed by a preemptive treatment with valganciclovir due to the early reactivation of Cytomegalovirus (CMV) infection. Immunosuppressive therapy consisted of mycophenolate, tacrolimus and prednisone. Routine surveillance endomyocardial biopsies revealed no evidence of cardiac allograft rejection. Laboratory analysis upon admission was as follows: hemoglobin 109 g/l, C-Reactive Protein (CRP) 14.8 mg/l, creatinine 117 µmol/l, as well as a highly elevated EBV titer (2.83444e+06 GEq/ml). The transthoracic echocardiography demonstrated normal cardiac allograft function (Figure 2A). Computed Tomography (CT) scan revealed multiple lesions in the liver and lung lobes. Histology of the liver lesion confirmed the presence of a Diffuse Large B-Cell Lymphoma (DLBCL). For staging of the disease, 18F-Fluorodeoxyglucose Positron Emission Tomography with Computed Tomography ( 18F-FDG PET-CT) scan was performed which revealed hypermetabolic thoracic and abdominal lymphadenopathy (Figure 3A,B). Due to the high tumor load, the patient received four cycles of first-line chemotherapy according to the R-CHOP regimen, and was then treated with an anti-CD20 monoclonal antibody rituximab. In addition, the immunosuppression has been reduced before and after initiation of chemotherapy. Due to its antiproliferative effect, mycophenolate was replaced by everolimus, but was changed back to mycophenolate due to severe hypertriglyceridemia.
This treatment resulted in a decrease in EBV load to 17300 GEq/ml, with no replication of the virus detected a week after the last assessment. The follow-up 18F-FDG PET-CT scan after three cycles of chemotherapy revealed almost complete metabolic and morphological remission of the intense hypermetabolic manifestations of PTLD (Figure 3C,D). Furthermore, after 3 cycles of rituximab treatment and 7 months after the diagnosis of DLBCL, follow-up 18F-FDG PET-CT scan demonstrated complete remission of the disease and EPV-PCR remained negative. However, due to the need for a long-term immunosuppression after heart transplantation, the patient remained at a high risk for relapse of the lymphoma. Therefore, the maintenance therapy with rituximab was initiated to improve the long-term outcome which was, however, discontinued after three doses due to impaired Left Ventricular (LV) function. While DLBCL was successfully treated, the patient unfortunately developed chemotoxic cardiomyopathy: Left Ventricular Ejection Fraction (LVEF) declined to 40% and a reduction in peak longitudinal systolic strain was observed (Figure 2B,C). In line with the echocardiography finding, a transient increase in the levels of high-sensitive cardiac troponin T (hs-cTnT) (peak 114 ng/l) and N-Terminal Pro B-Type Natriuretic Peptide (NT-proBNP) (peak 1553 ng/l) was noticed. The patient received HF therapy with an AngiotensinConverting Enzyme (ACE) inhibitor and β-blocker. She remained in complete remission after receiving three doses of maintenance treatment with rituximab in the ambulatory setting.
Discussion
Over the past decade, survival of patients after heart transplantation has improved due to immunosuppressive therapy, prophylaxis of infectious diseases and postoperative surveillance [8]. However, the development of cancer remains a complication associated with increased mortality [4]. PTLD occurs with an incidence of 2% to 10% in heart transplant recipients [9]. In particular, EBV-negative patients who receive an organ transplant from an EBV-seropositive donor are at increased risk for developing the disease [10] with the primary viral infection usually related to the early forms of PTLD developing during the first year after transplantation [9]. The most common histological form of the disease is considered to be CD20-positive DLBCL [11]. The patient in our case developed PTLD eight months after being transplanted with an EBV-positive heart. The chemotherapy was rapidly initiated. In addition, we replaced mycophenolate with everolimus, a Mammalian Target of Rapamycin (mTOR) inhibitor, due to its immunosuppressive and anti-proliferative effects [12]. Recent clinical studies have shown the efficacy of everolimus in the prevention and treatment of cancer after solid organ transplantation [13,14]. Furthermore, the preemptive therapy with valganciclovir may have also contributed to the decrease in the level of EBV viremia [15]. Thus, under modified immunosuppression, antiviral treatment, chemotherapy and rituximab, tumor regression was observed in our patient.
An important contributing factor to the development of PTLD is a long-term post-transplant immunosuppression which may decrease the virus-specific cytotoxic T-cell response [16]. Therefore, the risks of EBV reactivation and relapse of the lymphoma remain high in this patient cohort. The treatment with rituximab may decrease the risk of cancer development by eradicating EBV-infected B lymphocytes [17]. Moreover, this therapy lacks the toxicity and high mortality risk associated with chemotherapy. Choquet et al. have previously demonstrated the efficacy of rituximab in the treatment of EBV infection in heart transplant recipients [18]. In our study, this medication resulted in a complete remission of DLBCL. However, the patient did not receive the complete four doses of rituximab due to the presence of LV dysfunction. No sign of cardiac allograft rejection was observed in our study patient.
This case illustrated the treatment of cancer before and after orthotopic heart transplantation by an individualized therapeutic approach. Previous reports have described late forms of the disease and mainly in children after cardiac transplantation [19,20]. In contrast, cases of early EBV-positive PTLD in young adults after this operation are rarely reported in medical literature. Senechal et al. have shown complete remission of CD20- positive PTLD after rituximab monotherapy [21]. The authors of another study described a successful treatment of DLBCL by surgery, reduced immunosuppression and chemotherapy [22]. To the best of our knowledge, this is an original case report describing a unique treatment implemented in a cancer survivor who underwent heart transplantation due to advanced HF induced by prior cardiotoxic chemotherapy.
Conclusion
The adjusted anticancer treatment in a young adult resulted in complete remission seven months after the diagnosis of DLBCL. The clinical outcome of PTLD is poor with an overall mortality rate above 50% [23]. Although the disease prognosis remains uncertain, we hope that this treatment strategy will help our patient to stay in remission. This case highlighted the increased risk of development of malignancy associated with an EBV infection in patients receiving solid organ transplantation, as well as the clinical significance of their monitoring afterwards. Moreover, it has demonstrated that adjuvant immunotherapy with rituximab may be an effective therapeutic approach to prevent relapse of the disease and enhance survival in patients with cancer.
Declarations
Ethics approval: Not applicable.
Consent for publication: A written informed consent was obtained from the patient for publication of this case report.
Availability of data and materials: The data analyzed during this study are available from the corresponding author.
Conflict of interest: The authors declare that they have no competing interests.
Funding: A.B. was supported by the Swiss Government Postdoctoral Scholarship.
Authors’ contributions: QZ and AB contributed to the design, data interpretation and writing of the manuscript. QZ, OP and BD were involved in the treatment of the study patient and commented on previous versions of the manuscript. CM critically revised the original version of the manuscript. All authors read and approved the final manuscript.
References
- Hayes Jr D, Tumin D, Foraker RE, Tobias JD. Posttransplant lymphoproliferative disease and survival in adult heart transplant recipients. J Cardiol. 2017; 69: 144-148.
- Asleh R, Clavell AL, Pereira NL, et al. Incidence of malignancies in patients treated with sirolimus following heart transplantation. J Am Coll Cardiol. 2019; 73: 2676-2688.
- Engels EA, Pfeiffer RM, Fraumeni JF, et al. Spectrum of cancer risk among US solid organ transplant recipients. JAMA. 2011; 306: 1891-1901.
- Jäämaa Holmberg S, Salmela B, Lemström K, Pukkala E, Lommi J, et al. Cancer incidence and mortality after heart transplantation–A population-based national cohort study. Acta Oncol. 2019; 58: 859-863.
- Ligeti K, Müller L, Müller Tidow C, Weber T. Risk factors, diagnosis, and management of posttransplant lymphoproliferative disorder: improving patient outcomes with a multidisciplinary treatment approach. Transplant Research and Risk Management. 2017; 9: 1-14.
- San Juan R, Comoli P, Caillard S, Moulin B, Hirsch HH, et al. ESCMID Study Group of Infection in Compromised Hosts. EpsteinBarr-virus related post-transplant lymphoproliferative disorder in solid organ transplant recipients. Clin Microbiol Infect. 2014; 20: 109-118.
- Nourse JP, Jones K, Gandhi MK. Epstein-Barr virus-related posttransplant lymphoproliferative disorders: Pathogenetic insights for targeted therapy. Am J Transplant. 2011; 11: 888-895.
- Giuliano K, Canner JK, Etchill E, et al. High rates of de novo malignancy compromise post‐heart transplantation survival. J Card Surg. 2021; 36: 1401-1410.
- Petrara MR, Giunco S, Serraino D, Dolcetti R, De Rossi A. Posttransplant lymphoproliferative disorders: from epidemiology to pathogenesis-driven treatment. Cancer Lett. 2015; 369: 37-44.
- Al-Mansour Z, Nelson BP, Evens AM. Post-transplant lymphoproliferative disease (PTLD): Risk factors, diagnosis, and current treatment strategies. Curr Hematol Malig Rep. 2013; 8: 173-183.
- Eyre TA, Caillard S, Finel H, et al. Autologous stem cell transplantation for post-transplant lymphoproliferative disorders after solid organ transplantation: A retrospective analysis from the Lymphoma Working Party of the EBMT. Bone Marrow Transplant. 2021; 56: 2118-2124.
- Zuckermann A, Manito N, Epailly E, et al. Multidisciplinary insights on clinical guidance for the use of proliferation signal inhibitors in heart transplantation. J Heart Lung Transplant. 2008; 27: 141-149.
- Holdaas H, De Simone P, Zuckermann A. Everolimus and malignancy after solid organ transplantation: A clinical update. J Transplant. 2016; 2016: 4369574.
- Saber-Moghaddam N, Nomani H, Sahebkar A, Johnston TP, Mohammadpour AH. The change of immunosuppressive regimen from calcineurin inhibitors to Mammalian Target of Rapamycin (mTOR) inhibitors and its effect on malignancy following heart transplantation. Int Immunopharmacol. 2019; 69: 150-158.
- Yager JE, Magaret AS, Kuntz SR, et al. Valganciclovir for the Suppression of Epstein-Barr Virus Replication. J Infect Dis. 2017; 216: 198-202.
- Claeys E, Vermeire K. Immunosuppressive drugs in organ transplantation to prevent allograft rejection: Mode of action and side effects. J Immunological Sci. 2019; 3: 14-21.
- Nijland ML, Kersten MJ, Pals ST, Bemelman FJ, Ten Berge IJ. Epstein-Barr Virus–Positive Posttransplant Lymphoproliferative Disease After Solid Organ Transplantation: Pathogenesis, Clinical Manifestations, Diagnosis, and Management. Transplant Direct. 2016; 2: e48.
- Choquet S, Varnous S, Deback C, Golmard JL, Leblond V. Adapted treatment of Epstein–Barr virus infection to prevent posttransplantlymphoproliferative disorder after heart transplantation. Am J Transplant. 2014; 14: 857-866.
- Huang Q, Yang T, Jin X, Ni X, Qi H, Yan Z. Remission of late-onset post-heart transplantation lymphoproliferative disorder following treatment with rituximab and modified mini-CHOP chemotherapy: A case report. Exp Ther Med. 2016; 12: 262-266.
- Kusuki S, Hashii Y, Fukushima N, et al. Pediatric post-transplant diffuse large B cell lymphoma after cardiac transplantation. Int J Hematol. 2009; 89: 209-213.
- Senechal M, Demers S, Cantin B, et al. Usefulness and limitations of rituximab in managing patients with lymphoproliferative disorder after heart transplantation. Exp Clin Transplant. 2012; 10: 513-518.
- Nitta D, Kinugawa K, Imamura T, et al. How Should We Treat Early Post-Transplant Lymphoproliferative Disease After Heart Transplantation? A Case Report. Int Heart J. 2015; 56: 676-678.
- Ghobrial IM, Habermann TM, Maurer MJ, et al. Prognostic analysis for survival in adult solid organ transplant recipients with post-transplantation lymphoproliferative disorders. J Clin Oncol. 2005; 23: 7574-7582