Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Short Report - Open Access, Volume 3
Is that a berry?
Hala A1*; Stephen E2; Sameer R3; Mohammed M4
1 First year, Orthopedic Resident, Oman Medical Specialty Board, Muscat, Oman.
2 Senior Consultant, Vascular Surgery, Sultan Qaboos University Hospital, Muscat, Oman.
3 Consultant, Radiology, Sultan Qaboos University Hospital, Muscat, Oman
4 Consultant, Orthopedics, Sultan Qaboos University Hospital, Muscat, Oman.
*Corresponding Author: Hala Alisaii
First year, Orthopedic Resident, Oman Medical
Specialty Board, Muscat, Oman.
Email: 8hala2018@gmail.com
Received : Jan 29, 2022
Accepted : Feb 24, 2022
Published : Mar 03, 2022
Archived : www.jcimcr.org
Copyright : © Alisaii H (2022).
Citation: Hala A, Stephen E, Sameer R, Mohammed M. Is that a berry?. J Clin Images Med Case Rep. 2022; 3(3): 1709.
Case presentation
A 55-year-old male, smoker, with no other comorbidities, was referred to our hospital with signs and symptoms of acute left lower limb ischemia, which was not salvageable. He underwent an Above Knee Amputation [AKA] to avoid sepsis and relieve pain. He was discharged on therapeutic dose of Rivaroxaban as he had a past history of unprovoked venous thromboembolism.
Post AKA, his stump wound was healthy. Two weeks post-op he reported to the emergency with history of swelling and pain on the stump edge. Upon examination, there was 2 by 2 cm collection on the lateral edge of his stump wound. Under local anesthesia, the collection was drained. This was thought to be an infected hematoma. He started regular physiotherapy once the incision site healed.
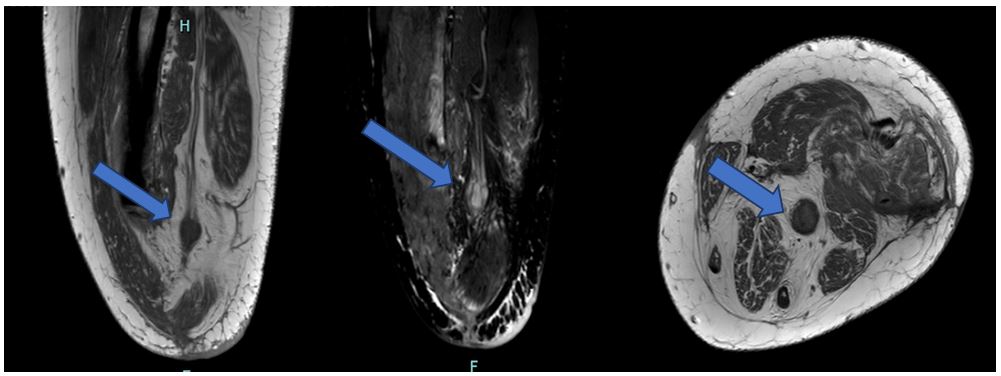
20 weeks later the patient presented with mid stump wound redness and pain and was attributed to the use of a recently acquired prosthesis. He received a course of antibiotics and an MRI was done to rule out an underlying collection, hematoma or osteomyelitis. Imaging revealed a well defined bulb like mass lesion demonstrating the fascicular sign [1] on T1WI and hyperintense signal on T2 WI at the end of sciatic nerve course - a “stump neuroma”.
Discussion
Neuroma is a non-neoplastic proliferation that occurs at the end of an injured nerve and is usually seen 1–12 months after amputation. It usually develops as an injured nerve starts to heal in an uncontrolled manner, resulting in a lump of unorganized axon fibers and non-neural tissue growth [2,3].
Two types of post-amputation neuromas are encountered. A terminal neuroma originates at the end of the severed nerve, which represents a normal pattern of healing of the nerve and is often asymptomatic, as seen in our case. The other is a spindle neuroma which is localized in the nerve and is away from the severed nerve ending, representing the response of a peripheral nerve subjected to microtrauma due to stretching or compression by the localized scar tissue [2].
Up to 60% of patients with a nerve injury can develop a painful neuroma [4]. The diagnosis of a neuroma relies on history and examination. When there is uncertainty, X-rays can be taken to rule out bone injury and malignant change as a cause of pain. Ultrasound, CT and MRI will show a well-defined soft tissue mass but are rarely necessary investigation [3].
Surgical prophylaxis against terminal neuroma, according to which technique is used is divided into the categories of - end closure (two proximal severed nerves are coapted, or a single nerve is split and coapted to itself, transposition with implantation (in which terminal nerves are buried into muscle, bone, or fascia), neurorrhaphy (two proximal severed nerves are coapted, or a single nerve is split and coapted to itself), and alternate target reinnervation like Targeted Muscle Reinnervation (TMR) and Targeted Nerve Implantation (TNI) [5].
References
- Murphey MD, Smith WS, Smith SE, Kransdorf MJ, Temple HT, et al. From the archives of the AFIP. Imaging of musculoskeletal neurogenic tumors: Radiologic-pathologic correlation. Radiographics. 1999; 19: 1253-1280.
- Henrot MD, Stines MD, Walter MD, Martinet MD, Paysant MD, et al. Imaging of the painful lower limb stump. Radiographics : A review publication of the Radiological Society of North America, Inc, 20 Spec No, S219–S235. https://doi.org/10.1148/radiographics.20.suppl_1.g00oc14s219
- Zabaglo M, Dreyer MA. Neuroma. [Updated 2021 Aug 11]. In: StatPearls [Internet]. Treasure Island (FL): Stat Pearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/ books/NBK549838/ [ Accessed on 1st October 2021]
- Peters BR, Russo SA, West JM, Moore AM, Schulz SA, et al. Targeted muscle reinnervation for the management of pain in the setting of major limb amputation. SAGE Open Medicine. 2020; 8: 2050312120959180.
- Bogdasarian RN, Cai SB, Tran BNN, Ignatiuk A, Lee ES, et al. Surgical prevention of terminal neuroma and phantom limb pain: A literature review. Arch Plast Surg. 2021; 48: 310-322.